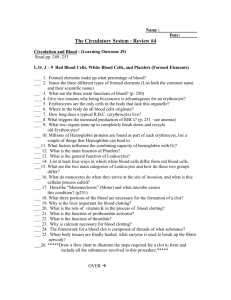
19. The Cardiovascular System: The Blood
advertisement

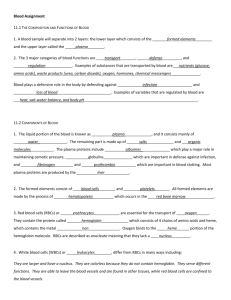
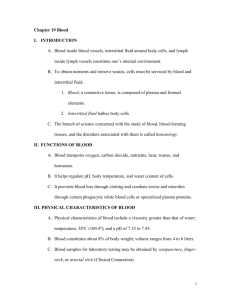
Chapter 19 THE CARDIOVASCULAR SYSTEM: BLOOD I. INTRODUCTION A. Blood inside blood vessels, interstitial fluid around body cells, and lymph inside lymph vessels constitute one’s internal environment. B. To obtain nutrients and remove wastes, cells must be serviced by blood and interstitial fluid. 1. Blood, a connective tissue, is composed of plasma and formed elements. 2. Interstitial fluid bathes body cells. C. The branch of science concerned with the study of blood, blood-forming tissues, and the disorders associated with them is called hematology. II. FUNCTIONS OF BLOOD A. Blood transports oxygen, carbon dioxide, nutrients, heat, wastes, and hormones. B. It helps regulate pH, body temperature, and water content of cells. C. It prevents blood loss through clotting and combats toxins and microbes through certain phagocytic white blood cells or specialized plasma proteins. III. PHYSICAL CHARACTERISTICS OF BLOOD A. Physical characteristics of blood include a viscosity greater than that of water. B. temperature, 38oC (100.4oF). C. pH of 7.35 to 7.45. D. Blood constitutes about 8% of body weight; volume ranges from 4 to 5 liters in females and 5-6 liters in males. E. Blood samples for laboratory testing may be obtained by venipuncture, finger-stick, or arterial stick. IV. COMPONENTS OF BLOOD A. Blood consists of 55% plasma and 45% formed elements. B. Blood plasma consists of 91.5% water and 8.5% solutes. 1 1. Principal solutes include proteins (albumins, globulins, fibrinogen), nutrients, enzymes, hormones, respiratory gases, electrolytes, and waste products. a. Proteins 1)Blood plasma is a complex mix of proteins, enzymes, nutrients, wastes, hormones, and gases. 2)The three major types of plasma proteins play a variety of roles, including defense, clotting, and transport. a)Albumins are the smallest and most abundant of the plasma proteins. They make major contributions to viscosity and osmolarity, and changes in their abundance can influence blood pressure, flow, and fluid balance. They transport some lipid-soluble hormones. b)Globulins are divided into three subclasses: alpha, beta, and gamma globulins. 1)Alpha Globulins. Include high density lipoproteins (HDLs) as well as lipid soluble hormone trasporters such as thyroxine-binding globulin, cortisolbinding globuliln, and steroid-binding hormones. 2)Beta Globulins. Include low density lipoproteins (LDLs) and very low density lipoproteins (VLDLs) and metaloproteins such as transferring. 3)Gamma Globulins. Antibodies c)Fibrinogen is the soluble precursor of fibrin, a protein involved in clotting. d)The liver produces all plasma proteins with the exception of gamma globulins, which are produced by cells of the immune system. b. Nonprotein Nitrogenous Substances 1)Nitrogenous substances in the blood are the amino acids from the digestive tract and nitrogenous wastes, the toxic end products of catabolism. 2 c. Nutrients 2)Various nutrients absorbed by the digestive tract are transported by plasma. 3)These include glucose, amino acids, fats, cholesterol, phospholipids, vitamins, and minerals. d. Gases 1)Plasma transports a portion of the carbon dioxide and oxygen circulated by the blood, and also carries dissolved nitrogen. e. Electrolytes 1)The plasma electrolytes and their concentrations. 2)Of these, sodium exerts a major influence on the blood osmolarity and therefore on blood volume and pressure. C. Formed Elements 1. The formed elements in blood include erythrocytes (red blood cells or RBCs), leukocytes (white blood cells or WBCs), and thrombocytes (platelets). V. FORMATION OF BLOOD CELLS A. Blood cells are formed from pluripotent hematopoietic stem cells. 1. Originating from the pluripotent stem cells are the myeloid stem cells and lymphoid stem cells. a. Myeloid stem cells give rise to RBCs, platelets, and all WBCs except for lymphocytes. b. Lymphoid stem cells give rise to lymphocytes. 2. Myeloid stem cells differentiate into progenitor cells or precursor cells (blast cells) which will develop into the actual formed elements of blood. 3. Lymphoid stem cells differentiate into pre-B and prothymocytes which develop into Blymphocytes and T-lymphocytes, respectively. 3 B. Hemopoiesis is the production of formed elements of the blood. 1. Hemopoiesis begins in the embryonic yolk sac. Here, primitive stem cells are produced that colonize fetal bone marrow, spleen, thymus, and liver tissue and begin the production of blood cells. See diagram. 2. Beyond infancy, almost all formed elements are produced by myeloid hemopoiesis in the red bone marrow, and lymphocytes are produced in lymphoid organs by lymphoid hemopoiesis. 3. All hemopoiesis begins with hemocytoblasts. They are pluripotent, and differentiation is determined by production of the various hormone receptors (now committed cells). C. Erythrocyte Production 1.Erythropoiesis produces erythrocytes at the rate of 2.5 million cells per second. 2.The proerythroblast (a committed cell) receives erythropoietin, which stimulates it to become an erythroblast. 3.Erythroblasts multiply and synthesize hemoglobin, their nuclei degenerate, and the cells are then called reticulocytes. 4.Once reticulocytes leave the bone marrow and the remaining ER disappears, they are considered mature erythrocytes. 5.RBC count is managed by negative feedback. Hypoxia in tissues, or hypoxemia, triggers secretion of more erythropoietin from the kidneys, and red blood cell production increases. 6.One of the nutritional requirements for erythropoiesis is iron, which can only be absorbed in its ferrous (Fe2+) state in the small intestine. Ferrous ions bind to gastroferritin produced by the stomach and travel to the small intestine. They are absorbed into the blood and bound to a plasma protein called transferrin. 7.Transferrin carries the iron to bone marrow, liver, and other tissues. Bone marrow uses the iron to make hemoglobin; muscle cells use it for myoglobin; and other cells use it to make cytochromes. 8.The liver stores excess iron in the form of ferritin. 4 9.Other nutrient requirements include folic acid and vitamin B12 for DNA synthesis, and copper and vitamin C that serve as cofactors for some of the enzymes that synthesize hemoglobin. D. Leukocyte Production 1.Leukopoiesis is the production of white blood cells; it begins when hemocytoblasts differentiate into three types of cells: B progenitors, T progenitors, or granulocyte-macrophage colony-forming units. 2.A variety of hormones stimulate the production of specific types of leukocytes in response to specific needs of the body. These include the cytokines such as colony stimulating factors and interleukins. 3.Granulocytes and monocytes are stored in red bone marrow and released when needed. Lymphocytes begin developing in bone marrow, then migrate to lymphoid tissue to mature. E. Platelet Production 1.Platelet production (thrombopoiesis) begins when a hemocytoblast becomes a megakaryoblast. In response to thrombopoietin, the megakaryoblast develops into a huge megakaryocyte. Thrombopoietin is produded by the liver and kidneys. This large cell fragments; some of the fragments become functional platelets. C. in patients who cannot normally form the blood cells. (Clinical Application) VI. ERYTHROCYTES (RED BLOOD CELLS) A. Form and Function 1.Red blood cells or erythrocytes (RBCs) contain the oxygen-carrying protein hemoglobin and number about 5.4 million cells/microliter of blood in males and 4.8 million cells/microliter in females. 2.Erythrocytes (RBCs) carry oxygen from the lungs to the tissues and return carbon dioxide from the tissues to the lungs. 5 3.RBCs are disc-shaped with exterior glycoproteins and glycolipids, conferring blood type, and interior peripheral proteins to impart elasticity to the cell. 4.During development, RBCs lose most of their organelles. This includes mitochondria which use oxygen for aerobic respiration. They can also carry on anaerobic fermentation indefinitely. 5.About one-third of the cytoplasm of an RBC consists of hemoglobin (280 million molecules per cell), which carries most of the oxygen and some of the carbon dioxide transported by the blood. 6.The shape of the RBCs allows the rapid diffusion of gases throughout the cell. B. Hemoglobin 1.Hemoglobin consists of four protein chains called globins. Two are alpha chains, and two are beta chains. Each chain is conjugated with a nonprotein heme group that binds oxygen to a ferrous ion at its center. 2.Carbon dioxide is transported bound to the globin portion of the hemoglobin. 3.Hemoglobin exists in several forms that differ in their structure and oxygen-carrying capacity. Fetal hemoglobin has a higher oxygen-binding capacity than adult hemoglobin, and thus can extract oxygen from the mother's blood. C. Quantities of Erythrocytes and Hemoglobin 1.The number of RBCs is of clinical interest because it indicates the oxygen-carrying capacity of the blood. 2.The hemoglobin concentration is 13–18 g/dL in men, and 12–16 g/dL in women. The RBC count is also higher in men, with 4.6 to 6.2 million RBCs per mm3 in men and 4.2 to 5.4 million per mm3 in women. Male hematocrits range from 40-54% and female hematocrits range from 3747%. 6 3.This difference between the sexes exists because male androgens stimulate RBC production, women have menstrual cycles, and hematocrit is inversely proportional to body fat, which is usually higher in women. 4. The percentage of total blood volume occupied by red blood cells is called the hematocrit. A hematocrit measures the percentage of red blood cells in whole blood. a. A significant drop in hematocrit indicates anemia, due to a lower than normal number of RBCs. b. In polycythemia the percentage of RBC is abnormally high with a higher than normal hematocrit. 5. The practice called induced erythrocytemia (blood doping) has been used by some athletes in an attempt to boost the oxygen-carrying capacity of their blood before an athletic event. Although evidence suggests that there may be performance benefits related to the procedure, the potential risks from higher blood viscosity are unknown and the practice is considered dishonest by the International Olympics Committee. D. RBC Physiology 1. The function of the hemoglobin in RBCs is to transport oxygen and some carbon dioxide. Hemoglobin molecules are specialized components of the red blood cell plasma membrane that combine with oxygen (as oxyhemoglobin) or with carbon dioxide (as carbaminohemoglobin) in this transport process. 2. Hemoglobin also functions in blood pressure regulation. a. Unsaturated hemoglobin picks up CO2 and nitric oxide (NO), a gas, which it releases in the lungs. b. Saturated hemoglobin carries fresh O2 and supernitric oxide (SNO) and releases them in body tissues. c. NO tends to cause vasoconstriction; SNO causes vasodilation. 7 d. By ferrying NO and SNO throughout the body, hemoglobin helps regulate blood pressure by adjusting the amount of NO or SNO to which blood vessels are exposed. D. RBC Life Cycle (Erythrocyte Death and Disposal) 1. Erythrocytes circulate for 120 days. As they age, their membranes become more fragile and can no longer squeeze undamaged through tiny capillaries. 2. The spleen traps and destroys old cells. Hemolysis is the rupture of RBCs, which releases hemoglobin. 3. The globin portion of hemoglobin is hydrolyzed to amino acids. The heme portion has its iron removed and transported using transferrin. The remainder of the heme becomes the greenish pigment biliverdin that is further modified into bilirubin. These two pigments are added to bile by the liver, and are responsible for the color of feces and urine. Urobilin (urochrome) produces the yellow color of urine and stercobilin gives feces its characteristic color. F. Erythrocyte Disorders 1.Polycythemia is an excess of red blood cells. a.Primary polycythemia is due to cancer of the myeloid tissue. b.Secondary polycythemia is caused by lung damage, high altitude, or other factors leading to hypoxia. c.Polycythemia is dangerous because of the increased blood pressure and viscosity that result from it. 2.Anemia is a deficiency of either RBCs or hemoglobin. a.Anemia falls into three categories: (1)inadequate erythropoiesis or hemoglobin production usually due to a nutritional deficiency), (2)hemorrhagic anemia from bleeding, and 8 (3)hemolytic anemia from red blood cell destruction. • b.Three potential consequences of anemia are hypoxia, reduced blood osmolarity, and reduced blood viscosity. 3.Sickle-cell disease and thalassemia are hereditary disorders affecting hemoglobin. 4.Sickle-cell hemoglobin (HbS) differs from normal hemoglobin (HbA) and is caused by a recessive allele. People who are heterozygous for the trait are also resistant to malaria. They have sickle-cell trait, but not malaria. Those homozygous for the recessive sickle-cell gene have sicklecell disease. a.At low oxygen concentrations, HbS causes RBCs to elongate and become sticky; they agglutinate and block small blood vessels, causing pain and fatigue as tissues are starved of oxygen. Hemopoietic tissues become active to counter the hypoxemia, and bones become misshapen and enlarged. b.Without treatment, those who are affected rarely live past the age of 2; with excellent treatment, life expectancy is only 50. 5.Thalassemia is seen among people of Mediterranean descent and is characterized by a lack or deficiency of alpha or beta polypeptides, resulting in very low RBC counts. VI. WHITE BLOOD CELLS A. Leukocytes (white blood cells or WBCs) are nucleated cells and do not contain hemoglobin. Two principal types are granular (neutrophils, eosinophils, basophils) and agranular (lymphocytes and monocytes). B. Granular leukocytes include eosinophils, basophils, and neutrophils based on the straining of the granules. C. Agranular leukocytes do not have cytoplasmic granules and include the lymphocytes and monocytes, which differentiate into macrophages (fixed and wandering). 9 D. Leukocytes have surface proteins, as do erythrocytes. They are called major histocompatibility antigens (MHC), are unique for each person (except for identical siblings), and can be used to identify a tissue. E. The general function of leukocytes is to combat inflammation and infection. 1. WBCs leave the blood stream by emigration (Diapedesis). 2. Some WBCs, particularly neutrophils and macrophages, are active in phagocytosis. 3. The chemical attraction of WBCs to a disease or injury site is termed chemotaxis. F. WBC Physiology 1. White blood cells usually live for only a few hours or a few days. Normal blood contains 5,000-10,000 leukocytes/mm3. a. Leukocytosis refers to an increase in the number of WBCs. b. Leukopenia refers to an abnormally low number of WBCs. 2. The general function of leukocytes is to combat inflammation and infection. a. WBCs leave the blood stream by emigration. b. Some WBCs, particularly neutrophils and macrophages, are active in phagocytosis. c. The chemical attraction of WBCs to a disease or injury site is termed chemotaxis. d. Different WBCs combat inflammation and infection in different ways. 1) Neutrophils and wandering or fixed macrophages (which develop from monocytes) do so through phagocytosis. Neutrophils have fine granules that contain antimicrobial agents. They have lobed nuclei, and function in the phagocytosis of bacteria and release of antimicrobial agents. They produce defensins which poke holes in the membranes of pathogens, lysozyme, and oxidants such as superoxide anion, hydrogen peroxide, and hyperchlorite. 2) Eosinophils combat the effects of histamine in allergic reactions, phagocytize antigen-antibody complexes, and combat parasitic worms. 10 Eosinophils have coarse cytoplasmic granules that stain orange-pink with eosin dye. The nucleus is bilobed. Eosinophils phagocytize antigen-antibody complexes, allergens, and inflammatory chemicals, and they aggregate near parasites and release enzymes to destroy them. They produce histaminase to combat histamine. 3) Basophils develop into mast cells that liberate heparin, histamine, and serotonin in allergic reactions that intensify the inflammatory response. Basophils have a U- or S-shaped nucleus and coarse granules that stain purple with basic dye. Basophils release histamine (a vasodilator) and heparin (an anticoagulant), thereby increasing blood flow into an area and promoting the mobility of other WBCs. 4) Lymphocytes are only slightly larger than RBCs and have a rounded nucleus. They secrete antibodies (B cells), destroy foreign, virally infected or cancer cells (T cells), or secrete chemicals to enhance the functions of other immune cells (helper T cells). One group, the natural killer cells, functions in nonspecific defense. T cells. B Cells. Natural Killer cells. 5)Monocytes Monocytes are the largest of the formed elements, with variably shaped nuclei and clear cytoplasm. These cells differentiate into macrophages that, in turn, phagocytize foreign particles and debris and activate other cells of the immune system. These cells form osteoclasts. 11 e. A differential white blood cell count is a diagnostic test in which specific white blood cells are enumerated. Because each type of WBC plays a different role, determining the percentage of each type in the blood assists in diagnosing the condition. 3. Bone marrow transplants may be used to treat several types of anemia, leukemia, and numerous other blood disorders. Abnormalities of Leukocyte Count • Total WBC count is usually 5,000 to 10,000 per mm3. A count less than this (leukopenia) can result from toxic chemicals, drugs, or certain diseases. • A higher than average count (leukocytosis) indicates an infection, allergy, dehydration, or emotional disturbance. • A more useful count is a differential WBC count, which identifies the relative abundance of each type of white cell. A high neutrophil count indicates a bacterial infection, such as might occur with appendicitis, for example. Numerous eosinophils indicate allergies or parasites. • An extraordinarily high number of WBCs is characteristic of leukemia, or cancer of the hemopoietic tissues. • Myelocytic leukemia shows uncontrolled granulocyte production, while lymphocytic leukemia is characterized by uncontrolled lymphocyte production. • Acute leukemia progresses rapidly after a sudden onset; chronic leukemia develops and progresses more slowly. • Death from leukemia is usually due to bleeding or opportunistic infection as the cancerous tissue crowds out other blood-forming tissues VIII. PLATELETS A. Thrombopoietin stimulates myeloid stem cells to produce platelets. 1. Myeloid stem cells develop into megakaryocyte-colony-forming cells that develop into megakaryoblasts. 12 2. Megakaryoblasts transform into megakaryocytes which fragment. 3. Each fragment, enclosed by a piece of cell membrane, is a platelet (thrombocyte). B. Normal blood contains 250,000 to 400,000 platelets/mm3. Platelets have a life span of only 5 to 9 days; aged and dead platelets are removed by fixed macrophages in the spleen and liver. C. Platelets help stop blood loss from damaged vessels by forming a platelet plug. Their granules also contain chemicals that promote blood clotting. D. Platelets secrete growth factors (platelet derived growth factor ) that stimulate mitosis in fibroblasts and smooth muscle, and help maintain linings of blood vessels. E. Platelets secrete vasoconstrictors that cause vascular spasms in broken vessels. F. They phagocytize and destroy bacteria, and secrete chemicals that attract neutrophils and monocytes to inflamed areas. G. They dissolve blood clots that have outlasted their usefulness. IX. HEMOSTASIS A. Hemostasis refers to the stoppage of bleeding. When blood vessels are damaged or ruptured, the hemostatic response must be quick, localized to the region of damage, and carefully controlled. B. It involves 1.vascular spasm, 2.platelet plug formation, and 3.blood coagulation (clotting). C. Vascular Spasm 1.Vascular spasm is the prompt constriction of a broken vessel to help stop bleeding. It is triggered by nervous impulses (pain pathway), by injury to the smooth muscle within the vessel wall, by serotonin (a vasoconstrictor) from platelets, and endothelins from damaged blood vessels. 2.Vascular spasm can usually be maintained long enough for platelet plug formation and coagulation to have an effect. 13 D. Platelet Plug Formation 1.When a vessel is injured, collagen fibers in its wall are exposed, causing platelets to stick to them. Platelets extend spiny pseudopods that adhere to the broken vessel; these contract and draw the walls of the vessel together. 2.As more platelets join in, a platelet plug forms that can stop minor bleeding. 3.Platelets undergo degranulation as they aggregate, releasing substances that promote hemostasis. Thromboxane A2 and serotonin stimulate vascular spasm. ADP stimulates other platelets to become sticky and adhere to the platelet plug. E. Coagulation 1. A clot is a gel consisting of a network of insoluble protein fibers (fibrin) in which formed elements of blood are trapped. 2. The chemicals involved in clotting are known as coagulation (clotting) factors; most are in blood plasma, some are released by platelets, and one is released from damaged tissue cells. 3. Blood clotting involves a cascade of reactions that may be divided into three stages: formation of prothrombinase (prothrombin activator), conversion of prothrombin into thrombin, and conversion of soluble fibrinogen into insoluble fibrin. 4. The objective of coagulation is to convert soluble fibrinogen into insoluble fibrin. As this occurs, blood cells and platelets get stuck in the net of fibrin, stopping blood loss. 5. The two reaction pathways to coagulation are the extrinsic mechanism, initiated by chemicals released from damaged tissue (tissue factor also known as thromboplastin), and the intrinsic mechanism, initiated by factors within the vessel itself, such as clots. 6. Clotting factors are called procoagulants and are produced in the liver. They normally circulate with the plasma in inactive form. 7. One clotting factor activates the next, which in turn activates another factor, and so on, in a reaction cascade. 14 8. The three steps in the coagulation process are: a. b. c. d. Normal coagulation requires vitamin K and also involves clot retraction (tightening of the clot) and fibrinolysis (dissolution of the clot). 1. The fibrinolytic system dissolves small, inappropriate clots and clots at a site of damage once the damage is repaired. 2. Plasmin (fibrinolysin) can dissolve a clot by digesting fibrin threads and inactivating substances such as fibrinogen, prothrombin, and factors V, VIII, and XII. e. The Fate of Blood Clots 1. After a clot forms, it undergoes clot retraction (syneresis) within 30 minutes. 2. Platelets and endothelial cells secrete a stimulant causing fibroblasts and smooth muscle cells to multiply and repair the damaged vessel. 3. Fibroblasts invade and strengthen the clot. 4. When tissue repair is completed, the clot is dissolved by fibrinolysis. This process involves a cascade of reactions, ending in the production of plasmin, a fibrin-dissolving protein. Review tissue plasminogen activator. E. Despite the anticoagulating and fibrinolytic mechanisms, blood clots sometimes form within the cardovascular system. 1. Clotting in an unbroken blood vessel is called thrombosis. 2. A thrombus (clot), bubble of air, fat from broken bones, or piece of debris transported by the bloodstream that moves from its site of origin is called an embolus. 15 3. Anticoagulants such as heparin or warfarin and thrombolytic agents such as streptokinase or tissue plasminogen activator can be used to prevent or dissolve clots in the body. F. Prevention of Inappropriate Coagulation 1. Controls are required to prevent unnecessary coagulation. These include platelet repulsion, dilution, and anticoagulants such as antithrombin, protein C and heparin. a.Platelet repulsion due to the prostacyclin that coats the endothelium of undamaged blood vessels. b.Dilution of clotting agents due to blood flow. c.Anticoagulants. d.Absorption of thrombin by fibrin. G. Coagulation Disorders 1.Radiation, drugs, poisons, or leukemia can lead to thrombocytopenia, or low platelet count. People with this condition bruise easily. 2.A deficiency in one clotting factor can shut off the coagulation mechanism, as is the case in hemophilia. 3.Lack of factor VIII causes hemophilia A, which affects 1 out of 5,000 males and accounts for 83% of hemophilia cases. Lack of factor IX causes hemophilia B (seen in 1 out of 30,000 males). Factor VIII is now produced by transgenic bacteria. 4.Most coagulation disorders are in the form of an unwanted blood clot (thrombosis). A thrombosis is a clot in an unbroken blood vessel. The clot itself is called a thrombus. If it begins to travel, it is an embolus. Clots arising in the arms and legs (from patient inactivity) commonly lodge in the lungs, causing pulmonary embolism. 16 H. Despite the anticoagulating and fibrinolytic mechanisms, blood clots sometimes form within the cardovascular system. 1. Clotting in an unbroken blood vessel is called thrombosis. 2. A thrombus (clot), bubble of air, fat from broken bones, or piece of debris transported by the bloodstream that moves from its site of origin is called an embolus. 3. Anticoagulants such as heparin or warfarin and thrombolytic agents such as streptokinase or tissue plasminogen activator can be used to prevent or dissolve clots in the body. • Intravascular Clotting • Thrombosus – Clotting in an unbroken blood vessel. • __________ – The name for the clot itself. • __________ – A blood clot, bubble of air, fat from broken bones in the blood stream. • Embolism – When an embolus lodges in a smaller diameter artery. X. BLOOD GROUPS AND BLOOD TYPES A. The surfaces of red blood cells contain genetically determined blood group antigens, called agglutinogens or isoantigens. 1. Blood is categorized into different blood groups based on the presence or absence of various isoantigens. 2. Within a blood group there may be two or more different blood types. 3. Major blood groups are the ABO and Rh groups. Other blood groups include the Lewis, Kell, Kidd, and Duffy systems. B. ABO Group 1. The ABO Group a.The ABO blood group was discovered in 1900 by Karl Landsteiner. 17 b.Surfaces of blood and body cells possess antigens that are capable of stimulating an immune response in another person. The antigens of RBCs that determine blood type are called agglutinogens because of their role in agglutination during mismatched blood transfusions. Plasma antibodies that react against agglutinogens are agglutinins. c.The ABO blood group consists of blood types A, B, AB, and O. The presence of ABO agglutinogens determines the person's blood type, as determined by genetics. d.Type A blood has type A agglutinogens (antigens) on the surface of its RBCs, and anti-B agglutinins (antibodies) in its plasma. Type B blood has type B agglutinogens (antigens) and anti-A agglutinins (antibodies). Type AB has both agglutinogens (antigens) but no agglutinins (antibodies), while type O has no agglutinogens (antigens), but both anti-A and anti-B agglutinins (antibodies). e.Mismatching blood types can lead to clumping (agglutination) of the blood in a transfusion reaction. This can result in the lysing of erythrocytes causing release of hemoglobin into the bloodstream. Death can follow within a week or two due to kidney failure. B. The Rh Group 1.The Rh blood group is so called because of the rhesus monkey in which it was first discovered. 2.If any of the Rh agglutinogens are present on the RBCs, the person is Rh positive. If none are present, the person is Rh negative. 3.Anti-Rh agglutinins are normally absent, unlike the situation for the ABO blood groups. 4.Problems arise when an Rh-negative person receives a transfusion from an Rh-negative person, and they begin to produce antibodies against the Rh factor. The next time Rh-positive blood is received, the recipient's plasma agglutinins agglutinate the donor's RBCs. This condition is referred to as hemolytic of the newborn. 18 5.A similar situation called hemolytic disease of the newborn occurs when an Rh-negative woman is carrying an Rh-positive fetus. The first fetus goes unharmed, but when a second Rh-positive fetus begins to grow, the mother's anti-Rh antibodies cause a severe anemia in the infant, called hemolytic disease of the newborn. This can be prevented by administering an anti-Rh gamma globulin injection called RhoGAM to the mother shortly after the first, and subsequent, Rh-positive babies are delivered. C. Transfusions 1. Knowledge of blood types is essential to safe transfusion of blood and may also be used in proving or disproving paternity, linking suspects to crimes, or as a part of anthropology studies to establish a relationship among races. D. Typing and Cross-Matching Blood for Transfusion 1. The Rh and ABO blood groups may be detected by a simple medical test, blood typing, in which a sample of blood is mixed with serum containing agglutinins to each of the major agglutinogens (AB, B, and Rh). 2. Typing is the determination of blood types, whereas cross-matching is the mixing of donor and recipient blood for compatibility. XI. DISORDERS: HOMEOSTATIC IMBALANCES A. Anemia is a condition in which the oxygen-carrying capacity of the blood is reduced; it is a sign, not a diagnosis and is usually characterized by a decreased erythrocyte count or hemoglobin deficiency. Kinds of anemia include iron-deficiency, pernicious, hemorrhagic, hemolytic, Thalassemia, and aplastic. B. Sickle-cell disease is an inherited disorder due to an abnormal kind of hemoglobin. RBCs show a characteristic sickle shape, rupture easily, and show a reduced oxygen carrying capacity which results in hemolytic anemia. 19 C. Hemophilia is an inherited deficiency of clotting in which bleeding may occur spontaneously or after only minor trauma. D. Disseminated intravascular clotting is a disorder of hemostasis characterized by simultaneous and unregulated blood clotting and hemorrhage. E. Acute leukemia is a malignant disease of blood-forming tissues characterized by uncontrolled production and accumulation of immature leukocytes. In chronic leukemia, there is an accumulation of mature leukocytes in the bloodstream because they do not die at the end of their normal life span. 20