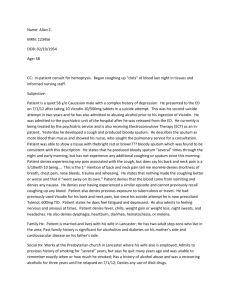
Running Header: PHYSICAL ASSESSMENT Physical Assessment
advertisement

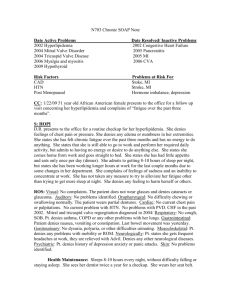
1 Running Header: PHYSICAL ASSESSMENT Physical Assessment Connie Wilson NURS 3293 Columbus State University 2 Running Header: PHYSICAL ASSESSMENT Current Health Status I performed my physical assessment on a 75 year old female who is retired and lives with her spouse. The assessment took place in her home for the purpose of assisting me with this assignment and has no physical complaints at this time. She is currently monitored for the following conditions: Hypertension, Hypothyroidism, Renal Insufficiency, Osteoarthritis, glucose intolerance, anxiety and Polycythemia. She has had several recent incidents of falling and “passing out”, the cause remains unidentified. Past Medical History When asking the patient about past health issues I get some conflicting information. She denies having chicken pox, but has had shingles in 1981, and reports having mumps at the age of 24. Her surgical history includes a Thyroidectomy in 1962, Hysterectomy in 1977, ORIF right ankle in 1998, Fusion of right ankle in 2001, Cholecystectomy in 2007, right total hip replacement in 2011, and left total hip replacement in 2012. She had a DVT in 2010 and also had a stent placed in her left shoulder on 2013 for another blood clot. She is a gravida 3 and para 3, her first child was born at the age of 19. The patient recently had her flu vaccination within the past week but refuses the pneumonia vaccine. She has not had the shingles vaccine and is current on her tetanus. She routinely sees her dentist for preventative and correctional care; mammograms are done yearly, and she has not seen a gynecologist is several years. She utilizes a chiropractor for complaints of occasional back discomfort. She reports exercise is nonexistent due to leg weakness and instability. There have not been in dietary changes nor any weight loss or gain. No known drug or food allergies. 3 Running Header: PHYSICAL ASSESSMENT Family History Mother – Cervical and Colon cancer, Myocardial Infarction (MI), Transient Ischemic Attack (TIA), Hypertension (HTN), dementia, and Diabetes Mellitus (DM), died at age of 85 due to cancer. Father - MI, died at age of 43. Brother - Coronary Artery Disease (CAD), DM, MI, smoker, died at age of 65 due to CAD. Sister – Congestive Heart Failure (CHF), DM, Lung cancer, renal failure, alcohol abuse, smoker, died at age 65 due to multiple issues listed. Brother – CAD, MI, DM, smoker, died at age 58 due to CAD and DM. Patient denies use of recreational drugs, does not smoke, and has an alcoholic beverage one to two times yearly. Hobbies include reading to relax, baking, and enjoys attending the local Baptist church. 4 Running Header: PHYSICAL ASSESSMENT Medications Losartan 50mg BID for HTN Premarin 0.9mg 6 tabs weekly for hormone replacement therapy PreCrea (dose unknown) 2 tabs daily for impaired glucose tolerance Calcitrol 0.25mcg, 3 tabs daily, calcium replacement due to hysterectomy Hydroxyurea 500mg, 1 cap daily for Polycythemia Warfarin 2.5mg daily, for history of blood clots Levothyroxine .088mg daily for hypothyroidism Citalopram 20mg daily for anxiety Bystolic 5mg daily for HTN Losartan 50mg BID, for HTN Lorazepam 0.5mg prn for SBP > 160 Hydroxyzine 25mg prn for itching Nitrostat 0.4mg prn chest pain Glucosamine/Chondroitin 1500mg daily, supplement for joint mobility, OTC Dermex-P 1 tablet daily, supplement for skin, OTC 5 Running Header: PHYSICAL ASSESSMENT Mini-Mental Examination The Mini –Mental Status Examination was performed, the patient scored 30, with the maximum score available being 30. The breakdown of the scoring is as follows: Orientation to Time- scored 4 out of 5 Orientation to Place-scored 5 out of 5 Immediate Recall- scored 3 out of 3 Attention-Part A- scored 2 out of 5 Part B-scored 5 out of 5 Delayed Verbal Recall- Part A-scored 2 out of 3 Naming-scored 2 out of 2 Repetition-scored 1 out of 1 3-Stage Command-scored 3out of 3 Reading, Writing, and Copying-scored 3out of 3 6 Running Header: PHYSICAL ASSESSMENT 24 Hour Food Diary Time Food Item Portion Calorie Count Total 0800 Cheerios 1 cup 255 0800 whole milk 1 cup 103 1200 peanut butter/jelly 1 376 1200 whole milk 1 cup 103 1700 crackers/pepperoni 5 130 1700 whole milk 1 cup 103 233 Snack energy bar 1 235 235 358 479 1,305 Dietary Education I attempted to discuss adding vegetables in her meals to encourage a balanced diet; she was very resistant to the conversation. I did note a cake (half eaten) in the kitchen and encouraged her to drink more water. She does not cook dinner as frequently as she once did. She is capable of cooking with no barriers other than a lack of desire to do so. As a last attempt, I suggested adding BOOST or Ensure to get the vitamins and minerals she is most likely missing. The response was about the same. 7 Running Header: PHYSICAL ASSESSMENT Physical Assessment After cleaning my hands I began the physical assessment by letting her know if she felt uncomfortable at any time to let me know and we would stop the process or change what we were doing. I asked her to have a seat, then assessed for orientation, along with verbal and motor response. The Glasgow Coma Scale score was 15, resulting in a normal score. Vital signs at the time of the exam were: B/P 172/82, HR 80, R18 and regular, T 98.5 orally. Skin I began by an overall observation of her appearance; her skin is even in color and clean with no signs of cyanosis or jaundice. One small ecchymotic area noted on left forearm, asked patient about this and she responded this was a result of her taking Coumadin. Scars were noted on bridge of nose, neck, and right ankle. Patient reports scar on the nose resulted from a recent fall, she had a thyroidectomy in the past, and the scar on the ankle was from a fusion surgery. She also reports she has scars on each hip due to hip replacement surgery. Her skin is thinning, tenting noted bilaterally on hands, small superficial veins noted around ankles and legs were clean shaven, therefore I was unable to assess for hair distribution on legs. Hair on forearms was absent and eyebrows were thin, with outer third of brow absent. Patient denies any skin complaints other than dryness which she treats successfully with over the counter (OTC) products. No rashes or lesions were found, she sees a dermatologist routinely for skin cancer screenings. She does have a history of sunbathing and sunburn. Temperature equal bilaterally when hands and feet were assessed. Feet noted to be slightly cooler to touch. 8 Running Header: PHYSICAL ASSESSMENT Fingernails The patient was wearing artificial nails and toenails were painted, she is clean and wellmanicured. Fingertips were of normal shape and capillary refill was less than 3 seconds on fingers and toes which is considered “brisk” in description. No indications of cyanosis or clubbing noted. Head Patient’s hair is thinning and she routinely colors. No skin abnormalities noted on the scalp, she denies itching, dryness, eczema, or any other scalp conditions. Palpation of scalp reveals normal shape and symmetry, no abnormalities were felt. Patient denies any pain or tenderness upon examination. Ears Ears are equal in size and shape bilaterally; they are clean and free of drainage or redness. She denies any pain or tenderness. She does have hearing loss bilaterally and wears hearing aids. She was not wearing them during the assessment and failed the whisper test. Face Face is symmetrical, no drooping of eyes, smile is equal. I performed the cotton ball test to assess the trigeminal nerve, also called cranial nerve 5, which she passed. No deficits were noted. I palpated her sinuses, patient denied pain or tenderness. 9 Running Header: PHYSICAL ASSESSMENT Eyes, Nose, and Throat We began her eye exam with the Snellen eye test, she stood 20 feet away from the chart and read the smallest line possible with each eye and she had a result of 20/40 bilaterally while wearing her glasses. We then did the near vision test, she struggled with the exam and her results were 16/160 in the right eye and16/80 in the left eye while wearing her glasses. She did not seem surprised by the results and reports she has had trouble seeing recently. She has an existing appointment scheduled for the near future with her eye doctor. Her pupils were checked with a pen light, they were equal and reactive to light with good accommodation. The six cardinal fields of gaze were checked and no nystagmus was seen. Confrontation was assessed and no deficits were noted. The vision tests checked cranial nerves 2, 3, 4, and 6, which are the optic, oculomotor, trochlear, and abducens. Observation of the sclera is white, no halos noted around the iris, mucus membranes are pink and moist, eyes are of normal shape with no drainage, and eyelashes are present. She wears glasses and sees her eye doctor regularly. The nose was checked for patency bilaterally, each side was clear and free of drainage. A smell test was performed to check the olfactory nerve, cranial nerve 1.Hand sanitizer was used to perform the test and no deficits were found. The bridge of the nose was slightly swollen and a scar was found, she reported this was a result of the fall she had recently. The bridge of the nose was fractured, therefore palpation was not performed. Observation of throat began with mucous membranes moist and pink in appearance. There were no lesions or abnormalities seen, asked the patient to say “ahhh”, the uvula remained midline. The hard and soft palates appear normal. She was able to swallow water without difficulty. 10 Running Header: PHYSICAL ASSESSMENT This was an assessment of cranial nerves 9 and 10, glossopharyngeal and vagus nerves. She denies having any problems or complaints with her throat or swallowing and denies hoarseness. She is able to move tongue side to side and up and down, with and without resistance, this assesses cranial nerve 12 which is the hypoglossal nerve. Neck Patient has had a thyroidectomy in the past, therefore palpated only to assess swallowing. No abnormalities were noted. She is able to turn head side to side, with and without resistance, also at this point, let it be noted that there were no pulsations to be seen to indicate higher vascular pressures. When asked, the patient performed a shoulder shrug with and without resistance, this assessed cranial nerve 11 which is the accessory nerve. She denies having any neck discomfort other than the occasional “stiff neck” after sleeping on it wrong. At this point I palpated the lymph nodes. I began with the retro-pharyngeal, then to pre and post auricular, occipital, moved down the cervical chain feeling for deep and superficial nodes and ended at the supraclavicular site. No lymphadenopathy was noted. Patient denied any tenderness at any of these locations. Breast Exam Breast exam was performed, palpation around breast revealed no abnormalities. Self-breast exam teaching was provided; patient was able to demonstrate how to perform and states she checks almost every week. As stated previously, mammograms are performed routinely. 11 Running Header: PHYSICAL ASSESSMENT Cardiovascular I began assessing her cardiovascular system by checking pulses. Brachial pulses were difficult to palpate, therefore I rated them at 1+ bilaterally, radial pulses bilaterally were 2+, popliteal were 2+ bilaterally, and dorsalis pedis were 2+ bilaterally. I also checked the temporal and carotids bilaterally and all were 2+. At the temporal and carotid locations I listened for bruits with the bell of my stethoscope and none were heard. I found no edema around the eyes or extremities. Patient does report that ankles swell occasionally if she stands for too long, elevating the legs corrects the problem. She denies any extremity pain. Auscultation of the heart was performed as follows with the diaphragm of the stethoscope: Right sternal border (RSB) and 2nd intercostal space (ICS), the aortic valve is assessed and S2 should be louder than S1. Normal sounds were heard. LSB and 2nd ICS, the pulmonic valve is assessed and S2 should be louder than S1. Normal sounds were heard. LSB and 3rd ICS, the ERB’s point is assessed and S2 and S1 should be equal. Normal sounds were heard. LSB and 4th ICS, the tricuspid valve is assessed and S1 should be louder than S2. Normal sounds were heard. LSB and 5th ICS, the mitral valve is assessed and S1 should be louder than S2. Normal sounds were heard. 12 Running Header: PHYSICAL ASSESSMENT No extra sounds such as clicks, extra beats, or murmurs were heard. Recent echo revealed normal findings per patient. I asked the patient to hold her breath at each location while I listened for bruits. None were heard. Patient denies having shortness of breath at either rest or on exertion. She is able to walk a flight of stairs without difficulty. She had an episode of chest pain last year which resulted in an infection being the cause. The hospital gave her a prn order for Nitrostat that she does not use. Respiratory Observation of patient’s chest reveals normal shape; respirations are even, regular, and unlabored. I auscultated lung sounds with the diaphragm of the stethoscope anteriorly, laterally, and posteriorly at all three levels. All lung sounds were clear, no wheezing, crackles, or rales heard. Patient denies complaints of recent illness, shortness of breath, or discomfort. I palpated for tactile fremitus while the patient counted to 100 and had a positive result posteriorly between the scapulae. I placed hands posteriorly, near bottom of ribs and asked patient to breathe in and out. Rise and fall is equal bilaterally. Patient has no current respiratory issues that she sees a physician for. Musculoskeletal Initial observation noted that patient’s finger joints were swollen and deformed. Patient reports she has osteoarthritis and scoliosis. I asked patient to stand and bend over if possible, spine is curved, and one hip is noted to be higher than the other. Kyphosis is also noted. She has a history of a fractured ankle where arthritis became aggressive and the ankle had to be fused. Osteoarthritis is also responsible for bilateral hip replacements. TMJ joint was palpated and no 13 Running Header: PHYSICAL ASSESSMENT abnormalities were found. Patient will take occasional Tylenol for pain relief. I assessed patient for strength, while grips were weak, they were equal bilaterally. Patient’s gait is slow and cautious, educated her on picking up her feet to prevent catching toe of shoes to prevent falls. We also talked about safety, removing throw rugs and keeping floor free of clutter. Patient was receptive to this advice. Neurological Assessment Most of the neurological assessment was performed during other sections of the physical exam; cranial nerve (CN) 1 was the olfactory nerve and was assessed performing the smell test. We assessed vision and cranial nerves 2, 3, 4, 6 which are the optic, oculomotor, trochlear, and abducens. CN 5, trigeminal nerve, was assessed with the cotton ball test. CN 9 and 10, glossopharyngeal and vagus nerves were assessed when the throat was examined and the swallow test was performed. CN 11 is the accessory nerve and was assessed while checking the shoulder shrug, and CN 12 is the hypoglossal nerve and was assessed when patient was asked to perform tongue movements. A sharp/dull test was performed on her extremities and no deficits were found. She was able to identify an object in her hand while eyes were closed, I also traced a number in her palms while eyes were closed and she was able to identify the number correctly. These assessments are checking for cortical diseases. Reflexes were assessed; I checked biceps, triceps, and patella reflex points bilaterally with a reflex hammer, I received negative results on all except the right patella which was graded at a 2+. 14 Running Header: PHYSICAL ASSESSMENT I asked patient to perform a rapid hand movement, she is able to follow directions and perform correctly, although speed was a little slow. Finger to nose was performed without deficits. She was unable to perform the heel to toe walk due to balance issues. Abdomen I asked patient to lie down on sofa to assess abdomen. I listen for bowel sounds in all four quadrants with the diaphragm of the stethoscope, all were active. I also listened for bruits while patient was in this position. I assessed the renal, iliac and aortic arteries with the bell of the stethoscope. No bruits were heard. I then palpated the abdomen in all quadrants; patient denies any pain or tenderness. Femoral arteries were assessed, each side was strong and given a 2+. While patient was in this position, I assessed the strength in the lower extremities by having her push with her feet against my hands and then pull against my hands. She was equal bilaterally. Impression Overall, the patient is compliant with medical treatments and follows up with appointments for preventative and follow up care. She is resistant to dietary recommendations and has a habit of trying expensive supplements to self-treat her medical problems; an example of this is the PreCrea that is sold off of Amazon. She refuses to have a conversation about this area. The arthritis has limited her movements, making exercise difficult. Falling is her biggest risk at the moment due to taking Coumadin. I would recommend an appointment with a dietician to assist in improving her diet.