The Heart
advertisement

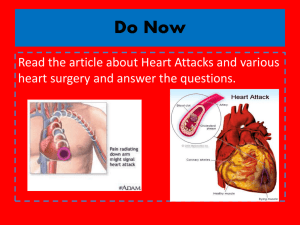
BIO 265 – Human A&P Chapter 18 The Heart The Heart Size Form Location – mediastinum – Figure 18.1 and from other text Heart Anatomy Pericardium (pericardial sac) – Figures 18.1 and 18.2 Heart Anatomy Heart Wall – Epicardium – Myocardium – Endocardium – Figure 18.2 Heart Structure and Function What are the heart chambers? Overview of heart function Figure 18.5 Coronary Circulation In order for the heart to function, it must have a constant supply of oxygen The coronary arteries carry the blood to the heart Figure 18.7 Heart Attack What is a heart attack or myocardial infarction? CD Animation Heart Valves What are the 4 valves in the heart? – Figure 18.8 Heart Valves Heart valve function – Figures 18.9 and 18.10 Heart Valves Heart sounds result from the closing of the heart valves Heart murmurs occur when a valve does not open or close properly CD Animation Histology What are the characteristics of cardiac muscle? – Branched fibers – Mitochondria – T-tubules – Intercalated disks with gap junctions – Figure 18.11 Conducting System What are the components? – Figure 18.14 Conducting System All cardiac muscle cells are autorhythmic – They can generate spontaneous AP – But the SA node is the pacemaker (it depolarizes faster than other areas of the heart) Figure 18.13 Conducting System Once the AP is generated it spreads through the atria to the AV node What role does the AV node play? – Delays the AP for a split second The AP then passes very quickly through the bundle branches – The effect is contraction at the apex first – Figure 18.14 Electrical Properties Cardiac muscle has an RMP similar to skeletal muscle Differences between cardiac and skeletal AP – Figure from other text Cardiac Action Potentials Phases of AP in contractile cells: – Depolarization • Na+ channels (fast channels) open • K+ channels are closed • Ca2+ channels (slow channels) begin to open – Early repolarization and plateau • Na+ channels close • Some K+ channels open • Ca2+ channels stay open – Figure from other text Cardiac Action Potentials – Final repolarization • Ca2+ channels close • many K+ channels open – Figure from other text Cardiac Action Potentials How would the AP in cardiac muscle stimulate a contraction? – Notice that Ca2+ comes from the extracellular fluid as well as the SR Cool CD Animations! (my CD) Electrocardiogram ECG wave patterns – Figures 18.16, 18.17, and 18.18 The Cardiac Cycle The cardiac cycle refers to the repetitive pumping process that occurs in the heart – Systole – contraction of the heart – Diastole – relaxation of the heart – CD animation The Cardiac Cycle Steps: – Ventricular filling • Passive – during complete diastole • Active – during atrial systole – Ventricular Systole • Isovolumetric Contraction – closes AV valves and opens semilunar valves • Period of Ejection – blood leaves the ventricles – Ventricular Diastole • Isovolumetric relaxation – semilunar valves close – Figure 18.20 The Cardiac Cycle Assuming an average 75 bpm: – Cardiac Cycle = 0.8 s – Atrial systole = 0.1 s – Ventricular systole = 0.3 s – Diastole = 0.4 s Awesome CD animation (my CD) Cardiac Output Cardiac output (CO) = Heart rate (HR) x Stroke volume (SV) of one ventricle Calculations (p.698) – Resting 75 bpm x 70 ml/beat = 5250 ml/min – Or in other words your entire volume of blood passes through each side of your heart each minute!!! – Exercise 20 liters/min to 35 liters/min Regulation of the Heart Regulation of cardiac output is critical for homeostasis Starlings law of the heart: – The greater the venous return to the heart, – The greater the stretch of the heart wall, – This results in a more forceful contraction and therefore a greater stroke volume Regulation of the Heart Neural regulation: – The heart is innervated by both sympathetic and parasympathetic fibers – Parasympathetic – decrease heart rate by releasing acetylcholine • It opens ligand-gated K+ channels • Effect? • Figure 18.15 Regulation of the Heart – Sympathetic – increases heart rate and force of contraction (stroke volume) • Norepinephrine (a neurotransmitter) stimulates the opening of the slow Ca2+ channels • It works through a G-protein system that synthesizes cAMP • Figures 18.22 and 18.15 Regulation of the Heart Hormonal Control – Epinephrine and norepinephrine – same effect as above Problems in Regulation: – Tachycardia – over 100 bpm – Bradycardia – under 60 bpm (can be normal in athletes) Regulation of the Heart – Congestive Heart Failure – cardiac output is too low to meet body tissue needs • Blood builds up in the veins (causing the “congestion”) – Causes: • Coronary Atherosclerosis – decreases the hearts pumping ability • Hypertension (high blood pressure) – ventricles can’t push the blood out into the arteries • Myocardial infarction Heart and Homeostasis How does the heart help maintain homeostasis? – Blood pressure example • Baroreceptors, the cardioregulatory center, and nerves – Figures from other text The Fetal Heart There are some interesting differences between the fetal and adult hearts Why? – Foramen ovalis in the atrial septum – Ductus arteriosis between the pulmonary trunk and the aorta – Figures 18.4b and e