Digestion
advertisement

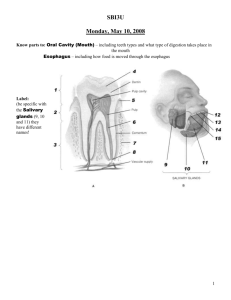
ANATOMY & PHYSIOLOGY THE DIGESTIVE SYSTEM Digestive System Ingestion: receiving food Digestion: breakdown of food particles small enough to pass through cell membranes Absorption: transfer of food into circulation A. Alimentary Canal – The Tube from beginning to end ~ 9m or 30ft. Oral Cavity Pharynx Esophagus Stomach Small Intestine Large Intestine Rectum/Anal Canal Walls of Alimentary Canal – 4 layers (inside outside) Mucosa – secrete mucus, protects surrounding tissue, absorbs nutrients Submucosa – nourishes surrounding tissues, carry away absorbed nutrients Muscular layer – move food to stomach (peristalsis) 1) Circular: changes diameter of tube 2) Longitudinal: changes length of tube Serous layer/serosa – produce serous fluid to prevent friction Tube Movements Mixing – some sections of the tube contract to mix and breakdown food Propelling (peristalsis) – wave-like movements push food through the canal B. Mouth/ Oral Cavity Cheeks – muscles for chewing Lips – sensory and manipulation of food Tongue – manipulated food; taste buds/receptors • Frenulum connects the tongue to the bottom of the mouth Palate (roof of mouth) – hard anterior, soft posterior • Uvula is extension of soft palate hangs down to direct food Teeth • 20 as a child, 32 as an adult • Incisors and canines: cutting and tearing • Premolars and molars: mastication Salivary Glands • Saliva – mostly water; slightly acidic, some antibodies 1) Serous cells: secrete serous fluid with digestive enzymes (amylase enzyme of the mouth) to lubricate food and begin digestion 2) Mucous cells: produce mucous to clump food into a ball/bolus 3) Three Glands a. b. c. Parotid – below the ear Submandibular – under the mandible (jaw) Sublingual – under the tongue Pharynx – cavity; posterior end of the mouth, leads to the esophagus Step 1 – chew, breakdown, mix with saliva into bolus Step 2 – swallowing reflex, once near the pharynx • Soft palate is raised to block the nasal passageway • Hyoid bone – larynx elevated to block trachea epiglottis then covers the opening • Muscle relax, lower pharynx and open esophagus • Peristaltic wave begins pushing food down esophagus Stomach – located on left portion of body, j-shaped Holds between 50 mL – 4L, folded when empty Digest proteins Absorbs very little – only few liquids, drugs, alcohol, and salts Mechanical and chemical digestion Regions of the Stomach Cardia –small region at the esophageal-stomach junction Fundus – formed by the upper curvature of the organ; temporary storage area for food Body – main, central region; holds max 4 Liters, avg. 0.9L Pylorus – small region at the stomach-duodenal junction; holds 30 mL only releases 3mL Cells of the Stomach/ Gastric Glands Mucous cells – secrete mucous for protection Chief cells – secrete digestive enzymes; pepsinogen Parietal cells – secrete HCL (hydrochloric acid); pH~ 2 Pepsinogen (an inactive enzyme) is converted to Pepsin when it reacts with HCl/acidic environment Pepsin breaks down proteins into amino acids 3 Layers of the Stomach Wall Serosal: outermost; thick connective tissue binds to other organs Muscularis: thick-middle; three layers of smooth muscle tissue. Mucosal: innermost; relatively thick and contains numerous tubular glands called gastric pits • Little to no digestion occurs here; alkaline (high pH) to combat HCl • Ulcers- holes in stomach, esophagus, duodenum brought on by stress Control of Gastric Juices Sight, smell, taste stimulates secretions (parasympathetic) Distension of the stomach and production of chemicals due to breakdown of food • Gastrin: hormone released with secretion also stimulates increase of secretion • Decrease juices if lots of fat/protein in the duodenum or if the intestine is extended. Digestion and Absorption in Stomach HCl + churning action breaks down food Smaller particles does what to surface area? What does this have to do with enzyme digestion? – Enzymes able to work better because they can attack a higher surface area Chyme: mixture of small food particles + acid + mucous Little absorption occurs through the walls of the stomach; foods high in fat stay in stomach the longest Exiting the Stomach Chyme: Ingested substances combine with the secretions of the glands of the stomach, producing a viscous, highly acidic soupy mixture of partially digested food Accessory Organs Liver Gallbladder Pancreas Liver: Largest gland/organ of the body; produces bile that is • • • • • • • stored in the gallbladder supplies quick energy metabolizes alcohol makes proteins stores vitamins and minerals regulates blood clotting regulates cholesterol production detoxifies poisons 3lbs. Requires 25% of cardiac output Gallbladder: stores and concentrates bile that is not needed immediately for digestion Bile: yellow-green, alkaline solution containing bile salts, bile pigments (primarily bilirubin), cholesterol, neutral fats, phospholipids, and a variety of electrolytes • Fat emulsification via bile salts • Bile does not usually enter the small intestine until the gallbladder contracts Pancreas (exocrine) • Digestive enzymes - break down carbs, proteins, and fats. • Base, bicarbonate ion (alkaline). - Neutralizes chyme from the stomach, permitting digestive enzymes to function. • Secretin stimulates production of bicarbonate ions • Cholecystokinin (CCK) stimulates production of enzymes Enzymes include: proteases, pancreatic lipase, and pancreatic amylase Small Intestine Receives chyme, pancreatic and liver secretions to complete digestion of nutrients • Duodenum: 25cm long x 5cm wide; c-shaped, most absorption of nutrients occurs here • Jejunum: middle; thicker more vascular walls, greater in diameter • Ileum: last section; suspended from abdominal wall by mesentery Duodenum Pancreatic enzymes & bile enter, continuing digestion. Villi: microscopic hair-like structures; absorption of nutrients • Active transport of sugars, amino acids, and fatty acids across membranes. • Pass through the epithelial wall into the bloodstream. Enzymes: break down carbs, proteins, and fats into sugars, amino acids, & fatty acids This is where most nutrients are absorbed in the digestive system Large Intestine Large Intestine: serves to compact the solids remaining after digestion. • Lacks villi: little to no absorption of nutrients • Water and a few ions (e.g. sodium) are absorbed through the walls of intestine; only sig. secretion is mucous • Undigested material then passes into the rectum and is finally eliminated through the anus. Sections of the Large Intestine Cecum: beginning of the large intestine; receives chyme from the ileum, and connects to the ascending colon; appendix attached Ascending Colon: begin the process of extracting water and electrolytes; peristalsis required to move up to transverse colon Transverse Colon: attached to the stomach by a wide band of tissue called the greater omentum; mobile section Descending Colon: store undigested wastes before moving into the rectum; IBS and colon cancer most common here Sigmoid Colon: s-shaped; walls are muscular and contract to increase pressure inside the colon to move wastes into the rectum Rectum: final straight portion of the large intestine; acts as a temporary storage site for undigested wastes; stretch receptors located in the walls Ailments & Diseases of the Digestive System Dysphagia: difficulty swallowing; common in old age or after a stroke/nervous system malfunction Gastroesophageal Reflux Disease (GERD): stomach contents leak backwards from the stomach into the esophagus irritating the esophagus, causing heartburn Crohn’s Disease: type of inflammatory bowel disease (IBD) that may affect any part of the gastrointestinal tract; primarily causes abdominal pain, diarrhea, vomiting, or weight loss; caused by interactions between environmental, immunological and bacterial factors in genetically susceptible individuals Ulcers: Peptic ulcers are holes/breaks in the lining of the duodenum or the stomach, areas that come into contact with stomach acids and enzymes. Duodenal ulcers are more common than stomach ulcers; recent theory holds that bacterial infection is the primary cause is the bacterium Helicobacter pylori (H. pylori) Celiac Disease: a disease that damages the small intestine and interferes with absorption of nutrients from food. Cannot tolerate gluten, a protein in wheat, rye, and barley. Gluten is found mainly in foods but may also be found in everyday products such as medicines, vitamins, and lip balms. Ulcerative colitis: a chronic, long-lasting disease that causes inflammation and sores (ulcers) in the lining of the large intestine, especially the colon and rectum Irritable Bowel Syndrome (IBS): a common disorder that affects the large intestine (colon); commonly causes cramping, abdominal pain, bloating gas, diarrhea and constipation Diverticulosis: small pouches may form along the walls of the large intestine called diverticuli; may collect and not be able to empty fecal material which can lead to inflammation Jaundice: “yellow” in french; backup of bile by-products from the blood into body tissues. May result from blockage of the ducts draining bile into the intestines Gallstones: hard, pebble-like deposits that form inside the gallbladder; may lead to inflammatory condition characterized by retention of bile in the gallbladder Cirrhosis: is scarring of the liver and poor liver function. It is the final phase of chronic liver disease; most commonly caused by alcoholism, hepatitis B and hepatitis C Hepatitis: inflammation of the liver; viruses cause most cases of hepatitis. Drug or alcohol use can also cause hepatitis. In other cases, your body mistakenly attacks healthy cells in the liver. • A - hepatitis A virus (HAV); usually spread by eating or drinking food or water contaminated with infected feces, undercook shellfish, or close contact with an infectious person. After a single infection a person is immune for the rest of their life. • B - hepatitis B virus (HBV); transmitted by exposure to infectious blood or body fluids; causes liver inflammation, vomiting, jaundice, and, rarely, death. Chronic hepatitis B may eventually cause cirrhosis and liver cancer. • C - hepatitis C virus (HCV); spread primarily by blood-to-blood contact associated with intravenous drug use, poorly sterilized medical equipment, and transfusions; often asymptomatic, but chronic infection can lead to scarring of the liver and ultimately to cirrhosis, liver failure, or liver cancer. Vaccines are readily available in developed countries