The Sports Medicine Team - Florida International University
advertisement

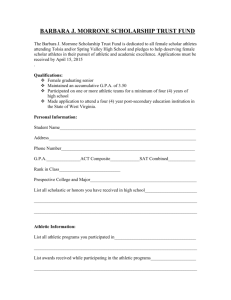
Chapter 1: The Athletic Trainer and the Sports Medicine Team Jennifer L. Doherty, MS, LAT, ATC Academic Program Director, Entry-Level ATEP Florida International University Acute Care and Injury Prevention Sports Medicine • Broad field of medical practices related to physical activity and sport • Involves a number of specialties involving active populations • Typically classified as relating to performance enhancement or injury care and management Human Performance Injury Management Exercise Physiology Practice of Medicine Biomechanics Sports Physical Therapy Sport Psychology Athletic Training Sports Nutrition Sports Massage The Players on the Sports Medicine Team • • • • • • • • • • • Physicians Dentist Podiatrist Nurse Physicians Assistant Physical Therapist Athletic Trainer Massage Therapist Ophthalmologist Dermatologist Gynecologist • • • • • • • • • • Exercise Physiologist Biomechanist Nutritionist Sport Psychologist Coaches Strength & Conditioning Specialist Social Worker Neurologist Osteopath Psychiatrist Growth of Professional Sports Medicine Organizations • • • • • • • International Federation of Sports Medicine (1928) American Academy of Family Physicians (1947) National Athletic Trainers Association (1950) American College of Sports Medicine (1954) American Orthopaedic Society for Sports Medicine (1972) National Strength and Conditioning Association (1978) American Academy of Pediatrics, Sports Committee (1979) • Sports Physical Therapy Section of APTA (1981) • NCAA Committee on Competitive Safeguards and Medical Aspects of Sports (1985) National Athletic Trainers’ Association (NATA) • Purpose: – To enhance the quality of health care for athletes and those engaged in physical activity, and to advance the profession of athletic training through education and research in the prevention, evaluation, management and rehabilitation of injuries • 30,000 members Purpose of Professional Sports Medicine Organizations • Promote involvement of various health related professions – Dentistry, podiatry, chiropractic medicine • Focus on athletic health and safety • All bodies have worked towards the reduction of injury and illness in sport Sports Medicine Journals • A variety of publications exist, providing excellent resources to the sports medicine community – – – – – – Journal of Athletic Training Journal of Sports Rehabilitation International Journal of Sports Medicine Physician and Sports Medicine Clinics in Sports Medicine American Journal of Sports Medicine The Athletic Trainer • Charged with injury prevention and health care provision for the athlete and physically active population – Consists of athletic, recreational or competitive activities – Requires physical skills and utilizes strength, power, endurance, speed, flexibility, range of motion and agility • Athletic trainer deals with the athlete and injury from its inception until the athlete returns to full competition Roles and Responsibilities: Performance Domains • • • • Prevention of athletic injuries Clinical evaluation and diagnosis Immediate care of injuries Treatment, rehabilitation and reconditioning of athletic injuries • Health care administration • Professional responsibilities Personal Qualities of ATCs • Stamina and Adaptability – Prevents burnout • Empathy – Ability to detect stress with a desire to minimize that stress • Sense of Humor – Helps relieve tension and promote relaxation Personal Qualities of ATCs • Ability to Communicate – Oral and written communication is necessary • Intellectual Curiosity – Lifelong commitment to learning • Ethics – High standard of conduct and integrity The ATC and the Athlete • Major concern for the ATC = athlete • All decisions impact the athlete • The injured athlete must always be informed – Be made aware of the how, when and why that dictates the course of injury rehabilitation The ATC and the Athlete • The athlete must be educated about injury prevention and management • Instructions should be provided regarding training and conditioning • Inform the athlete to listen to his/her body in order to prevent injuries The ATC and Parents • ATC must keep parents informed, – Particularly in the secondary school setting • The parents decision regarding healthcare must be a primary consideration • Insurance plans may dictate care – Selection of physician The ATC and Parents • ATC, physician and coaches must be aware and inform parents of Health Insurance Portability and Accountability Act (HIPAA) – Regulates dissemination of health information – Protects patient’s privacy and limits the people who could gain access to medical records The ATC and the Team Physician • ATC works under the direct supervision of a physician • Physician and ATC must be able to work together – Have similar philosophical opinions regarding injury management • Helps to minimize discrepancies and inconsistencies Roles and Responsibilities of the Team Physician • Compiling medical histories and conducting physical exams – Pre-participation screening • Diagnosing injury • Deciding on disqualifications – Based on medical knowledge and psychophysiological demands of the sport Roles and Responsibilities of the Team Physician • Attending practice and games • Commitment to sports and athletes • Potentially serve as the ATEP Medical Director – Provides input into educational content – Provides programmatic instruction The ATC and the Coach • Must understand the role of the ATC • Coach must clearly understand the limits of their ability to function as a healthcare provider • Directly responsible for injury prevention – Appropriate conditioning programs Roles and Responsibilities of the Team Physician • Coach must be aware of risks associated with the sport • Provide appropriate training and equipment • Must have knowledge of CPR and first aid • Must have thorough knowledge of skills, techniques, and environmental factors associated with sport • Develop good working relationships with staff, including athletic trainers Athletic Training • Where have we been? • Where are we now? • Where are we going? Athletic Training: Where have we been clinically? • Traditional employment settings deal exclusively with an athletic population: – Colleges – Secondary schools Athletic Training: Where are we now clinically? • Today, ATCs work in a variety of settings – – – – – – – Professional sports Hospitals Clinics Industrial settings The military Equipment sales Physician extenders Athletic Training: Where are going clinically? • Employment opportunities are becoming increasingly diverse – Dramatic transformation since 1950 – Due largely in part to the efforts of the NATA • More employment settings will include: – Research – Administration Athletic Training: Where are we going clinically? • Evolution of the profession has led to: – Recognition of ATC’s as healthcare providers – Increased diversity of practice settings – Passage of practice acts – Third party reimbursement for athletic trainers – Constant revision and reform of athletic training education Athletic Training: Where have we been educationally? • Formerly there were two types of athletic training education programs – Accredited education programs • Competency-based education – Internship education programs • Quantity-based education Athletic Training: Where are we now educationally? • In 1998, the NATA - Education Council was established to dictate the educational preparation for the athletic training student • Focus has shifted to competency based education at the entry level • Education Council has significantly expanded and reorganized the clinical competencies and proficiencies Athletic Training Education Competencies Twelve Content Areas – Risk management – Pathology of injuries and illnesses – Assessment and evaluation – Acute care – Pharmacological aspects of injury and illness – Therapeutic modalities – Therapeutic exercise – General medical conditions and disabilities – Nutritional aspects of injury and illnesses – Psychosocial intervention and referral – Organization and administration – Professional responsibilities Athletic Training: Where are we now educationally? • June 1990 – the AMA officially recognized athletic training as an allied health profession • Committee on Allied Health Education and Accreditation (CAHEA) was charged with developing the guidelines for academic programs to use in preparation of individuals for entry into profession through the Joint Review Committee on Athletic Training (JRCAT) Athletic Training: Where are we now educationally? • June 1994 - CAHEA dissolved • Replaced immediately by the Commission on Accreditation of Allied Health Education Programs (CAAHEP) – Recognized as an accreditation agency for allied health education programs by the U.S. Department of Education • Entry level college and university athletic training education programs at both undergraduate and graduate levels are currently accredited by CAAHEP Athletic Training: Where are we going educationally? • In 2003, JRC-AT became an independent accrediting agency – New name: Commission on the Accreditation of Athletic Training Education (CAATE) • CAATE will accredit athletic training education programs without – No involvement from CAAHEP Athletic Training: Where are we going educationally? • CAATE will seek affiliation with CHEA once it is fully independent – CHEA is a private nonprofit national organization that coordinates accreditation activity in the United States • Recognition by CHEA will put CAATE on the same level as other national accreditors, such as CAAHEP • CAAHEP accreditation will be discontinued in 2006; CAATE will begin in 2007 Athletic Training: Where are we going educationally? • Specialty Certifications – Build on entry level knowledge • NATA is in the process of developing specialty certifications – Further enhance professional development – Aid in expanding scope of practice Athletic Training: Where are we going educationally? • Seven proposed specialty certifications – Business practice, medical care management, occupational health, wellness, pediatric/adolescent health, adult/geriatric health, special health populations • Candidates will have to complete experiential requirements and pass a standardized examination Requirements for Certification as an Athletic Trainer • Must have extensive background in formal academic preparation and supervised clinical experience • Upon meeting the educational guidelines applicants are eligible to sit for the Board of Certification (BOC) examination BOC Examination • Examination consist of the following: – Written portion – Practical portion – Written simulation • Exam assesses the 6 domains – Prevention of injuries – Evaluation and diagnosis – Immediate care of injuries – Treatment, rehabilitation & reconditioning – Organization and administration – Professional responsibility BOC Examination • Upon passing BOC examination, you are a BOC certified athletic trainer – Credential of ATC • BOC certification is a prerequisite for licensure in most states Continuing Education Requirements • Continuing education is a requirement to maintain the ATC credential • Ensure ongoing professional growth and involvement • Requirements that must be met to remain certified – 80 CEU’s over the course of three years • Purpose: – To encourage ATC to obtain current professional development information – To explore new knowledge in specific areas – To master new athletic training related skill and techniques – To expand approaches to effective athletic training – To further develop professional judgement – To conduct professional practice in an ethical and appropriate manner • CEU’s are awarded for: – Attending symposiums, workshops, seminars – Serving as a speaker or panelist – Certification exam model – Participating in the USOC program – Authoring a research article; authoring/editing a textbook – Completing post-graduate work – Obtaining CPR and first aid certification State Regulation of the Athletic Trainer • During the early-1970s NATA realized the necessity of obtaining some type of official recognition by other medical allied health organizations of the athletic trainer as a health care professional • Laws and statutes specifically governing the practice of athletic training were nonexistent in virtually every state • Athletic trainers in many individual states organized efforts to secure recognition by seeking some type of regulation of the athletic trainer by state licensing agencies • To date 40 of the 50 states have enacted some type of regulatory statute governing the practice of athletic training • Rules and regulations governing the practice of athletic training vary tremendously from state to state Licensure • Regulation may be in the form of Licensure – Limits practice of athletic training to those who have met minimal requirements established by a state licensing board – Limits the number of individuals who can perform functions related to athletic training as dictated by the practice act • Most restrictive of all forms of regulation Certification • Regulation may be in the form of Certification – Does not restrict using the title of athletic trainer to those certified by the state – Can restrict performance of athletic training functions to only those individuals who are certified Registration • Regulation may be in the form of Registration – Before an individual can practice athletic training he/she must register in that state – Individual has paid a fee for being placed on an existing list of practitioners but says nothing about competency Exemption • Regulation may be in the form of Exemption – State recognizes that an athletic trainer performs similar functions to other licensed professions (e.g. physical therapy), yet still allows them to practice athletic training despite the fact that they do not comply with the practice acts of other regulated professions Future Directions for the ATC Determined by the efforts of the NATA and its membership… • Ongoing re-evaluation, revision and reform of athletic training education • CAATE will become an accrediting agency • Third party billing will gradually become the rule, not the exception for ATC’s • Standardization of state practice acts • ATC’s will seek specialty certifications – Expanding breadth and scope of practice Future Directions for ATC • Increase in secondary school employment • Increase in recognition of ATC as a physician extender • Potential for expansion in the military, industry, and fitness/wellness settings • With general population aging, there may be increased opportunity to work with aging physically active individuals • Continue to enhance visibility through research and scholarly publication Future Directions for ATC • Continue to be available for local and community meetings to discuss healthcare of the athlete • Increase recognition and presence internationally • Most importantly, continue to focus efforts on injury prevention and to provided high quality healthcare to physically active individuals who are injured while participating in sport