Damage Control Resuscitation and EGDTT
advertisement

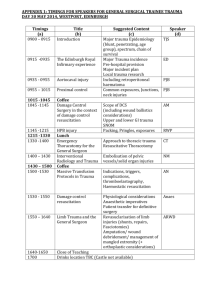
Damage Control Resusc: toward an EGDT for trauma Lanny Littlejohn CDR MC (FS/UMO/DMO) USN NMCP Dept of Emergency Medicine Cases to Consider • 21 yo male with GSW to proximal thigh on the Eastern Shore of Virginia – Airevac from facility without surgical coverage – 120 28 90/70, continued moderate bleeding, becoming altered. – ETA 25 min (helo just dispatched) • 18 yo male with GSW to mid abdomen – Hunting accident, shows up on your doorstep at a small ED. – 130 30 74/p Plan of Attack 1 Historical highlights in trauma resuscitation 2 Changes and Current Practice at Trauma Ctrs 3 New Trends of Critical Importance 4 Future Directions in Trauma Resuscitation Conclusion Fluid Resucitation Tourniquets Terminology • KIA • DOW • CFR Killed in Action Died of Wounds Combination of above • Levels of Care – – – – – I II III IV V Resuscitative Damage Control Surgery Definitive Surgery in theatre OCONUS, Landstuhl Large MTF CONUS Historical Background WWI WWII Korea “When a patient must wait for a considerable period, elevation of his systolic blood pressure to approximately 85 mmHg is all that is necessary…and when profuse internal bleeding is present, it is wasteful of time and blood to attempt to get the Bleeding Control patient’s blood pressureAggressive up to normal.” Permissive Hypotension Hemostatic Resuscitation Vietnam ARDS ACS OIF OEF Cannon W, Fraser J, Cowell E. The Preventative Treatment of Wound Shock. JAMA 1918:618-621 Tactical Combat Casualty Care • Recognition that ATLS is inappropriate in the combat setting • Focused on 3 preventable causes of combat death • Combined Good Medicine with Good Tactics • Divided the appropriate care into 3 phases • Care under Fire (CUF) • Tactical Field Care (TFC) • Tactical Evacuation (TACEVAC) TCCC in the 75th Ranger Regiment Eliminating Preventable Death on the Battlefield, Arch Surg 2011 • All personnel trained in TCCC • All training conducted with built-in TCCC scenarios • Substantial prehospital care provided by nonmedical personnel • 419 casualties, 32 fatalities • None were from preventable causes in the prehospital setting The classic ATLS resuscitative algorithm • If vitals abnormal, give one bolus crystalloid • Reassess, if still hypotensive or transiently responds, give another • PRBC’s after 2nd bolus of crystalloid • Cont to monitor coags (PT/PTT/INR) until they are 1.5 times normal and then begin correcting • FFP, Cryoprecipitate, Platelets • What is the problem with this approach? Advanced Trauma Life Support, 8th edition, the evidence for change J Trauma 2008 • One safe way of providing initial assessment and care • “The ATLS course will not be at the sharp edge of changes in trauma assessment, resuscitation, and adoption of new technology.” • Common baseline • Still recommends crystalloid resuscitation but allows for permissive hypotension. Current Practice at Civilian Trauma Centers • In the last 5 years the approach to MT has undergone a renaissance • Of victims of trauma, 8-10% will receive a blood transfusion • Of those…10% will need a massive transfusion – What is a MT? • What is Hemostatic Resuscitation (HR)? • DCR? • Survival benefit of high plasma:rbc appears to be primarily in truncal hemorrhage • Penetrating truncal trauma with noncompressible hemorrhage is the most common cause of potentially preventable death in US casualties Current Practice of MT Protocol • Activation by attending or fellow (Surg, Anesth, EM, CC) • Blood sample immed sent, bank sends – 6u O PRBC – 6u AB Plasma (some centers remains frozen) • • • • Bank continues to send packs q 30 min w plt Aggressive use of Cryo is emphasized (10u) Calcium is also emphasized If bleeding remains uncontrolled in the OR, FVIIa is made available • • • • Why is 1:1:1 theoretically better than the old way? Evidence is still flawed Physiologic evidence is strong Critically injured patients are losing whole blood The coagulopathy of trauma is real and multifactorial – – – – – – Traumatic event itself (strongly inflammatory) Consumption Hypothermia Acidosis Iatrogenic (dilutional) Overall, Coagulopathy is present in 25-38% and assoc w 6 fold increase in mortality Now for some random thoughts • Which specialty is the initial resuscitative SME? • The Problem with Trauma Research – Why have we been going in circles for more than a century • Damage Control Resuscitation – TXA – Plasma The Resuscitative Experts • We are the resuscitative experts for all conditions • We must know as much as the trauma surgeon in the initial resuscitation of hemorrhagic shock • A recent study reports that 25% of the US population now lives farther from a trauma center • 1981-1991: 66 centers had closed • 1990-2005: 339 more centers had closed • More and more trauma is being managed nonoperatively Difficulties with Trauma Research • Best evidence is based on animal research • Human evidence is predominantly retrospective and suffers many inherent biases • Survival bias present in most HR studies • Selection bias • Academic bias • Evidence follows a pyramid as it progresses Ideas, editorials, opinions Case reports, Case series, case-control Cohort studies and then finally, RCTs IV Crystalloid Resuscitation • Still important component of ATLS • Rationale for administering IVF’s in patients prior to definitive control of hemorrhage has been challenged repeatedly for almost a century • No scientific evidence to support this • Evidence does show that conventional resuscitation exacerbates the underlying cellular injury • Hemorrhage related deaths primarily occur in first 6 hours, thus early resusc needs more precision Damage Control Resuscitation • Becoming standard of care in Trauma Centers • Combines limited prehospital fluids with early blood component resuscitation • Goal is to prevent the lethal triad • Outcomes can be improved if – Hemorrhage is controlled early – Permissive hypotension is followed for penetrating trauma – Hemostatic resuscitation vs Crystalloid – TXA is given in appropriate settings Is there good evidence? • Hemorrhage control – DO2 = CO X 1.34Hgb X SaO2 + 0.003paO2 • Permissive hypotension/Delayed Resuscitation – Bickel, Immediate vs Delayed, NEJM, 1994 • Hemostatic Resuscitation • Tranexamic Acid (TXA) Tranexamic Acid • Antifibrinolytic – Inhibits plasminogen activation and plasmin activity – “Clot stabilizer” – Fibrinolysis is huge in the Coagulopathy of Trauma • Thought similar to minimizing crystalloid resusc to avoid disruption of soft thrombus • Only recently being looked at for trauma – CRASH 2 (Lancet, 2010) – MATTERS (pending) The Academic Bias • CRASH2 showed a statistically significant reduction in death due to bleeding w a NNT of 67 • RCT; n 20,211; 274 centers; 40 countries • Criticisms were many, including the fact that the benefit was overstated due to lack of sophisticated trauma systems in many centers • NO mention that one exclusion criteria were those patients who would have clearly benefitted • NO mention that the population at risk for death was much smaller than the overall study population TXA makes sense • Hyperfibrinolysis is an early component of traumatic coagulopathy • Thus, earlier use of TXA should decrease bleeding Tranexamic acid decreases mortality following wartime injury: the Military Application of Tranexamic acid in • MATTERS: Trauma Emergency Resuscitation Study – – – – Retrospective TXA group more severely injured TXA group had lower mortality TXA independently assoc with survival in MT group Some thoughts from the CoTCCC • Majority of potentially survivable deaths are due to hemorrhage in the combat setting • 25% of the 6000 deaths in OIF and OEF had potentially survivable injuries (1500) • If benefit from TXA is indeed 1.5% – 23 lives would have been saved – Cost per life saved $5200 – One dose TXA = $39.12 Plasma as the primary fluid • Problems with crystalloids • Problems with colloids • Plasma has several benefits over both – – – – – – Expands plasma volume Replaces lost coagulation proteins Contains about 400 mg fibrinogen 50 times the buffering capacity of NS Is not pro-inflammatory Problem: FFP takes time to be thawed Latest push now is the use of Freeze Dried Plama instead of FFP in the combat setting. Time to reconstitute and adminster is 5-10 min Plasma Prehospital? • Actually being done at Mayo Clinic and Memorial Hermann Hospital in Houston • Use of prehospital plasma achieves 1:1 at 30m • Thus first plasma is received 131 m sooner • In animal models, plasma improves survival over hextend even without red cell transfusion FDP (Lyophilized Plasma) • • • • No cold chain requirements Better flexibility as to where it can be given Constituted when needed (approx 2 min) Has been stored up to 30 years without altering efficacy Lessons Learned for Civilian Practice • 21 yo male shot in the groin by handgun on Virginia’s Eastern Shore • Stabilized in ED, dressing applied, 1 L LR given for hypotension • Bleeding resumes through bandages during flight • Presents in trauma bay combative, hypotensive again, bleeding uncontrolled from SFA transection • Admitted, repaired, dies from MOFS HD#3 Lessons Learned for Civilian Practice • 18 yo male with GSW to the Abdomen, brother brings him in. • You are at facility without surgical coverage. • 120 92/76 28 98% Cool, sweaty, pale • TXA • Hemostatic Resuscitation – Early plasma – Permissive hypotension Future Directions: These shock conditions are not the same • Septic shock char by: – – – – Closed Dilated High flow, low pressure With infection as the primary etiology • Hemorrhagic shock char by: – – – – Open Constricted Low flow, low pressure With hemorrhage as the primary etiology Future Directions • In sepsis we tended to under-resuscitate and EGDT helped us to focus on specific endpoints and early source control • In trauma we tend to over-resuscitate and EGDT for trauma is needed for: – Source control • Stop extremity hemorrhage (TQ, HA) • Stabilize clot formation (TXA) • Avoid the lethal triad (no crystalloids, hypothermia prevention, early plasma protocols) – Resuscitate to both specific hemodynamic and coagulation system endpoints. Predicting the need for MT • Dente, J Trauma 2010 – Transpelvic and Multicavity wounds – Combination of SBP<90 and Base deficit <-10 • Sihler, Chest 2009 : 4 independent predictors – HR>105 – SBP<110 – pH<7.25 – Hct<32 • ABC Score (Assessment of Blood Consumption) – Penetrating mechanism – Hypotension – Tachycardia – Positive FAST Once the need for MT is predicted • • • • • • • Control obvious severe hemorrhage Primary assessment simultaneously with FAST Activate protocol Send basic labs and order CXR TXA Plasma (FDP?) and RBC’s Tailor to TEG in major trauma centers Thromboelastography • R value: Reaction time – Time until first evidence of clot is detected (initial fibrin formation) • K value – The speed of clot formation (clot kinetics) • Alpha Angle – Rapidity of fibrin build up • MA: Maximum Amplitude – Strength of the clot • Coagulation Index: takes into account all 4 values Thromboelastography Questions Your Text here Your Text here Your Text here Your Text here Your Text Your Text Your Text here here here Your Text here Your Text here Your Text here Your Text here Your Text here Your Text here Your Text here Text Your Text here Your Text here Your Text here Your Text here Your Text here Your Text here Duis autem vel eum iriure dolor in hendrerit in vulputate velit esse molestie consequat, vel illum dolore eu feugiat nulla facilisis . Your Text here Your Text here Your Text here Your Text Click to add text Your Text Your Text •Add text 1 •Add text 2 Your Text Your Text Your Text Your Text Text Text Text Add Title Text Text Text Text 1 Add text 1 Add text 2 Add text 3 Add text 4 Add text 5 Text 2 Text 3 Text 4 Text 5 Text 6 1 2 3 Click to add text Click to add text Click to add text •Add •Add •Add •Add •Add •Add •Add •Add •Add •Add •Add •Add •Add •Add •Add text text text text text 1 2 3 4 5 text text text text text 1 2 3 4 5 text text text text text 1 2 3 4 5 120 30 100 80 23 60 88 40 2 3 A 25 1 33 20 10 0 65 30 30 20 4 B 5 1 1 1 1 Add Your Text here Text 2 Text 3 Text 1 Text 4 Text 6 Text 5