Chapter 20 The Cardiovascular System
advertisement

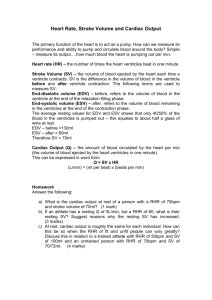
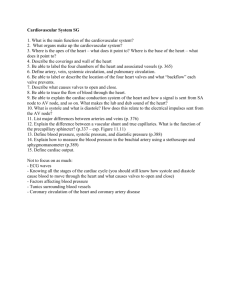
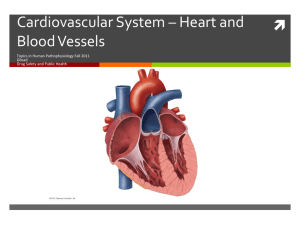
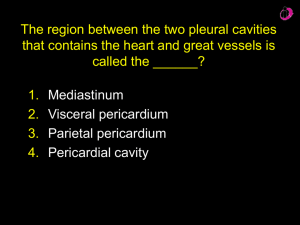
Chapter 20 - The Heart Location and Size of Heart Located in thoracic cavity in mediastinum About same size as closed fist base is the wider anterior portion apex is tip or point Pericardium: Heart Covering Fibrous Pericardium Rests on and is attached to diaphragm Tough, inelastic sac of fibrous connective tissue Continuous with blood vessels entering, leaving heart at base Protects, anchors heart, prevents overstretching Parietal (Outer) Serous Pericardium Thin layer adhered to inside of fibrous pericardium Secretes serous (watery) lubricating fluid Pericardial Cavity Contains pericardial (serous) fluid lubricates surface of parietal and visceral serous pericardium decreases friction Visceral (Inner) Serous Pericardium Adheres to Heart Forms epicardium Secretes watery (serous) lubricating fluid Pericardium Homeostatic Imbalances Pericarditis inflammation of pericardium painful, rubbing of tissues can damage myocardium Cardiac tamponade a buildup of pericardial fluid bleeding into pericardial cavity may result in cardiac failure Heart wall - Three layers Epicardium (outer) visceral layer of pericardium thin, transparent smooth, slippery Myocardium (middle) cardiac muscle Endocardium (inner) endothelium over connective tissue smooth lining for inside of heart, valves continuous w/ endothelium of vessels Chambers of the Heart External landmarks coronary sulcus separates atria/ventricles anterior/posterior interventricular sulcus separates right/left ventricles Internally - 4 compartments R/L atrium w/ auricles R/L ventricles Interatrial septum separates atria Interventricular septum separates ventricles Ventricular thickness varies depending on function Right – pumps to lungs (pulmonary circulation) Left – pumps to the body (systemic circulation) Valves of the Heart Function to prevent backflow of blood into/through heart Open, close in response to changes in pressure in heart Four valves Valve Structure Dense connective tissue covered by endocardium AV valves chordae tendineae - thin fibrous cords connect valves to papillary muscles Valve Function Opening and closing a passive process when pressure low, valves open, flow occurs with ventricular contraction, pressure increases papillary muscles contract, prevent valves from pushing back into atria Atrioventricular (AV) valves Separate atria, ventricles tricuspid valve - right bicuspid (mitral) valve - left Semilunar valves In arteries that exit heart to prevent blood from re-entering heart pulmonary semilunar valves aortic semilunar valves Pathologies incompetent – do not close stenosis – stiff and do not close Blood Flow Through Heart Right atrium (RA) receives deoxygenated blood from three sources superior vena cava (SVC) inferior vena cava (IVC) coronary sinus Right ventricle (RV) receives blood from RA pumps to lungs Pulmonary trunk - from RV branches into pulmonary arteries (PA) Pulmonary arteries from heart to lungs for gas exchange right and left branches for each lung blood gives up CO2 and picks up O2 Pulmonary veins (PV) oxygenated blood from lungs to heart Pulmonary Circulation Left atria receives blood from PV pumps to left ventricle Left ventricle (LV) sends blood to body via ascending aorta aortic arch curls over heart three branches off of it that feed superior portion of body thoracic aorta abdominal aorta Myocardial Blood Supply Myocardium has own blood supply coronary vessels diffusion into tissue impossible due to thickness much overlap of vessels and anastomoses (art-art connections) Heart can survive on 1015% of normal arterial blood flow Arteries left coronary artery divides into anterior interventricular artery and circumflex arteries anterior interventricular artery supplies walls of both ventricles and septum circumflex supplies LV and LA right coronary artery small branches to RA, divides into posterior interventricular and marginal artery posterior interventricular supplies walls of both ventricles marginal branch supplies RV Coronary veins blood into muscle then drains into coronary sinus supplied by great cardiac vein (drains anterior of heart) and middle cardiac vein (drains posterior) Coronary Circulation Pathologies Faulty coronary circulation due to: blood clots fatty atherosclerotic plaques smooth muscle spasms in coronary arteries Problems ischemia hypoxia Pathologies (cont.) Angina pectoris - "strangled chest" pain w/ myocardial ischemia - referred pain! tight/squeezing sensation in chest labored breathing, weakness, dizziness, perspiration, foreboding often during exertion - climbing stairs, etc silent myocardial ischemia Pathologies (cont.) Myocardial infarction (MI) - heart attack thrombus/embolus in coronary artery tissue distal to blockage dies if survival, muscle replaced by scar tissue Long term results size of infarct, position pumping efficiency? conduction efficiency, heart rhythm Pathologies (cont.) Treatment clot-dissolving agents angioplasty Reperfusion damage re-establishing blood flow may damage tissue oxygen free radicals - electrically charged molecules w/ unpaired electron radicals attack proteins (enzymes), neurotransmitters, nucleic acids, plasma membranes further damage to previously undamaged tissue or already damaged tissue Myocardium (Cardiac Muscle) Cells are involuntary, striated, branched Fibers connected to others by intercalated discs gap junctions allow AP's to pass from fiber to fiber desmosomes “spot welds” prevent cardiac fibers from separating Intercalated Discs Normal Action Potential Cardiac Muscle Action Potential Long absolute refractory period Pacemaker potentials Leaky membranes Spontaneously depolarize Conduction System and Pacemakers Autorhythmic cells cardiac cells repeatedly fire spontaneous action potentials autorhythmic cells: the conduction system pacemakers SA node origin of cardiac excitation fires 60-100/min AV node conduction system AV bundle of His R and L bundle branches Purkinje fibers Conduction System and Pacemakers Arrhythmias irregular rhythm abnormal atrial and ventricular contractions Fibrillation rapid, out of phase contractions squirming bag of worms Ectopic pacemakers (ectopic focus) abnormal pacemaker controlling the heart SA node damage, caffeine, nicotine, electrolyte imbalances, hypoxia, toxic reactions to drugs Heart block AV node damage - severity determines outcome may slow conduction or block it Conduction System and Pacemakers SA node damage (MI) AV node can run things (40-50 bts/min) if AV node out AV bundle, bundle branch/conduction fibers fire at 20-40 bts/min Artificial pacemakers - can be activity dependent Atrial,Ventricular Excitation Timing SA node to AV node - small delay about 0.05 sec from SA to AV, 0.1 sec to get through AV node conduction slows allows atria time to finish contraction and better fill the ventricles once to AV bundle, conduction rapid to rest of ventricle Extrinsic Control of Heart Rate Basic rhythm of heart set by pacemaker system Central control from medulla sympathetic input parasympathetic input Electrocardiogram Electrical activity of the heart P wave QRS complex T wave Cardiac Cycle Connection between electrical and mechanical events Systole Diastole Isovolumetric contraction Isovolumetric relaxation Quiz!!!!! 1. Superior vena cava 2. Right atrium 3. Tricuspid valve 4. Right ventricle 5. Papillary muscle 6. Aorta (aortic arch) 7. Pulmonary trunk 8. Left atrium 9. Bicuspid valve 10. Interventricular septum Cardiac Output Amount of blood pumped by each ventricle in 1 minute CO = HR x SV HR heart rate 70 bts/min SV stroke volume 70 ml/min CO 5 L/min (70 bts x 70 ml) Regulation of Stroke Volume SV = EDV – ESV EDV End Diastolic Volume volume of blood in the heart after it fills (following diastole) 120 ml ESV End Systolic Volume volume of blood in the heart after contraction (after systole) 50 ml each beat ejects about 60% of blood in ventricle Most important factors in regulating SV: preload, contractility and afterload Preload degree of stretch of cardiac muscle cells before contraction determined by EDV Contractility increase in contractile strength separate from stretch and EDV determined by changes in Ca++ availability Afterload pressure that must be overcome for ventricles to eject blood from heart determined by TPR Preload Muscle mechanics length-tension relationship? fiber length determines # of cross bridges cross bridge # determines force increase/decrease fiber length increase/decrease force generation Cardiac muscle how is cardiac fiber length determined/regulated? fiber length determined by filling of heart – EDV factors that effect EDV (anything that effects blood return to heart) increase/decrease filling increase/decrease SV Preload – Frank-Starling Law of the Heart length tension relationship of heart length = EDV tension = SV Contractility Increase in contractile strength separate from stretch and EDV Do not change fiber length but increase contraction force? what determines force? how can we change this if we don’t change length? Increase the number of cross bridges by increasing amount of Ca++ inside the cell – positive inotrope Sympathetic nervous system opens channels to allow Ca++ to enter the cell Increase force of contraction without changing fiber length Afterload Flow = P/R If blood pressure is high (TPR), difficult for heart to eject blood More blood remains in ventricle with each beat Heart has to work harder to eject blood, change the length/tension of the heart Regulation of Heart Rate Intrinsic regulators pacemakers Bainbridge effect increase in EDV increases HR filling stretches SA node increasing depolarization and HR Extrinsic regulators autonomic nervous system sympathetic parasympathetic hormones – epinephrine, thyroxine ions – Na+, K+, Ca++ body temperature age gender exercise