Gastrointestinal Physiology, Lecture 3: The Gastric Phase of Digestion
advertisement

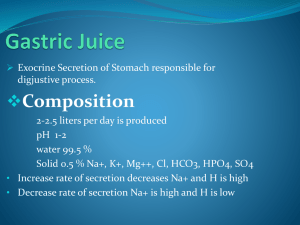
Gastrointestinal Physiology, Lecture 3: The Gastric Phase of Digestion IDP/DPT GI Section 2011 Jerome W. Breslin, PhD LSUHSC-NO Dept. of Physiology Downtown Campus, MEB 7208 (504) 568-2669 jbresl@lsuhsc.edu Required Reading Kim Barrett, Gastrointestinal Physiology: Chapter 3 Chapter 8 Three Phases of Gastric Secretion Slide number Cephalic Phase 1. The taste or smell of food, tactile sensations of food in the mouth, or even thoughts of food stimulate the medulla oblongata (green arrow). Taste or smell of food Tactile sensation in mouth 2. Parasympathetic action potentials are carried by the vagus nerves to the stomach (pink arrow). Medulla oblongata 3. Preganglionic parasympathetic 1 vagus nerve fibers stimulate postganglionic neurons in the enteric plexus of the stomach. 4. Postganglionic neurons stimulate secretion by parietal and chief cells and stimulate gastrin secretion by endocrine cells. 5 Vagus nerves 2 Secretions stimulated 3 Gastrin 4 Circulation 5. Gastrin is carried through the circulation back to the stomach (purple arrow), where it stimulates secretion by parietal and chief cells. Stomach Copyright © The McGraw-Hill Companies, Inc. Permission required for reproduction or display. GI Physiology Lecture 3 Outline: Gastric Phase of Digestion: Overview Gastric Motility - Part 1 LES Relaxation Receptive Relaxation Mixing and Grinding Gastric Secretions and Their Regulation: HCl, HCO3-, mucus, pepsin, gastrin Gastric Motility - Part 2 Gastric Emptying and its Regulation Vomiting Figure 15-16 Body (Corpus) Reservoir Function Antrum: Mixing Function The abundant smooth muscle in the stomach is responsible for gastric motility. Gastric Phase Receptive Relaxation Entry of Meal Increased Gastric Secretions Motility: Mixing and Grinding Digestion of protein, CHO, fat Gastric Emptying Figure 15-15 1. Peristalsis of bolus to the stomach 2. Opening of LES 3. Receptive relaxation in stomach The coordinated sequence of contraction and relaxation in the upper esophageal sphincter, the esophagus, and the lower esophageal sphincter is necessary to deliver swallowed food to the stomach. LES Relaxation: Neurogenic process, although the relative importance of neural inputs is not clear, and the specific neurotransmitter is unknown. Vagal stimulation causes LES relaxation. Swallowing causes LES relaxation, as well as receptive relaxation of the stomach to facilitate entry of the bolus. Gastric Motor Function during the Gastric Phase: Receptive Relaxation. Fundus and Body relax to accommodate the volume of the meal. Mixing and Grinding. Antral peristalsis to grind the meal into small particles and mix with secretions. Gastric Emptying. Coordination of antropyloro-duodenal motor activity for regulation of gastric emptying. In addition, gastric reservoir function participates by regulating fundus tone. Receptive Relaxation Swallowing causes relaxation of gastric smooth muscle. Mediated by vagus nerve. Receptive relaxation increases compliance, so that luminal pressure changes very little between the empty state (50 mL volume) and filled state (1500 mL volume). Receptive Relaxation Intrinsic and vago-vagal reflexes mediate receptive relaxation. Duodenal distension also results in relaxation of the gastric fundus. Barrett, Fig. 8-4 Mixing and Grinding Pacemaker Region induces peristaltic contraction from the body to the antrum, which closes the pyloric sphincter. Pacemaker Cells (ICC) induce slow waves (BER) ~ 3 times per minute. Force of Contraction, Regulation: Increased by gastric distension, via short reflexes and gastrin. Inhibited by 1) duodenal distension, 2) appearance of fat, protein, acid or hypertonic chyme in the duodenum 3) increased sympathetic tone. Figure 15-22 Waves of smooth muscle contraction mix and propel the ingested contents of the gastric lumen, but only a small amount of the material enters the small intestine (duodenum) as a result of each wave cycle. Motor behavior of the antral pump is initiated by the dominant pacemaker in the mid-corpus. PACEMAKER POTENTIALS DETERMINE CONTRACTILE PARAMETERS: 1. MAXIMAL FREQUENCY 2. PROPAGATION VELOCITY 3. PROPAGATION DIRECTION Barrett, Fig 8-2 BER established by the gastric pacemaker. Note that a contractile stimulus is needed to reach the threshold for gastric contractions to occur. THRESHOLD Barrett, Fig. 8-3 Gastric Secretions Oxyntic Gland Area - proximal 80% of the stomach (body and fundus) - secretes HCl and pepsinogen into stomach lumen. Pyloric Gland Area - distal 20% of the stomach (antrum) - secretes pepsinogen into the lumen, as well as the hormone gastrin to the bloodstream. Gastric Mucosa Surface - secretes mucus and HCO3 for protection from the acidic environment. Composition Of Gastric Juice Component Source Function Pepsinogen Chief Cells Inactive Protease Pepsinogen Protease (activated by HCl) HCl Parietal Cells Acid Environment Activation of Pepsin Mucus Mucous Cells Goblet Cells Viscous, Alkaline Protective Layer Parietal Cells Vitamin B12 Absorption Pepsin Intrinsic Factor HCl Secretion during the Cephalic, Gastric, and Intestinal Phases of Digestion: Figure 15-16 1. Cardia Three Regions of Stomach with Specialized Functions 2. Body & Fundus Specialized cells in the stomach synthesize and secrete mucous fluid, enzyme precursors, hydrochloric acid, and hormones. 3. Antrum & Pylorus The abundant smooth muscle in the stomach is responsible for gastric motility. Stomach Wall: Gastric Gland Mucous cells secrete mucous, HCO3-, & trefoil peptides. Chief cells secrete pepsinogen & gastric lipase. Parietal cells synthesize and secrete hydrochloric acid & intrinsic factor. ECL Cells secrete histamine. Enteroendocrine cells (specifically G cells) secrete gastrin. 25 Parietal Cells secrete HCl Resting Parietal Cell Stimulated Parietal Cell Secreting HCl Barrett, Figs 3-2 and 3-3 or Berne & Levy Fig. 32-10 Upon stimulation, the intracellular canniculi fuse to the apical membrane, and the tubulovesicles fuse to the canniculi, increasing the apical (luminal) membrane surface area 5-10 times. The tubulovesiclar membrane is a storage site for the H+/K+ ATPase. Fusion of tubulovesicles to the apical membrane increases availability of the H+/K+ ATPase for H+ secretion. • Barrett, Fig. 3-6 Regulation of HCl and pepsin secretion Potentiation A phenomenon in which the effect produced when two (or more) agents act to together is greater than the sum of their effects when they act separately. Acid Secretion in the Stomach - potentiation among the three stimuli: histamine, ACh, gastrin, such that histamine H2 receptor blockade drastically reduces acid secretion. Figure 15-19 X H2 Blockers (Pepcid, Zantac, Axid) X Atropine (not practical) One inhibitory and three stimulatory signals that alter acid secretion by parietal cells in the stomach. H/K-ATPase Inhibitors (Prilosec, Prevacid, Nexium) X X Antacids (e.g. Tums, Maalox, PeptoBismol) Figure 15-18 F O O D Acid production by the parietal cells in the stomach depends on the generation of carbonic acid; subsequent movement of hydrogen ions into the gastric lumen results from primary active transport. Note: Some of the bicarbonate secreted into the blood goes to surface epithelium, where it is taken up and then secreted in the mucus layer to protect cells. Surface epithelium secretes a mucus layer containing bicarbonate for protection from gastric acid. • Berne & Levy, Fig. 32-13 Figure 15-21 The acidity in the gastric lumen converts the protease precursor pepsinogen to pepsin; subsequent conversions occur quickly as a result of pepsin’s protease activity. Gastric Phase: Both Vago-vagal reflexes and gastrin increase HCl and pepsinogen release. Dorsal Vagal Complex Response: HCl Secretion Pepsinogen Secretion Gastrin (hormone) Vago-vagal Reflex Pepsinogen pH < 5 G Cells Pepsin Oligopeptides Proteins Distension sensed by mechanoreceptor Response: HCl Secretion Pepsinogen Secretion Gastrin Secretion Note: The ENS is also stimulated by distension. Enteroendocrine Cells and Pathways Regulating Acid Secretion: Acid in Antrum stimulates somatostatin release from D cells Cellular Mechanism of HCl Secretion: 38 Regulation of Pepsinogen Secretion: Vagus Nerve (can be activated by distension of stomach) ACh + Circulation + Secretin Secretin Gastrin G Cell + D Cell SS Peptides S Cell + H+ Parietal Cell + H+ ENS + ACh+ Proteins Pepsin + Pepsinogen H+ (SS = Somatostatin) Peptides Gastric acid output at rest and during maximal stimulation: Representative Ranges Condition Basal Acid Maximal Acid Output (mEq/h) Output (mEq/h) Normal 1-5 6 - 40 Gastric Ulcer 0-3 1 - 20 0 0 - 10 Duodenal Ulcer 2 - 10 15 - 60 Gastrin-Secreting Tumor (Zollinger-Ellison Syndrome) 10 - 30 30 - 80 Pernicious Anemia (Loss of Parietal Cells) Output = Hourly volume of gastric juice x [H+] Ulcers The cause is usually mucosal breakdown due to an infection with H. pylori. Other possible causes: Chronic use of NSAIDs, gastrinoma. Gastric Ulcer - Cause is usually breakdown of mucosa lower basal pH due to leakage of acid from stomach Duodenal Ulcer - Cause may have to do with more acid present in duodenum than normal (not clear, though) - increased parietal cell mass. Doubled HCl and pepsinogen secretion. Gastric Emptying • Gastric Distension increases emptying (rate is proportional to size of meal) • Gastric Emptying Inhibited By: – Entry of chyme into duodenum –Fat, protein digests in duodenum –Acidity (pH < 3.5) in duodenum –Hypo/hyper-osmotic chyme in duodenum –Distention of the Duodenum –Solids more inhibitory than liquids. Figure 15-24 (CCK, Secretin) Delivery of acid and nutrients into the small intestine initiates signaling that slows gastric motility and secretion which allows adequate time for digestion and absorption in the duodenum. Between meals: MMCs Vomiting VARIOUS CAUSES: antibiotics, Analgesics narcotics, cancer chemotherapy, mechanical obstruction, radiation injury, gastroparesis, functional bowel disorders, intraperitoneal inflammation, increased intracranial pressure, Emotional responses, psychiatric conditions, tumors, bayrinthine disorders, pregnancy, uremica, diabetic ketoacidosis, viral or bacterial gastroenteritis Summary: Digestion of a Meal in the Stomach Entry • • • • • • • • • Bolus Large Particles Triglycerides Protein Starch Monosaccharides Disaccharides Salivary Secretions Water and Ions Departure • Small Particles (<2 mm) • Emulsion • Triglyceride + small amount of 2-monosaccharides and free fatty acids. • Protein + small amount of peptides and amino acids. • Starch + 20% oligosaccharides • Monosaccharides • Disaccharides • Water, ions, low pH