Balance (Vestibular) Therapy
advertisement

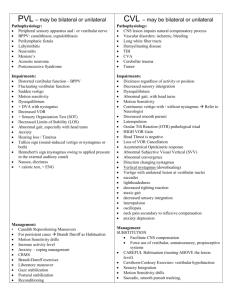
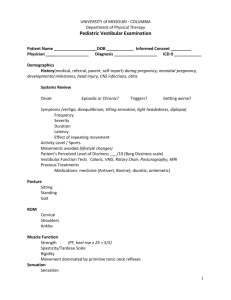
Presented by Maureen E. Gordon, PT, MSPT, CEAS Certified in Vestibular Rehabilitation Certified in Cervicogenic Dizziness Physical Therapy at St. Luke’s The brain constantly monitors the sensory information coming in and uses body movements to maintain stable posture Changes in sensory information input or motor control output require the brain to use the correct strategy Balance Integration Sensory Input Visual Vestibular Proprioceptive Central Processing Primary Processor (Vestibular Nuclear Complex) Adaptive Processor (Cerebellum) Motor Neurons Positional Movements Hip, ankle, and stepping strategies Eye Movements Peripheral Vestibular System Vestibular end organs (3 semicircular canals, 2 otolith organs) Vestibular portion of the VIIIth cranial nerve Central Vestibular System Vestibular nuclei Vestibulo-ocular pathway Vestibulospinal pathway Vestibulocollic pathway Vestibulo-autonomic pathway Vestibulocerebral pathways Primary and secondary cortical areas Vestibulocerebellum Vestibular System Function What does it do? Senses rotational movements of the head Senses linear movements of the head Senses head position in space due to gravity being a linear acceleration What does it do with that information? Postural Stability (Balance) Gaze Stability (Eye-head coordination) Orientation in Space Brain Where am I? What am I going to do? Sensory Systems Motor Patterns Environmental Interaction Generation of Body Movement Balance (Postural) Control Balance Control Gaze Stability Postural Stability Gaze Stability The ability to maintain gaze or visual focus on an external target during movement. A function of an intact VOR (vestibuloocular reflex) at speeds > 85 degrees/second. Postural Stability The ability to maintain the body’s center of gravity (COG) over the base of support (BOS) in a given sensory environment. Sensory Integration Decreased ankle proprioception Abnormal interactions between the 3 sensory systems Inappropriately relying on one system over another Excessive reliance on visual input, even when it is inaccurate Biomechanical Constraints Impaired quality and size of the base of support Anteriorly displaced center of pressure in the paretic leg Poor trunk control (Oliveira et al, 2008) Movement Strategies Compensation strategies, e.g. holding objects or walls and using stepping strategy more frequently than agematched controls Predominant use of hip strategy and use ankle strategy less Decreased anticipatory control Perception of Verticality Abnormal postural perception of verticality, especially with visuospatial neglect Resistance to support weight on nonparetic side (“pusher syndrome”) (Oliveira et al, 2008) Weakness/hemiplegia Spasticity or hypotonicity Vestibular/inner ear disturbances Affected vision and/or sensation Ataxia Decreased range of motion (ROM) Fatigue and deconditioning Pain Impaired cognition Objective Tests/Measurements Assessment of Functional Limitations Fall Risk Assessment – observational measurement tools Postural Assessment Scale for Stroke Patients Benaim, et al. 1999) (Mao, et al. 2002. Berg Balance Scale Dynamic Gait Index Assessment of Impairment Oculomotor Exam: abnormal smooth pursuit, saccades, skew deviation (Kattah, 2009) and VOR cancellation Computerized Testing, e.g. Balance Master® or Biodex® ROM and Strength Testing Sensation and Coordination Tests Assessment of Spasticity Gait Assessment Feature Peripheral Central Effect of Fixation Nystagmus decreases Nystagmus increases or stays the same Direction of Gaze Mixed plane (e.g. vertical and torsional) Usually single plane – vertical, horizontal or torsional Effect of Gaze Nystagmus increases with gaze toward the direction of the quick phase Nystagmus reverses direction or it does not change Can assess balance control with greater sensitivity than observational methods A sensory modality can be removed or attenuated and the effect of these changes in postural control can be assessed Evaluation of hemiparetic patients can show asymmetrical distribution of weight in lower limbs, difficulty in actively transferring, and impaired muscle selection (Oliveira et al, 2008) Balance Exercises – Computerized and noncomputerized training: focusing on proprioception, widening BOS, ankle strategy Neuroplasticity – if damage is done to portions of the brain effecting balance, then the goal of balance training would be to have different portions of the brain take over those functions or aid in those functions (Sawakri et al 2008) In the chronic stroke population, balance impairment and fall risk are associated with lower quality of life scores (Schmid 2013) Activities for Motor Strategies Motor learning is improved with task specificity. Therefore, if specific circumstances challenge balance, practicing those tasks are more effective than practicing general balance tasks (Klein et al) Gait Training – assistive device and bracing, as needed High intensity gait training with focus on increasing the number of steps taken throughout the day, and during PT sessions, has been proven to help balance and transfers, in addition to gait training (T George Hornby) Gait speed – important measure for fall prediction, community participation, and can be a balance measure (Beauchet et al 2008) Stretching, Strengthening, & Conditioning Adaptation Exercises – gaze stabilization/VOR exercises Home Exercise Program (HEP) Recommendations for Environmental Modification Beauchet O, et al. Recurrent falls and dual task-related decrease in walking speed: Is there a relationship? J Am Geriatr Soc 2008 Jul;56(7):1265-9 Benaim C, et al. Validation of a standardized assessment of postural control in stroke patients: The Postural Assessment Scale for Stroke Patients (PASS). Stroke 1999;30(9):1862-68 Hornby, T George from University of Illinois. Unpublished study to be presented at 2015 CSM Kattah, Jorge C, et al. HINTS to diagnose stroke in the acute vestibular syndrome: Three-step bedside oculomotor examination more sensitive than early MRI diffusion-weighted imaging. Stroke 2009;40:3504-3510 Klein et al. Principles of experience dependent neural plasticity: Implications for rehabilitation after brain damage supplement. Journal of Speech, Language, and hearing research. S1: 5225-5239 Mao HF, et al. Analysis and comparison of the psychometric propeties of three balance measures for stroke patients. Stroke 2002;33(4):1022-27 Oliveira, Clarissa Barros de, et al. Balance control in hemiparetic stroke patients: main tools for evaluation. Journal of Rehabilitation Research & Development 2008;45(8):1215-1226 Sawakri, et al. Constraint induced movement therapy results in increased motor map area in subjects 3 to 9 months after stroke. Neuro Rehab and Neuro Repair 2008, 220: 505 Schmid, AA, et al. Balance is associated with quality of life in chronic stroke. Top Stroke Rehabilitation, 2013 Jul-Aug;20(4):340-6