UVL
advertisement

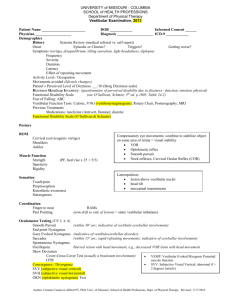
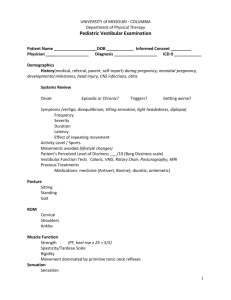
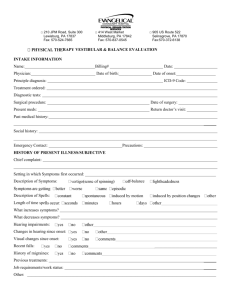
PVL – may be bilateral or unilateral CVL – may be bilateral or unilateral Pathophysiology: Peripheral sensory apparatus and / or vestibular nerve BPPV: canalithiasis, cupulolithiasis Perilymphatic fistula Labyrinthitis Neuronitis Meniere’s Acoustic neuroma Postconcussive Syndrome Pathophysiology: CNS lesion impairs natural compensatory process Vascular disorders: ischemic, bleeding Long white fiber tracts Demyelinating disease TBI CVA Cerebellar trauma Tumor Impairments: Distorted vestibular function – BPPV Fluctuating vestibular function Sudden vertigo Motion sensitivity Dysequilibrium + DVA with nystagmus Decreased VOR + Sensory Organization Test (SOT) Decreased Limits of Stability (LOS) Abnormal gait, especially with head turns Anxiety Hearing loss / Tinnitus Tullios sign (sound-induced vertigo or nystagmus or both) Hennebert's sign (nystagmus owing to applied pressure in the external auditory canal) Nausea, dizziness + caloric test, + ENG Impairments: Dizziness regardless of activity or position Decreased sensory intergration Dysequilibrium Abnormal gait, with head turns Motion Sensitivity Continuous vertigo with / without nystagmus Refer to Neurologist Decreased smooth pursuit Lateropulsion Ocular Tilt Reaction (OTR) pathological triad HIGH VOR Gain Head Thrust is negative Loss of VOR Cancellation Asymmetrical Optokinetic response Abnormal Subjective Visual Vertical (SVV) Abnormal convergence Direction changing nystagmus Vertical nystagmus (downbeating) Vertigo with unilateral lesion at vestibular nuclei saccades lightheadedness decreased righting reaction ataxic gait decreased sensory integration lateropulsion oscillopsia neck pain secondary to reflexive compensation anxiety depression Management: • Canalith Repositioning Maneuvers For persistent cases Brandt Daroff as Habituation Motion Sensitivity drills Increase activity level Anxiety – coping management CRMS Brandt-Daroff exercises Liberatory maneuver Gaze stabilization Postural stabilization Reconditioning Management: SUBSTITUTION Facilitate CNS compensation Force use of vestibular, somatosensory, propioceptive systems CAREFUL Habituation (treating ABOVE the lesion level) Cawthorn-Cooksey Exercises: vestibular hypofunction Sensory Integration Motion Sensitivity drills Saccadic, smooth pursuit tracking, Ocular ROM DVA – Dynamic Visual Acuity Retrain VSR – for postural stability (static balance, dynamic equilibrium, perturbations, motor strategies Retrain Gaze Stabilization (VORx1, VORx2, VOR Cancellation) Motion Sensitivity Quotient Conditioning exercises Flexibility Anxiety / coping management Walking program (conditioning and improve gaze stabilization) xxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxx xxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxx UVL BVL Pathophysiology: Lesion to peripheral sensory apparatus and / or vestib nuclei in pons Labryinthitis Perilymph fistula Acoustic neuroma Meniere’s disease Head trauma / labyrinthine concussion Vestibular neuritis Surgical procedure Pathophysiology: Ototoxicity Bilateral infections Age-related degeneration Meningitis Impairments: Spontaneous nystagmus with acute lesion Must make diff dx of vertigo from episodic cause, eg Meniere’s, migraine + Head Thrust (saccade to side of lesion) decreased VOR Gain + Dynamic Visual Acuity (DVA) sign + CTSIB + Sensory Organization Test (SOT) + Fukuda Abnormal gait: LOB, head turns, deviation to side Dysequilibrium Decreased Single Limb Stance (SLS), Sharpened Romberg (Tandem) Hearing loss, progressive, unilateral nystagmus postural instability tinnitus sudden vertigo, nausea + head shake + caloric test Dysequilibrium visual complaints decreased head / trunk rotation with gait anxiety, depression Impairments: No nystagmus No vertigo Dysequilibrium VOR abnormal with severe Gaze Instability Decreased Single Limb Stance (SLS), Romberg and Sharpened Romberg (Tandem) + Head Thrust occurring bilaterally + Dynamic Visual Acuity (DVA) sign + Fukuda + CTSIB + Tandem Walk (EO) Abnormal gait: head turns hearing loss oscillopsia postural instability; rigidity lightheadedness nausea wide base gait Management: ADAPTATION, Recovery, Substitution, Habituation (if chronic) VOR exercises Gaze stabilization ex. Retrain VSR (Vestibulospinal Reflex); postural stabilization Gait training Flexibility Conditioning Anxiety – coping management Increase motion tolerance Watchful waiting Meniere’s: salt restriction Post op exercise (neuroma excision, etc.) Management: SUBSTITUTION (for complete lesion), ADAPTATION (for incomplete lesion), Habituation is NOT appropriate Potentiate Cervical Ocular Reflex (COR) Use modified saccades Central pre-programming Enhance visual input, eg, spotting Somatosensory input Alternative strategies for Gaze Stabilization & Postural Control Goal: improve functional abilities rather than improvement of vestibular damage (if severe or complete lesion). Pt. education: o avoidance strategies o preplanning o appropriate shoes, floors, lighting Flexibility Conditioning Tai Chi, pool exercises Functional Actitivites ( ADL, IADL) In making a differential diagnosis, remember that PVL/CVL and UVL/BLV form a matrix. PVL UVL BVL CVL