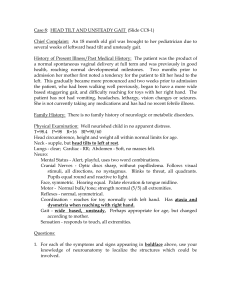
Dizziness

Jordan Smedresman
SUNY Downstate College of Medicine
Class of 2013
Suddenly started ~6 hours prior to evaluation when she stood up after dinner
Felt the room spinning, had to be supported to keep from falling
Nausea , one episode of vomiting
Similar episode one week prior, spontaneously resolved after “a few hours”
No history of trauma, no recent illness, no tinnitus
Still unsteady on her feet, but gradually improving, nausea has resolved
PMH—anemia
PSH—c-section 7 years ago
Allergies—shellfish (rash), no drugs
Meds—iron, Centrum
Temp 98.2, HR 86, RR 16, 178/107 (repeat
150/100)
Physical exam unremarkable
Alert and oriented x3
CN II-XII intact, slight horizontal nystagmus upon turning the head, worse when turning left
Muscle strength 5/5 in all extremities, normal sensation
Reflexes 2+ throughout
FTN intact
Gait unsteady, not ataxic
Upon lying flat, symptoms returned
Patient refused Dix-Hallpike test
WBC: 9.3
Hb: 12.4
Hct: 40.6
Plt: 344
MCV: 65
β-HCG: 0
T4: 1.18
TSH: 1.792
Na: 141
K: 4.2
Cl: 104
CO2: 26.6
BUN: 14
Cr: 0.6
Glucose: 104
Ca: 10.2
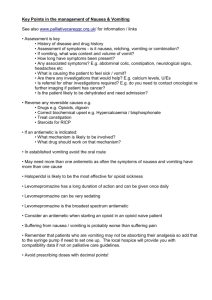
Usually multiple short (seconds) episodes reproduced by tilting the head
Often caused by canaliths
Can last weeks to months
Vomiting is rare
Diagnosed through history. Dix-Hallpike can helpful (50-80% sensitive)
Believed to be viral or postviral inflammatory disorder
Rapid onset of severe, persistent vertigo with nausea/vomiting and gait instability (fall toward affected side)
Spontaneous nystagmus
Clinical diagnosis
Usually lasts 1-2 days
Time course—vestibular neuronitis
Suggestive setting—BPPV (more predictable head movements, no recent illness)
Nystagmus—more typical of vestibular neuronitis
Treatment—meclizine with ENT followup
Second line—benzos