Bez nadpisu
advertisement

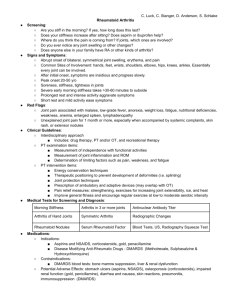
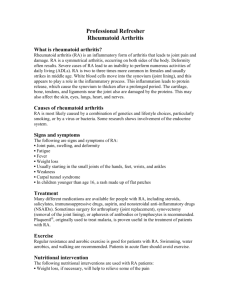
Locomotion disorders Martin Votava Treatment of locomotion disorders Skeletal Muscle Relaxants Anxiolytic Agents Nonsteroidal anti-inflammatory drugs Analgetics Slow-acting anti-rheumatic drugs Glucocorticoid drugs Chondroprotective drugs Drugs used in gout Rheumatoid Arthritis • A chronic, systemic autoimmune disease of unknown etiology • Characterized by symmetric, erosive, joint synovitis • Can be Palindromic, Relapsing, or Malignant • May involve multiple organ systems: cardiovascular, pulmonary, renal, skin and eyes Epidemiology: • • • • • Affects 1% of U.S. adults 150,000 new cases annually 80% of cases occur between 35-50 years Female-to-male ratio of ~ 3:1 Gender predisposition decreases with increasing age • Costs/year ~$8.74 billion (1994 dollars) RA Joint • Pannus formation • Tendon and ligament instability • Invasion of cartilage and bone surface • Erosion of bone and cartilage • Joint instability • Eventual destruction of the joint What diseases are considered in the differential diagnosis of RA? • • • • • • • Osteoarthritis Spondyloarthritis Gout and Pseudogout Fibromyalgia Polymyalgia Rheumatica Systemic Lupus Erythematosus Reactive Arthritis Functional Classification • Class I: capable of all activities without handicap • Class II: Able to conduct normal activities despite discomfort or limited mobility of one or more joints • Class III: Functional capacity only adequate to perform a few of the normal duties of usual occupation • Class IV: Confined to bed or wheelchair; capable of little or no self-care Rheumatoid Arthritis: Extra-articular Manifestations • • • • • Dermatologic: subcutaneous nodules Hepatic: elevated transaminases Cardiac: pericarditis Pulmonary: fibrosis, nodules, pleural effusion Ocular: keratoconjunctivitis, scleritis Rheumatoid Arthritis: Laboratory Abnormalities • Serologic Findings: Anemia, thrombocytosis, mild leukocytosis, positive RF, elevated ESR, C-reactive protein • Synovial Fluid Findings: Straw-colored and slightly cloudy fluid, leukocytosis 5,000 to 25,00/mm3, 85% polymorphonuclear cells What laboratory data is consistent with a diagnosis of RA • Anemia • Thrombocytosis • (+) Rheumatoid Factor Rheumatoid Arthritis: Treatment • Goal: – Prevent disease progression to irreversible joint damage – Maintain Quality of life • Multidisciplinary approach: – Patient education: treatment plan, compliance, understanding of disease – Psychotherapy: manage pain and stress – Rehabilitation: exercise, joint protection Non-Pharmacologic Interventions: • Goal: – Reduce pain, disability and protect mobility • • • • Physical Therapy Occupational Therapy Psychological support for the patient and family Surgical Alternatives – Synovectomy – Joint replacement Pharmacologic Interventions • Early aggressive treatment: – Control swelling and pain – Reduce the probability of irreversible joint damage • Agents: – – – – – Glucocotricoids NSAID’s DMARDs Biologic response modifiers Chondroprotective agents NSAIDs NONSTEROIDAL ANTI-INFLAMMATORY DRUGS are among the most widely used drugs major type of effects: • antiinflammatory • analgesic (reduction of somatic pain) • antipyretic (lowering of a raised temperature) mechanisms of action: inhibition of arachidonate cyclooxygenase (COX) inhibition of biosynthesis of PGs and TXs COX-1 = enzyme expressed in most tissues involved in cell-cell signalling and in tissue homeostasis COX-2 = enzyme induced in inflammatory cells when they are activated , responsible for the production of prostanoid mediators of inflammation Nonselective NSAIDs arachidonic acid physiological activation COX-1 (constitutive form) Selective and nonselective NSAIDs inflammation COX-2 Endoperoxides (inducible form) proinflammatory prostanoids prostanoids ensuring physiological functions Results from inhibition of prostanoids biosynthesis COX-2 inhibition COX-1 inhibition) Unwanted effects mainly on the GIT Antiinflammatory, analgesic and kidney, decrease in pl.aggregation and antipyretic effects Regulation and Expression of COX-1 and COX-2 COX-1 • Constitutive (Protective) • Found in all tissues • Important role in – GI tract – Kidneys – Platelets COX-2 • Induced at site of inflammation (Inducible) • Produced by macrophages, synoviocytes during inflammatory process Vane JR, Botting RM. Semin Arthritis Rheum. 1997;26:2-10. the antiinflammatory action of NSAIDs is mainly related to their inhibition of COX- 2 and it is probable that their unwanted effects are largery due to their inhibition of COX-1 All NSAIDs are analgesics and antipyretics but the degree of anti-inflammatory activity varies. OTC drugs (over the counter) Analgesic effect-- mechanisms in the periphery against pain associated with inflammation or tissues damage because of decrease in PGs production that sensitises nociceptors to inflammatory mediators (bradykinin) central mechanisms (in the spinal cord) NSAIDs are effective in: arthritis pain of muscular and vascular origin headache, toothache, dysmenorrhoea in combination with opioids : decrease in postoperative pain Antiinflammatory effect NSAIDs reduce mainly components of the inflammatory and immune response in which the products of COX-2 action play a significant part: • vasodilatation • oedema • pain THE SALICYLATES natural products that contain precursors of salicylic acid such as willow bark (glycoside salicin) acetylsalicylic acid sodium salicylate methylsalicylate used in topical applications diflunisal ASPIRIN (acetylsalicylic acid) pharmacokinetics well absorbed, highly bound to plasma proteins first-pass effect--converted to salicylic acid in low dose t1/2 = 4 h, first-order kinetics in high doses >4 g/day saturation pharmacokinetics (danger of overdosage !) pH of urine Unwanted effects: • gastritis with focal erosions and bleeding • salicylism with repeated ingestion of large doses of s: tinnitus, vertigo, decreased hearing • Reye´s syndrom in children: encephalopathy and hepatopathy that can follow an acute viral illness (treated with aspirin). RS has a 20-40% mortality • allergic reactions: skin rashes, worsening of asthma IND: • antiplatelet effects: • analgesic effects: 0.1 g/day 0.5 g 4-6times/day for short-term analgesia • antiinflammatory effects: 3.5 - 4 g/day for long-term treatment IBUPROFEN analgesic, antipyretic and antiinflammatory action without gastric toxicity ind: acute pain for short-term analgesia OTHER NSAIDs • for antiinflammatory effects in acute or chronic inflammatory conditions (e.g. rheumatoid arthritis and related connective tissue disorders) • are given in higher doses then that for simple analgesia and treatment may need to be continued for long period indomethacin, naproxen can also be used for severe pain unrelated to inflammation flurbiprofen, diclofenac more selective for COX-2: nimuselide, celecoxib (treatment of arthritis) COX Isoform Selectivity of Commercially Available NSAIDs and Investigational COX-2 Selective Inhibitors Highly COX-1 Selective Relatively COX-1 Selective Flurbiprofen Fenoprofen Ketoprofen Piroxicam Equally Selective Aspirin Ibuprofen Indomethacin Ketorolac Naproxen Oxaprozin Tolmetin Relatively COX-2 Selective Highly COX-2 Selective Diclofenac Etodolac Meloxicam Nabumetone Nimesulide Celecoxib Rofecoxib L-743,337 NS-398 Valdecoxib Parecoxib Vane JR et al. Annu Rev Pharmacol Toxicol. 1998;38:97-120. Unwanted effects • gastrointestinal disturbances dyspepsia, diarrhoea, nausea, vomiting one in five chronic users: gastric damage (risk of serious hemorrhage and/or perforation) PGs inhibit acid secretion and have protecting action on the gastric mucosa • skin reactions (from mild rashes, urticaria to more serious reactions) • renal reactions acute renal insufficiency reversible on stopping the drug (due to inhibition of PGE2 mediated compensatory vasodilatation that occurs in response to NORA and ANG II) chronic NSAIDs consumption: analgesic nephropathy chronic nephritis, renal papillary necrosis (renal hypertension, malignancies) NSAID-Induced Upper GI Toxicity • Estimated prevalence of dyspepsia is 10%-60% • Use of nonselective COX-2 NSAIDs is associated with a significantly increased risk of gastric and duodonal ulcers • Endoscopic ulcer point prevalence is 10%-30% • Upper GI ulcers, gross bleeding, or perforation caused by NSAIDs appears to occur in 2%-4% of patients treated for 1 year • Majority of patients hospitalized for NSAID-induced ulcer complications have no warning symptoms Singh G. Am J Med. 1998;105(suppl 1B):31S-38S. (cont) NSAID-Induced Upper GI Toxicity • NSAID use is associated with significant morbidity and mortality – Approximately 107,000 hospitalizations per year – More than 16,500 deaths per year – Relative risk does not decline with long-term therapy Singh G. Am J Med. 1998;105(suppl 1B):31S-38S. Prevention of NSAID-Induced Gastropathy • • • • • Is inflammation present? Misoprostil Omeprazole Not H2-Blockers COX-2 selective NSAIDs Criteria for NSAID Selection • Record of efficacy and safety (experience, length of time on the market) • Patient characteristics and concomitant disease states (minimize risks in high risk patients) • Pharmacodynamic/pharmacokinetic profiles • Dose - Dosing interval • Price Pros and Cons of NSAID Therapy Pros • Effective control of inflammation and pain • Effective reduction in swelling • Improves mobility, flexibility, range of motion • Improve quality of life • Relatively low-cost Cons • Does not affect disease progression • GI toxicity common • Renal complications (eg, irreversible renal insufficiency, papillary necrosis) • Hepatic dysfunction • CNS toxicity Rheumatoid Arthritis: Disease-Modifying Antirheumatic Drugs • DMARDs can alter the progression of RA • May be initiated within the first 3 months of diagnosis if: – – – – Ongoing inflammation despite treatment with NSAIDS Glucocorticoid dose 7.5 mg prednisone/day (or equiv) Radiographic evidence of joint destruction Presence or development of extra-articular disease • May take 2wks - 6 months for a response Rheumatoid disease (one of commonest chronic inflammatory conditions) is a common cause of disability. The primary inflammatory cytokines, interleukin-1 and tumour necrosis factor-α , have a major role in pathogenesis DMARDs improve symptoms and can reduce disease activity as measured by: • reduction in number of swollen and tender joints • pain score • disability score • radiology • serum concentration of acute-phase proteins The effects : • probably result from inhibition of excessive cytokine liberation • are slow in onset • only have a part to play in progressive disease • are also toxic (the patient must be monitored) IND: rheumatoid + psoriatic arthritis Drugs Unwanted effects Comments --------------------------------------------------------------------------Immunosuppressants blood dyscrasias MTX is usual methotrexate (MTX) carcinogenesis first-choice azathioprin opportunistic inf. DMARD cyclosporin MTX: cirrhosis mucositis cycl.: nephrotoxicity hypertension --------------------------------------------------------------------------------------sulphasalazine blood dyscrasias s. is also used for (combination of rashes chronic inflammatory sulphonamide colours urine/tears bowel disease with a salicylate) orange Drugs Gold compounds Unwanted effects skin rashses Comments inhibit mitogensodium aurotiomalate mouth ulcerations induced concentrated in macrophages lymphocyte and synovial cells in joints, proliferation effects appear slowly (in months) (maximum effects in 3-4months) penicillamine in 40% nauzea, vomiting, proteinuria is known to have metal-chelating propert and decreases IL-1 gener. chloroquine blurring of vision decreases leukocyte retinopathies chemotaxis, lyozomal enzyme release Rheumatoid Arthritis: Choice of DMARDs Drug hydroxychloroquine sulfasalazine Side Effects retinal toxicity, diarrhea bone marrow suppression, GI intolerance • Can be used as initial therapy in milder disease • Semiannual eye exam for HCQ (macular damage) • Dosing: – SAS - 1 gram bid or tid – HCQ - 200 mg bid (maintenance) Rheumatoid Arthritis: Choice of DMARDs Drug methotrexate Side Effects bone marrow suppression, hepatic and pulmonary toxicity, GI intolerance, stomatitis, rash • Most rapid onset and sustained benefit • Weekly dose 7.5-15 mg PO • Close monitoring required Rheumatoid Arthritis: Choice of DMARDs Drug gold salts Side Effects bone marrow suppression, rash, stomatitis, proteinuria diarrhea, edema • Administered IM (50 mg) on a weekly basis for 35 months, followed by less frequent dosing • Requires close monitoring of bone marrow and renal toxicity • PO dosing 3-6 mg qd (auranofin) Rheumatoid Arthritis: Choice of DMARDs Drug azathioprine Side Effects bone marrow suppression, hepatotoxicity, GI symptoms • AZA is used when disease activity persists on other DMARDs • May be safer than MTX for patients > 65 years with renal insufficiency • PO dose: 50-100 mg qd (max 2.5 mg/kg/day) Rheumatoid Arthritis: Choice of DMARDs Drug D-penicillamine Side Effects bone marrow suppression, rash, stomatitis, dysgeusia, proteinuria, autoimmune disease • d-Penicillamine is used if disease activity persists on other DMARDs • Associated with high incidence of lupus, myasthenia gravis • PO dose: 125-250 mg qd (max. 1 gram/day) Rheumatoid Arthritis: Choice of DMARDs Drug cyclophosphamide Side Effects bone marrow suppression hemorrhagic cystitis, malignancy, infertility • Oral immunosuppressive agent with significant toxicity profile • Used in severe vasculitis and other extra-articular involvement • PO dose: 50-100 mg qd (max 2.5 mg/kg/day) DMARD Combinations • • • • • • MTX + sulfasalazine MTX + hydroxychloroquine (HCQ) MTX + sulfasalazine + HCQ MTX + gold MTX + Azathioprine + HCQ MTX + Penicillamine Rheumatoid Arthritis: Choice of DMARDs • • • • • • Cost Dosing regimen Compliance Comorbid disease states Toxicity profile and monitoring requirements Severity and prognosis of patient Rheumatoid Arthritis : Glucocorticoids • Potent rapidly acting anti-inflammatory agents • Used as “bridge therapy” until DMARD’s become effective; local injection is efficacious and less toxic than DMARD’s • Low dose systemic therapy may slow the rate of joint damage and is effective in refractory RA Rheumatoid Arthritis: Glucocorticoids • Side effects: – Osteoporosis, Cushingoid state, hypertension, premature athersclerosis, infection • Reducing the risk of osteoporosis: – Regular exercise, estrogen therapy, supplemental calcium and vitamin D – Calcitonin or bisphosphonates in patients with low bone mass Pros and Cons of Corticosteroid Therapy Pros • Anti-inflammatory and immunosuppressive effects • Can be used to bridge gap between initiation of DMARD therapy and onset of action • Intra-articluar injections can Cons • Does not conclusively affect disease progression • Tapering and discontinuation of use often unsuccessful • Low doses result in skin thinning, ecchymoses, and Cushingoid appearance • Significant cause of steroidinduced osteopenia New Pharmacologic Agents • Immunomodulator: – Leflunomide • Biologic Response Modifiers – Etanercept – Infliximab • Antibiotics: – Minocycline Leflunomide/A77 1726 Primary Mechanism of Action DHODH Dihydroorotate Orotate Salvage pathway UMP Extracellular pyrimidines Leflunomide Glutamine + HCO3 + Aspartate DNA/RNA synthesis; glycosylation Pyrimidine nucleotides Leflunomide: • Hepatic metabolism: – Active metabolite inhibits cell proliferation in activated lymphocytes; results in cell cycle arrest – t 1/2 ~14 days – Dose: 100 mg/day x3 days then 20 mg qd • Side effects: – Diarrhea 27%, LFT’s 10%, rash 8%, alopecia 7% Etanercept: • soluble receptor for TNFα • Indication: – To reduce signs/symptoms of moderate to severe active RA in patients who have had an inadequate response to one or more DMARD’s • Dose: – 10 mg or 25 mg SC twice a week • Kinetics: – t 1/2 of 25 mg dose ~5 days • Response rate: – 50-70% in moderate or severe RA Infliximab: • Monoclonal TNF- antibody (binds TNF) • Chimeric mouse-human IgG1 • Well-tolerated and effective in ~50% of patients with RA • FDA approved for use w/mtx to reduce s/s of RA (inadeq response) Infliximab • Administered as IV infusion: 3 mg/kg single dose followed with doses 2-6 weeks after the first dose, then q8weeks • Should be used with methotrexate for synergy and enhanced duration of response • Adverse events include increased risk of infection, hypersensitivity reactions, and formation of auto-antibodies Antibiotics: Minocycline • Tetracyclines first advocated for RA in 1960’s • Minocycline: – inhibits metalloproteinases which destroy cartilage – 3 Clinical Trials have shown statistically significant improvement in patients w/RA New Agents - Place in Therapy • TNF blockade will likely become a major therapeutic advance in treatment of RA • Leflunomide can be added to MTX if disease remains active and LFT’s are stable • Etanercept, and infliximab should be considered if disease remains active despite adequate DMARD trials (3-6 months at therapeutic doses) or significant toxicity precludes continued administration of other DMARD’s Chondroprotective agents • Glukosamine sulphate • Chondroitine sulphate • Hyaluronic acid • Diacereine Rheumatoid Arthritis: Prognosis • Progressive in 2/3 of patients resulting in disabling and destructive disease • Poor Prognostic Factors: – Male, age >50, poor functional capacity, positive RF, presence of nodules, HLA-DR4 • 3-10 year decrease in survival in 50% of patients Drugs used in gout • artritis (deposit of monosodium urate in joints and cartilage) • excess of meal, drinking (alcohol), gait, stress, mild injury • Acute attack • Colchicine, Indometacine Chronic gout • Uricosuric agents (probenecid, sulfinpyrazon) • - reabsorption of uric acid in the proximal tubule is decreased • Inhibition of synthesis (allopurinol) • inhibititor of xanthine oxidase