GI Case Study
advertisement

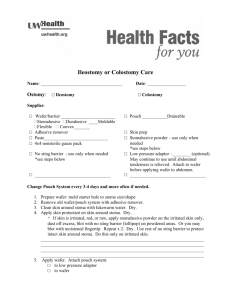
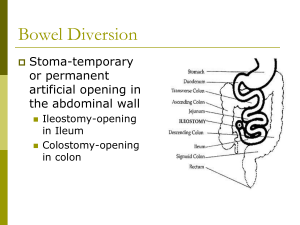
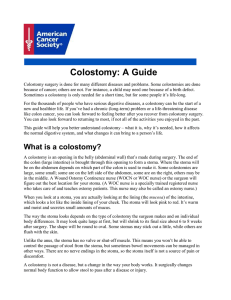
GI Case Study N.L. is a 27 year old female with admitted with recurrent bloody stools and dehydration. She has been having cramping and sharp pain in her LLQ for the past day and almost continuous diarrheal stools. Her vital signs are: 104/60, 96, 20, 38.2 C. Her lab work reveals Hgb: 9.2 g/dl, Na 130 mmol/L., K 3.5 mmol/L, Mg 1.0 mEq/L She is very weak, pale and she states that she just wants the pain and diarrhea to stop. She has had diarrheal stools in the past, but not to this extent. She was diagnosed with ulcerative colitis when she was 20 years old, but has been controlling it with medication and diet. What medications and diet would you anticipate N.L. was receiving? MEDS: Common drug therapy for UC includes aminosalicylates, glucocorticoids, immunomodulators, and antidiarrheal drugs. The aminosalicylates are a class of drug used to treat mild to moderate UC and/or maintain remission after accomplished by other treatments. Four aminosalicylate compounds are available. All deliver 5-aminosalicylic acid (5-ASA) to the affected area. The method of action is unknown but thought to have an anti-inflammatory effect by inhibiting prostaglandins. These agents are effective in 2 to 4 weeks. Sulfasalazine (Azulfidine, Azulfidine EN-tabs) is metabolized by the intestinal bacteria into 5ASA, which delivers the beneficial effects of the drug, and sulfapyridine, which is responsible for the side effects (nausea, vomiting, anorexia, folate malabsorption, and headache). With higher doses, rash, hemolytic anemia, hepatitis, male infertility, or agranulocytosis can occur. This drug is in the same family as sulfonamide antibiotics. Therefore assess the patient for an allergy to sulfonamide or other drugs that contain sulfur such as furosemide. The use of a thiazide diuretic is a contraindication for sulfasalazine. Mesalamine (Asacol, Pentasa, Rowasa) is the generic name for 5-ASA. This drug is better tolerated than sulfasalazine, with side effects of headache and GI upset. Asacol is an entericcoated drug and is released in the terminal ileum and right side of the colon. Pentasa is a delayed-release drug and is released throughout the small bowel and colon to the rectum. Rowasa is a suppository or enema used nightly to treat left-sided disease. Topical agents (suppository or enema) have minimal systemic absorption and therefore have fewer side effects. Balsalazide (Colazal) releases 5-ASA and is well tolerated, with headache and abdominal pain as the primary side effects. It is distributed mainly in the colon itself, with little drug effectiveness in the terminal ileum. Table 60-5 lists recommended doses for the 5-ASA drugs. Glucocorticoids, such as prednisone and budesonide, are corticosteroid therapies prescribed during exacerbations of the disease. Prednisone (Deltasone, Winpred) 40 to 65 mg daily is usually given orally. Once clinical improvement occurs, the corticosteroids are tapered because of the adverse effects that commonly occur with long-term steroid therapy (e.g., hyperglycemia, osteoporosis, peptic ulcer disease, increased risk for infection). For patients with rectal symptoms, topical steroids in the form of small retention enemas may be prescribed. Hydrocortisone rectal foam (Cortifoam) is prescribed as one to two times daily for 2 to 3 weeks and then every other day. Hydrocortisone enemas (Cortenema) are given at bedtime for 21 days, tapered, and discontinued. Immunomodulators are drugs that alter a person's immune response. They are not thought to be effective in the treatment of ulcerative colitis. However, in combination with steroids, they may offer a synergistic effect to a quicker response, thereby decreasing the amount of steroids needed. For example, cyclosporine used in severely ill patients might avoid an emergent colectomy. Immunosuppressants used with UC (and Crohn's disease) include azathioprine, mercaptopurine, cyclosporine, methotrexate, infliximab, and adalimumab. To provide symptomatic management of diarrhea, antidiarrheal drugs may be prescribed. These drugs are given very cautiously, however, because they can cause colon dilation and toxic megacolon. Common antidiarrheal drugs include diphenoxylate hydrochloride and atropine sulfate (Lomotil) and loperamide (Imodium). Although not approved as a first-line therapy for ulcerative colitis, infliximab (Remicade) may be used for refractory disease or for severe complications, such as toxic megacolon (massive dilation of the colon that can lead to peritonitis). Remicade is an immunoglobulin G (IgG) monoclonal antibody that reduces the activity of tumor necrosis factor (TNF) to decrease inflammation. Adalimumab (Humira) is another monoclonal antibody recently approved for refractory cases. They are used more commonly in management of Crohn's disease. These drugs cause immune suppression and should be used with caution. Teach the patient to report any signs of a beginning infection, including a cold, and to avoid large crowds or others who are sick. DIET: Patients with severe symptoms are kept NPO to ensure bowel rest. The physician may prescribe total parenteral nutrition (TPN) for severely ill and malnourished patients. Chapter 63 describes this therapy in detail. Patients with less severe symptoms may drink elemental formulas such as Vivonex, which are absorbed in the small bowel and reduce bowel stimulation. Those with significant but less severe symptoms may be restricted to a low-fiber (low-residue) diet. Although a fiber-restricted diet remains controversial, teach the patient to limit or omit foods that cause him or her discomfort or diarrhea. Often, lactose-containing foods are poorly tolerated and should be reduced or eliminated. Warn the patient that caffeinated beverages, pepper, alcohol, and smoking are common GI stimulants that could cause discomfort. Smoking and other forms of nicotine have been shown to help heal ulcerative colitis, but this approach is not recommended. What are signs of Ulcerative Colitis? What are potential complications of this condition? Ulcerative colitis (UC) creates widespread inflammation of mainly the rectum and rectosigmoid colon but can extend to the entire colon with “backwash ileitis” evident in the terminal ileum when the disease is extensive. Distribution of the disease can remain constant for years. UC is a disease that is associated with periodic remissions and exacerbations (flare-ups). In mild disease, the intestinal mucosa is hyperemic (has increased blood flow), edematous, and reddened. In more severe inflammation, the lining can bleed and small erosions, or ulcers, occur. Abscesses can form in these ulcerative areas and result in tissue necrosis (cell death). Continued edema and mucosal thickening can lead to a narrowed colon and possibly a partial bowel obstruction. Table 60-3 lists the categories of the severity of UC. The patient's stool typically contains blood and mucus. Patients report tenesmus (an unpleasant and urgent sensation to defecate) and lower abdominal colicky pain relieved with defecation. Malaise, anorexia, and weight loss are common. Anemia occurs less often. Extraintestinal manifestations such as migratory polyarthritis, ankylosing spondylitis, and erythema nodosum are present in some patients. Gallstones are also common. With long-term disease, cellular changes can occur that increase the risk for colon cancer. Damage from inflammatory cytokines (e.g., interleukins [IL-1, IL-6, IL-8) and tumor necrosis factor (TNF)–alpha have cytotoxic effects on the colonic mucosa. Therefore annual colonoscopies are recommended when the patient has longer than a 10-year history of UC involving the entire colon. Primary sclerosing cholangitis (PSC) is a chronic fibrosing inflammation of the intrahepatic/ extrahepatic bile ducts that can develop into cirrhosis and commonly occurs with UC. What treatments do you expect to start for this patient? She is scheduled for a colonoscopy this pm, what type of preparation would she receive? Do you expect her to receive a complete bowel prep? Why? Her colonoscopy reveals severe U.C. in her descending colon. The physician wants to schedule her for surgery, but says that she has to first have her labs corrected. What do think this means and what lab work above needs to be corrected? Laboratory Assessment: As a result of chronic blood loss, hematocrit and hemoglobin levels may be low, which indicates anemia and a chronic disease state. An increased WBC count, platelet count, C-reactive protein, or erythrocyte sedimentation rate (ESR) is consistent with inflammatory disease. Blood levels of sodium, potassium, and chloride may be low as a result of frequent diarrheal stools and malabsorption through the diseased bowel. Hypoalbuminemia (decreased serum albumin) is found in patients with extensive disease from losing protein in the stool. Other Diagnostic Assessment: A colonoscopy is the most definitive test for diagnosing UC. In some cases, a computed tomography (CT) scan may be done to confirm the disease or its complications. Barium enemas with air contrast can show differences between UC and Crohn's disease and identify complications, mucosal patterns, and the distribution and depth of disease involvement. In early disease, the barium enema may show incomplete filling as a result of inflammation and fine ulcerations along the bowel contour, which appear deeper in more advanced disease. N.L. is ordered 2 Units of PRBC’s prior to surgery. What precautions need to be taken when administering blood, including how to hang blood, ie. What types of fluid to give with it and the type of IV line. Explain how the blood is checked and what is monitored. Blood products should be given only with NS 0.9% because D5W will also cause hemolysis of the blood product. Given w/out a pump, just hung… 18 gauge, anything smaller will take forever to infuse & there is a time limit. For infusion of blood, it is essential to always check the expiration date of blood and/or blood components to make sure that the blood is not outdated. Under NO circumstances should outdated blood be used! Policies at most hospitals and other health care agencies require that blood and blood products be double checked by another registered nurse BEFORE the blood is hung and infused. This is important in preventing a mix up of blood types. Blood types should always be a major concern because of the possible complications that can occur, some life threatening, if the wrong blood type is given or if the blood is given to the wrong person. The five “Rights” of drug administration remain critical in all that nurses do with medications, and administering blood is no exception. When infusing blood and blood products, all vital signs and related parameters should be documented before, during, and after administration of a blood product, component (e.g., PPF, platelets, and FFP), or solution. The patient should then be assessed and the findings documented. Vital signs should also be checked and recorded. A transfusion reaction would most likely be noted by the occurrence of the following: apprehension, restlessness, flushed skin, increased pulse and respirations, dyspnea, rash, joint or lower back pain, swelling, fever and chills (a febrile reaction beginning 1 hour after the start of administration and possibly lasting up to 10 hours), nausea, weakness, and jaundice. These signs and symptoms should be reported to the physician immediately, and regardless of when the reaction occurs, the blood or product should be stopped and IV line kept patent with isotonic NS solution infusing at a low drip. Always follow the facility's protocol for transfusion reactions. In summary, patients taking any type of fluid or electrolyte substance, colloid, or blood component should be encouraged to immediately report unusual adverse effects to their physician. Such complaints include chest pain, dizziness, weakness, and shortness of breath. EVALUATION: The therapeutic response to fluid, electrolyte, and blood or blood component therapy includes normalization of fluid volume and laboratory values, including RBCs, WBCs, Hgb, Hct, sodium, and potassium. In addition to these laboratory values, evaluation of the patient's cardiac, respiratory, musculoskeletal, and gastrointestinal functioning is also important. Energy levels and tolerance to activities of daily living should return to normal. There should be improved skin color, minimal to no dyspnea, chest pain, weakness, or fatigue. Blood volume that has been correctly treated will be evidenced by a return to normal of the laboratory values, improved vital signs, an increase in energy, and near normal O2 saturation levels. The therapeutic response to albumin therapy includes an elevation of blood pressure, decreased edema, and increased serum albumin levels. Monitoring for the adverse effects of any of these drugs and/or solutions should occur frequently and include monitoring for distended neck veins; shortness of breath; anxiety; insomnia; expiratory crackles; frothy, blood-tinged sputum; and cyanosis. After N.L. receives her blood, her Hgb climbs to 11.5 and surgery is scheduled for the next am. Her stools have slowed somewhat with the IV fluids and her pain level has decreased. The physician tells N.L. that he has planned surgery tomorrow for a left total colectomy and descending colostomy. N.L. agrees, but when you enter the room later she is crying. She asks you ,“what am I going to do with a colostomy: I’m only 27 years old and I’ve never had children.” What would you say to her? Whom may you call as a resource? Identify the local ostomy support group by contacting the United Ostomy Associations of America (www.uoaa.org). The United Ostomy Association of Canada serves the needs of Canadian patients (www.ostomycanada.ca). A local support group or the Crohn's and Colitis Foundation of America (www.ccfa.org) may be helpful in obtaining supplies and providing education for ostomates. Inform the patient and family of available ostomy ambulatory care clinics and ostomy specialists. If the patient agrees, a visit from an ostomate can be continued after discharge to home. When an ileostomy is indicated, provide an in-depth explanation to the patient and family. An ileostomy is a procedure in which a loop of the ileum is placed through the abdominal wall (stoma) for drainage of fecal material into a pouching system worn on the abdomen. The pouching system consists of a solid skin barrier (wafer) to protect the skin and a fecal collection device (pouch). The surgeon usually consults with a certified wound, ostomy, continence nurse (CWOCN) or enterostomal therapist (ET) (sometimes called an ostomy nurse) before surgery for recommendations on the best location of the stoma. A visit from an ostomate (a patient with an ostomy) may be helpful before surgery. Oral or parenteral antibiotics such as neomycin sulfate (Mycifradin) are prescribed as a bowel antiseptic. Cleansing of the bowel with enemas or laxatives may also be needed although the value of preoperative bowel preparation is currently being questioned (Jung et al., 2007). The next day N.L. returns from surgery, she has a PCA with dilaudid running and states that she has pain of 6/10. You explain to her how the PCA works and have her demonstrate. Besides her PCA, what types of alternative therapies may help relieve her pain? she may benefit from nutrition changes to decrease abdominal discomfort such as cramping and bloating. Antidiarrheal drugs such as Imodium or Lomotil are used to control diarrhea, thus reducing the discomfort. However, they must be used with caution and for a short time because toxic megacolon can develop. Perineal skin can be irritated by contact with loose stools and frequent cleaning. Explain special measures for skin care. Use of medicated wipes is soothing if the rectal area is tender You assess her surgical and note the colostomy site. How should a normal stoma appear? What type of stool do you anticipate N.L. will have from her colostomy? The stoma (Fig. 60-2, B) is usually placed in the right lower quadrant of the abdomen below the belt line. It should not be prolapsed or retract into the abdominal wall. The stoma should be pinkish to cherry red because it should be receiving an adequate blood supply. If it looks pale, bluish, or dark, report these findings to the health care provider immediately. With a permanent ileostomy, initially after surgery the output is a loose, dark green liquid that may contain some blood. Over time, a process called “ileostomy adaptation” occurs. The small intestine begins to perform some of the functions that had previously been done by the colon, including the absorption of increased amounts of sodium and water. Stool volume decreases, becomes thicker (pastelike), and turns yellow-green or yellow-brown. The effluent (fluid material) usually has little odor or a sweet odor. Any foul or unpleasant odor may be a symptom of a problem such as blockage or infection. The ostomy drains frequently, and the stool is irritating. The patient must wear a pouch system at all times. The stool from the small intestine contains many enzymes and bile salts, which can quickly irritate and injure the skin. Skin care around the stoma is a priority! A pouch system with a skin barrier (gelatin or pectin) provides sufficient protection for most patients. Other products are also available. Three days later, N.L. is off of the pain medication and up in her room, she will be going home tomorrow and you know that she has not taken care of her colostomy yet. She turns her head whenever someone empties it. How are you going to get her involved in this care? Describe in detail how a patient should change and empty an ostomy appliance. Get someone w/ an ostomy to talk to NL. Call an ostomy support group. Ileostomy Care SKIN PROTECTION: • Use a pectin-based skin barrier to protect your skin from contact with contents from the ostomy. Use skin care products, such as skin sealants and ostomy skin creams. If your skin continues to come into contact with ostomy contents, select a product to fill in problem areas and provide an even skin surface. • Watch your skin for any irritation or redness. POUCH CARE: • Empty your pouch when it is one-third to one-half full. • Change the pouch during inactive times, such as before meals, before retiring at night, on waking in the morning, and 2 to 4 hours after eating. • Change the entire pouch system every 3 to 7 days. NUTRITION: Chew food thoroughly. • Be cautious of high-fiber and high-cellulose foods. You may need to eliminate these from the diet if they cause severe problems (diarrhea, constipation, or blockage). Examples include corn, peanuts, coconut, Chinese vegetables, string beans, tough-fiber meats, shrimp and lobster, rice, bran, and vegetables with skins (tomatoes, corn, and peas). A case manager (D. S.) from the hospital stops in to see N.L. and she reveals that she also has a colostomy. D.S. discusses her diet and sexual activity with N.L. What information do you think may they have discussed? Can N.L. engage in all activities? Do you think that she can have children? A patient with an ileostomy may have many concerns about management at home and about sexual and social adjustments. Considering possible sexual issues helps the patient identify and discuss these concerns with the sex partner. For example, a simple change in positioning during intercourse may alleviate apprehension. Social situations may cause anxiety related to decreased self-esteem and a disturbance in body image. Encourage the patient to discuss possible concerns in addressing and resolving these potentially stressful events.