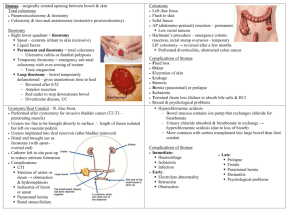
Bowel Diversion Stoma-temporary or permanent artificial opening in the abdominal wall Ileostomy-opening in Ileum Colostomy-opening in colon Bowel Diversion Types of Colostomy Reconstruction Loop colostomy usually temporary large stomas Common site-Transverse colon Loop of bowel is pulled out and an external device (plastic rod, rubber catheter or bridge) is placed to keep the bowel from slipping back loop has 2 openings through 1 stoma Distal- rains mucus Proximal drains stools External device is removed within 7-10 days Types of Colostomy Reconstruction End colostomy The functioning end of the intestine (the section of bowel that remains connected to the upper gastrointestinal tract) is brought out onto the surface of the abdomen, forming the stoma by cuffing the intestine back on itself and suturing the end to the skin The surface of the stoma is actually the lining of the intestine, usually appearing moist and pink. The distal portion of bowel (now connected only to the rectum) may be removed, or sutured closed and left in the abdomen. An end colostomy is usually a permanent ostomy, resulting from trauma, cancer or another pathological condition. Types of Colostomy Reconstruction Double Barrel Colostomy colostomy involves the creation of two separate stomas on the abdominal wall. proximal (nearest) stoma is the functional end that is connected to the upper gastrointestinal tract and will drain stool. distal stoma, connected to the rectum and also called a mucous fistula, drains small amounts of mucus material. most often a temporary colostomy performed to rest an area of bowel, and to be later closed. Total proctocolectomy with permanent ileostomy Total proctocolectomy with permanent ileostomy Removal of colon, rectum and anus with closure of anus. End of terminal ileum is brought out through the abdominal to form an ostomy Ileostomy Ileostomy Possible complications include: skin irritation caused by leakage of digestive fluids onto the skin around the stoma; Irritation is the most common complication of ileostomies diarrhea the development of abscesses gallstones or stones in the urinary tract inflammation of the ileum odors can often be prevented by a change in diet intestinal obstruction a section of the bowel pushing out of the body (prolapse) Total proctocolectomy with continent ileostomy Total proctocolectomy with continent ileostomy The Kock pouch is a variation of the basic ileostomy and is named for its Swedish inventor. In the Kock technique, the surgeon forms a pouch inside the abdominal cavity behind the stoma that collects the fecal material. The stoma is shaped into a valve to prevent fluid from leaking onto the patient's abdomen. The patient then empties the pouch several times daily by inserting a tube (catheter) through the valve. The Kock technique is sometimes called a continent ileostomy because the fluid is contained inside the abdomen. When the patient returns to his room, attach the drainage catheter emerging from the ileostomy to continuous gravity drainage Kock Pouch A thin tube is inserted into the stoma to drain the contents a few times a day. A one-way nipple valve sitting flush with the skin, stops the stool from coming out at all other times. Complications from Kock Pouch Pouchitis Increased stool frequency Urgency hematochezia abdominal cramping Fever Malaise and pelvic pain *treat with Flagyl (metronidazole) Fistula development Nipple valve extrusion Ileostomy Patient education Ileostomy patients must learn to watch their fluid and salt intake. greater risk of becoming dehydrated in hot weather, from exercise, or from diarrhea. In some cases they may need extra bananas or orange juice in the diet to keep up the level of potassium in the blood. Ileostomy Patient education includes social concerns as well as physical self-care. Many ileostomy patients are worried about the effects of the operation on their close relationships and employment. find out about self-help and support groups. The ET can also evaluate the patient's emotional reactions to the ostomy. Ileoanal Reservoir (IAR) The IAR requires complete removal of the colon, leaving all of the small intestine and about two inches of the rectum The lining of the rectum, called the mucosa, is then removed (stripped), leaving the muscle of the rectum and the underlying anal sphincter muscles intact. An ileal J pouch is then formed, using the last 12 inches of the small bowel (ileum). A surgical stapling instrument is used to create the pouch. The end of the pouch is then "pulled through" the pelvis and sewn to the anus. Ileoanal Reservoir (IAR) A temporary ileostomy about 12 inches upstream from the pouch is made. This is constructed to divert stool until the suture lines in the reservoir have healed and the patient has recovered from the operation. This results in all stool going into the ileostomy bag on your right lower abdomen so that the ileal pouch can heal. When the pouch to anus connection has healed, usually about two months, the ileostomy is closed, resulting in bowel movements from your anus. Ileoanal Reservoir Comparison of colostomies & Ileostomy Ascending Transverse Sigmoid Ileostomy Stool consistency Semi liquid Semiliquidsemiformed Formed Liquid to semiliquid Fluid requirement Increased Probably increased No change increased Bowel regulation No Uncommon Yes if with regular pattern No Pouch & yes skin barriers yes Dependent on regulation yes irrigation no no Possible q 24-48 hrs no Indications for surgery Diverticulitis, Same as trauma, CA ascending of colon, rectum or pelvis Ca of rectum or rectosigmoid area, diverticulitis Crohn’s, ulcerative colitis, trauma, CA Effects of food on stoma output ODOR Producing Diarrhea causing Eggs, garlic, onions, fish, asparagus, cabbage, broccoli, alcohol Alcohol, beer, cabbage family, spinach, green beans, coffee, spicy foods, raw fruits Gas Forming Beans, onions, cabbage beer, carbonated beverages, sprouts, Strong cheese Potential for obstruction in Ileostomy Nuts, raisins, popcorn, seeds, raw vegetables, celery, corn NURSING MANAGEMENT Pre-operative preparation Psychological preparation Ability to perform self care Identify support systems Visit by ET Bowel preparation-decrease post op infection Osmotic lavages, cathartics, enemas Antibiotics-neomycin & erythromycin NURSING MANAGEMENT Post-operative Patient adaptation-ADL’s in 6-8 weeks, no heavy lifting, psychological support, identify coping mechanism Colostomy care Assess stoma and surrounding skin Pink stoma-healthy; pale- anemic; dusky bluenecrotic Mild to moderate swelling- till 2-3 weeks is normal; moderate to severe swelling-obstruction of stoma Small amount of oozing-normal; moderate to large bleeding-coagulation problem or or GI bleed NURSING MANAGEMENT Colostomy care Assess stoma and surrounding skin Wash stoma with mild soap & water Use of skin barrier Use of pouch-leave ¼ of skin around the stoma Colostomy irrigations Regulate bowel function-stimulate the bowel to function at specific time everyday or every other day Treat constipation Prepare for surgery Colostomy Irrigation Use lukewarm water as irrigant(500-1000 ml) just enough to distend but not cause cramping Ensure comfortable position-sit up on chair or toilet bowl Hang container on hook or IV pole (18-24 in) above stoma Apply irrigating sleeve and place end in toilet bowl Lubricate stoma cone and insert gently into the stoma Allow irrigation solution to flow steadily for 5-10 minutes: stop the flow if cramping occurs Colostomy Irrigation Clamp the tubing and remove irrigating cone when desired amount has been delivered or when patient senses colonic distention Allow 30-45 minutes for the solution and feces to be expelled. Cleanse, rinse and dry peristomal skin well and replace the colostomy drainage pouch Nursing Diagnosis/Interventions Risk for skin integrity related to irritation from fecal drainage and peristomal area, irritation from appliance and lack of knowledge of skin care Skin assessment, use mild soap & water to cleanse area, use of skin barrier and application of well fitting pouch Nursing Diagnosis/Interventions Disturbed body image related to presence of ostomy and malodor Assess attitude towards ostomy Allow expression of feelings and assist in adjustment process (grief) Prepare patient to do owm stoma and appliance care to increase independnce and enhance self-esteem/image Encourage attendance in support classes or groups Use of measures to control odors Odor proof pouch, pouch deodorants, avoid foods that increases odor Nursing Diagnosis/Interventions Imbalanced nutrition less than body requirements related to decreased appetite and lack of knowledge of appropriate foods Assess nutritional intake Introduce foods one at a time Provide list of foods for reference Risk for fluid volume deficit related to excess fluid loss from ileostomy or diarrhea or inadequate fluid intake Assess for signs & symptoms of fluid & electrolyte imbalance I/O, encourage fluids-3000ml/day Monitor electrolytes Nursing Diagnosis/Interventions Ineffective sexuality patterns related to perceived loss of sexual appeal and accidental seepage of fecal materials during sexual activity Assess patients attitude and impact of the ostomy on the sexual functioning-fear of rejection (encourage open communication) Encourage support groups to share concerns and solutions Encourage use of perfumes or fragrance to combat odors