Basic Human Needs Bowel Elimination
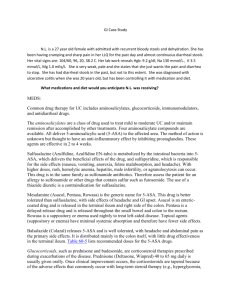
advertisement

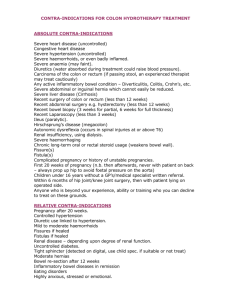
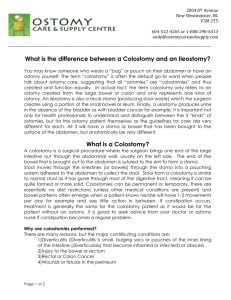
Basic Human Needs Bowel Elimination Bowel Elimination GI Tract is a series of hollow mucous membrane lined muscular organs Purpose is to absorb fluids & nutrients, prepare food for absorption & provide storage for feces GI Tract Anatomy Mouth Esophagus Stomach Small Intestine Large Intestine Rectum Mouth Digestion begins here Mechanical, chemical breakdown of nutrients Teeth-Mastication Salivary secretions-enzymes Food Bolus Esophagus Hollow, muscular tube for passage of food to stomach Peristaltic waves, contraction and relaxation of smooth muscle moves food down to stomach Sphincter control to prevent reflux Stomach Food is temporarily stored and mechanically and chemically broken down Secretes HCL, mucus, pepsin, & intrinsic factor(Needed for Vitamin B12 absorption) Food is converted into chyme Small Intestine 1 inch in diameter 20 feet long Three divisions: Duodenum, Jejunum, Ileum Enzymes in small intestine (amylase, lipase, & bile) break down fats, proteins & carbs into basic elements Nutrients absorbed in duodenum & jejunum, ileum absorbs vitamins, iron, & bile salts Large Intestine Lower GI tract Larger diameter, 5-6 feet in length 3 divisions: cecum, colon, rectum Responsible for absorption of water Primary organ of bowel elimination Cecum-chyme enters cecum via the ileocecal valve, valve prevents regurg back to small intestine, cecum ends with appendix Colon 3 Divisions: Ascending, Transverse, Descending Colon Functions: Absorption, Protection, Secretion, & Elimination (stool and flatus) Flatus Formation Air swallowing Diffusion of gas from bloodstream into intestines Bacterial action on unabsorbable CHO (Beans) Fermentation of CHO (cabbage, onions Can stimulate peristalsis Adult forms 400-700 ml of flatus daily Rectum Sigmoid colon Storage of feces Length varies with age When fecal mass or flatus moves into rectum, it distends and defecation begins Process involves involuntary (Internal sphincter) and voluntary control (external sphincter) Valsalva Maneuver- voluntary contraction of abdominal muscles Factors Affecting Bowel Elimination Age Infection Diet Fluid Intake Physical Activity Psychological factors Personal Habits Factors Affecting Bowel Elimination Position during Defecation Pain Surgery and Anesthesia Medications Common Bowel Elimination Problems Constipation Impaction Diarrhea Incontinence Flatulence Hemorrhoids Constipation More of a symptom than a disorder Decrease in frequency of BM Straining & pain on defecation is associated symptoms(Valsalva maneuver) Can be significant heath hazard (increase ICP, IOP, reopen surgical wounds, cause trauma, cardiac arrhythmias) Impaction Results from unrelieved constipation Collection of hardened feces wedged into rectum Can extend up to sigmoid colon Most at risk: depilated, confused, unconscious (all are at risk for dehydration) Impaction When a continuous ooze of diarrheal stool develops, impaction should be suspected Associated S/S: Loss of appetite, abdominal distention, cramping, rectal pain Diarrhea Increase in number of stools & the passage of liquid, unformed stool Symptom of disorders affecting digestion, absorption, & secretion of GI tract Intestinal contents pass through small & large intestines too quickly to allow for usual absorption of water & nutrients Diarrhea Irritation can result in increased mucus secretion, feces become too watery, unable to control defecation Excess loss of colonic fluid can result in acid-base imbalances or fluid/electrolyte imbalances Can also result in skin breakdown Conditions that cause Diarrhea Emotional Stress Intestinal Infection (Clostridium difficile) Food Allergies Food Intolerance Tube Feedings (Enteral) Medications Laxatives Colon Disease Surgery Incontinence Inability to control passage of feces and gas from the anus Caused by conditions that create frequent, loose, large volume, watery stools or conditions that impair sphincter control or function Flatulence Gas accumulation in the lumen of intestines Bowel wall stretches and distends Common cause of abdominal fullness, pain, & cramping Gas escapes through mouth (belching), or anus (flatus) Hemorrhoids Dilated, engorged veins in the lining of the rectum External (Clearly visible) or Internal Caused by straining, pregnancy, CHF, chronic liver disease Clicker Question 1. A newly admitted client states that he has recently had a change in medications and reports that stools are now dry and hard to pass. This type of bowel pattern is consistent with: A. Abnormal defecation B. Constipation C. Fecal impaction D. Fecal incontinence 46 - 31 Bowel Diversions Certain diseases cause conditions that prevent normal passage of feces through rectum Creates need for temporary or permanent artificial opening (stoma) in the abdominal wall Bowel Diversions Surgical openings (ostomy) are most commonly formed in the ileum (ileostomy) or the colon (colostomy) Incontinent ostomy- need to wear appliance pouch Continent ostomy- have control through use of ostomy cap Incontinent Ostomy Location of ostomy determines consistency of stool Ileostomy bypasses the entire large intestine, stools are frequent & watery Ascending colostomy- liquid stool Sigmoid colostomy-most like normal stool Incontinent Ostomies Loop colostomy- temporary, usually done on transverse colon 2 openings through stoma, proximal loop for stool, distal loop for mucus End colostomy- one stoma formed from the proximal end of the bowel with the distal portion removed or sewn shut (Hartmann’s Pouch) Incontinent Ostomies End colostomy usually done for colorectal cancer Ruptured diverticulum- temporary end colostomy with a Hartmanns Pouch Double barrel colostomy- Bowel is surgically severed, 2 ends are brought out onto abdomen with 2 distinct stomas (proximal & distal) Continent Diversions Ileoanal reservoir- restorative proctocolectomy, no outward stoma, no pouch wearing, clients have internal pouch created from the ileum Ileal pouches constructed in various configurations (S,J,W) End of the pouch is sewn or anastamosed to the anus Continent Diversions Ileoanal Reservoir Several stages to surgery to create pouch May need temporary ostomy to allow time for pouch to heal Kegel exercises to increase pelvic floor muscle tone Continent Diversions Kock Continent Ileostomy-Internal reservoir or pouch is created using piece of small intestine Stoma brought out low on abdomen, end of internal part in pouch is a one way nipple valve to promote continence Valve only allows fecal contents to drain when an external catheter is place in stoma, no pouch required Ostomy Nursing Considerations Patient Education Care of stoma, appliance selection and use Body Image considerations Support groups (UOA) Enterostomal nursing- specialty within profession Nursing Process Assessment Nursing History Physical Assessment Lab Tests Fecal characteristics Diagnostic evaluation- Endoscopy, Colonoscopy Nursing Diagnosis Bowel Incontinence Constipation Diarrhea Impaired Skin Integrity Body Image Disturbance Altered bowel elimination Pain Implementation Promoting Normal Defecation and Acute Care Management Positioning of patient-squatting Positioning on bedpan Use of cathartics, laxatives Anti-diarrheal agents Enemas Digital removal of stool Ostomy care Fecal Incontinence Devices Common Laxatives & Cathartics Metamucil-bulk forming Colace, Surfak-emollient or wetting agent Fleets, MOM. Mag Sulfate-saline agent Dulcolax, Ex-Lax, Castor oil- stimulant cathartic Haley’s MO, mineral oil- Lubricant Enemas Cleansing enema Tap water Normal saline Hypertonic Solutions (Fleet’s enema) Soapsuds Oil Retention Medicated enemas (Kayexalate, Lactulose) Administering a Cleansing enema P&P pg. 12001201 Nasogastric Tubes Decompress GI tract in surgery, infection of GI tract, trauma to GI tract, conditions where peristalsis is absent N/G tube purposes- decompression, feeding, compression, & lavage Pliable tube inserted through nasopharynx into stomach Uncomfortable insertion Nasogastric Tubes Types: Levin – single lumen, different sizes used for feeding or decompression Salem Sump – Most preferable for decompression, dual lumen, one for removal of gastric contents, one as an air vent, hooked to suction to achieve decompression Care of Nasogastric Tubes Confirm placement after insertion HOB at 30 degrees unless ordered otherwise Mark point where tube exits nose (AACN 2005) Tape tube securely to nose Tube Irrigation Nasal skin care Frequent oral hygeine Assess for abdominal distention Suction settings Restorative Care Bowel training Maintenance of proper fluid & food intake Promotion of regular exercise Promotion of Comfort Maintenance of skin integrity Promotion of self concept Clicker Question 2. To maintain normal elimination patterns in the hospitalized client, you should instruct the client to defecate 1 hour after meals because: A. The presence of food stimulates peristalsis. B. Mass colonic peristalsis occurs at this time. C. Irregularity helps to develop a habitual pattern. D. Neglecting the urge to defecate can cause diarrhea. 46 - 70