chronic wounds
advertisement

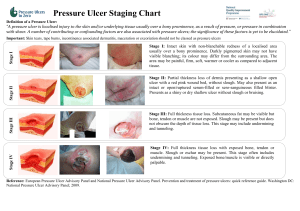
CHRONIC WOUNDS Based on a presentation by Dr. David Thomas at the AMDA Convention Four Kinds of Chronic Wounds Pressure Ulcer (PU) Diabetic Ulcer (DU) Venous Ulcer (VU) Arterial Ulcer (AU) Chronic Ulcer Types Etiology is different Treatment is different Outcome is different Gestalt is different Differential Diagnosis LOCATION CAUSE APPEARS PU Bony Prom DU Callus Pressure Crater Neuropathy/trauma Borders distinct VU Calf/ankle AU Distal points Venous Stasis Inadequate arterial flow Irregular Gangrene Diagnostic Approach Wound over bony prominence (PU,DU) DM with neuropathy, recurrent trauma, surrounding callus (DU) PVD, wet or dry gangrene (AU) Signs of venous stasis/calf or ankle (VU) Other causes possible, but rare Pain in Chronic Ulcers DU: no or diminished pain, sensation VU: little pain, intact sensation PU: intermittent pain AU: constant pain Pressure Ulcers Visible evidence of pathological interruption of blood flow to dermal tissues Chief cause: sustained pressure Most commonly over sacrum, hip Pressure Ulcers: What Works Must relieve pressure or it won’t heal. Must use moist dressing or it won’t heal. Types of Moist Dressings Wet to wet: cheapest Hydrocolloid: for dirty areas Hydrogel/ Foam/ Alginates/ Biomembranes/ Collagen Thin Film Polymers: tear off top layer of cells Problems Most doctors treat few pressure ulcers. Very few good studies; none for most treatments. Treatment modalities for pressure ulcers are considered devices: only safety, NOT efficacy, must be proved. Treatments Proven NOT to Work Zinc paste Antacid Gold leaf Aluminum foil Topical insulin Ultrasound Lasers Arginine Dry dressings Paraffin Treatments with No Data Magnet therapy Honey/ Sugar “Skin equivalents” Treatments With Very Flawed Data Vitamin C Patient’s serum mixed with proprietary gel Vacuum therapy Electrical stimulation Topical Phenytoin Cytokine growth factors Other Effective Treatments Sheng-ji-san (SJS) Whirlpool Any kind of pressure relieving bed Debridement of necrotic tissue: surgical (required if infected), autolytic, enzymatic Pearls from Dr. Thomas Hydrocolloid dressings are impervious to urine and feces but cannot change dressing. Heel ulcers have a very thin layer of tissue underneath: debridement exposes bone. Debride only if tissue is infected; otherwise form crust with betadyne and use boots. Pressure Ulcer Guidelines Address nutrition Promote granulation tissue Promote epithelialization Prevent contamination Dressings Stage I: Thin film polymer Stage II: Moist gauze (wet-to-wet) or hydrocolloid Stage III/ IV with dead space/ exudate: hydrogel, wet-to-wet, or hydrocolloid with synthetic absorption dressing below. Stage III/ IV with necrosis: debride, then treat as III/ IV above. Nursing Home Pearl Home health nursing and nursing home care plans of ulcers tend to call for improved nutrition and healing; if pressure ulcers have occurred because the patient is dying/ not eating, make sure the care plan reflects that (for liability and survey purposes). Venous Stasis Ulcers An area of discontinuity of the epidermis, persisting for 4 weeks or more, occurring as a result of venous hypertension and calf muscle pump insufficiency. Must exclude arterial disease, neuropathy, diabetes, rheumatoid arthritis, hemoglobinopathies, and carcinoma. Biopsy if long-standing or looks weird. Diagnosis of Venous Ulcers Location on the calf Bronzing (lipodermatosclerosis) Exclusion of arterial insufficiency by bounding DP pulses, or ABI > 0.8 Tend to be slow-healing (~90% heal by one year), irregular, and associated with edema and sloughing Treatment of VU: What Works Must compress the calf, or it won’t heal However, arterial insufficiency is an absolute contraindication to compression therapy Must carefully assess for arterial flow Compression Options for VU ACE wrap: useful for removing edema Unna boot: works via muscle contraction against the hard shell; will not work in a nonambulatory patient Venous support hose: comes 25 to 35 mmHg, but 35 needed to work All compression must be wrapped tight enough to be effective Infection in VU All VU’s are colonized No evidence that colonization impairs healing, though may interfere with a graft Don’t culture VU’s! Recognition of Infection in VU’s Fever Increased pain Increased skin erythema Lymphangitis Ulcer rapidly becomes larger If infected, treat with systemic AB’s VU Treatments Hydrocolloid dressing Cadexomer iodine topically Trental (anticytokine) and compression Artificial skin Skin graft TGF-B2 Ineffective VU Treatments (RCT’s) Antibiotics, including Bactroban Elase Zinc Stanozolol Ifetroban Silver sulfadiazine Secondary Prevention in VU’s Recurrence in ~57% Reflux in deep veins in 50 to 71% Prior DVT causes 95% of DV reflux Venous support hose may reduce recurrence rate (unpublished data) Treatment Guidelines--VU Use moist wound dressings Use a compression bandage system Don’t use AB’s/antiseptics unless infected Use grafting/artificial skin only if all other treatments have failed—very expensive, and high recurrence rate Diabetic Ulcers Chronic ulcer in a diabetic patient, not primarily due to other causes Extrinsic causes: smoking, friction, burn Intrinsic causes: neuropathy, macrovascular and microvascular disease, immune dysfunction, deformity, reopened previous ulcer Neuropathy in DU Use monofilament for 5 seconds or less, to avoid triggering propioceptors Also assess temperature sensation— may use reflex hammer Can test pinprick and 2-point discrimination Co-Morbidity in DU Peripheral vascular disease occurs in 11% of diabetic patients Peripheral neuropathy occurs in 42% of diabetic patients PVD is associated with delayed ulcer healing and increased rates of amputation Treatment of DU: What Works Must surgically debride ulcer to allow healing: the wound edges are dead Weekly debridement down to healthy bleeding tissue gives best results Must keep pressure off the ulcers to allow healing Pressure Reduction Off DU Orthopedic shoes: drop recurrence rate from 83% to 17% Sandals Splints Crutches/wheelchairs Total contact casting Total Contact Casting Worsens the ulcer if not applied perfectly Need to find a consultant for this task on whom you can rely Other Possibly Helpful Treatments Moist dressings (clearly better than dry) Hyperbaric O2 Dermagraft (cultured skin—human) Platelet-derived growth factor Antibiotics (ineffective if uncomplicated) Questionable effectiveness: U/S, electrical stimulation Pathogens in DU Infections Mild severity: tend to be Staph and Strep Moderate severity (i.e. non-limb threatening): Staph, Strep, and gram neg Severe/limb-threatening: usually 5 to 6 organisms, including Staph, Strep, E. coli, Enterobacter, Bacteroides, Proteus, Pseudomonas, and MRSA Dx of Osteomyelitis in DU Pearl: A steel probe contacting bone, especially if consistency of bone is crumbly, has PPV 89% and NPV 56% MRI best imaging modality; serial films also of some benefit Bone scan non-specific Bone biopsy gold standard Effective treatment: amputation Arterial Ulcers--AU Tend to occur on distal areas Diminished/absent pulses Punched-out appearance, or gangrene Requires either salvage revascularization, or amputation— usually the latter Diagnosis: ABI ABI= LE systolic BP/Brachial art syst BP ABI < 0.7 abnormal; < 0.4 unlikely to heal Can perform in FMC Values: 0.9-1.30 normal; 0.7-0.89 mild; 0.4-0.69 moderate; < 0.4 severe Medical Treatment of AU Control DM and HTN Moderate exercise Smoking cessation Dry dressings (dry gangrene preferable) ? Pletal, gingko biloba What Works: AU Amputation/revascularization/hospice if ABI < 0.4 Do not compress if ABI < 0.7