Peripheral Vascular Disease: Introduction - Dis Lair
advertisement

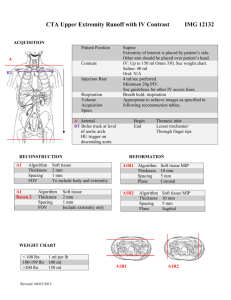
Peripheral Vascular Disease: Introduction Background Peripheral vascular disease (PVD) is a nearly pandemic condition that has the potential to cause loss of limb or even loss of life. Peripheral vascular disease manifests as insufficient tissue perfusion caused by existing atherosclerosis that may be acutely compounded by either emboli or thrombi. Many people live daily with peripheral vascular disease; however, in settings such as acute limb ischemia, this pandemic disease can be life threatening and can require emergency intervention to minimize morbidity and mortality. Pathophysiology PVD, also known as arteriosclerosis obliterans, is primarily the result of atherosclerosis. The atheroma consists of a core of cholesterol joined to proteins with a fibrous intravascular covering. The atherosclerotic process may gradually progress to complete occlusion of medium and large arteries. The disease typically is segmental, with significant variation from patient to patient. Vascular disease may manifest acutely when thrombi, emboli, or acute trauma compromises perfusion. Thromboses are often of an atheromatous nature and occur in the lower extremities more frequently than in the upper extremities. Multiple factors predispose patients for thrombosis. These factors include sepsis, hypotension, low cardiac output, aneurysms, aortic dissection, bypass grafts, and underlying atherosclerotic narrowing of the arterial lumen. Emboli, the most common cause of sudden ischemia, usually are of cardiac origin (80%); they also can originate from proximal atheroma, tumor, or foreign objects. Emboli tend to lodge at artery bifurcations or in areas where vessels abruptly narrow. The femoral artery bifurcation is the most common site (43%), followed by the iliac arteries (18%), the aorta (15%), and the popliteal arteries (15%). The site of occlusion, presence of collateral circulation, and nature of the occlusion (thrombus or embolus) determine the severity of the acute manifestation. Emboli tend to carry higher morbidity because the extremity has not had time to develop collateral circulation. Whether caused by embolus or thrombus, occlusion results in both proximal and distal thrombus formation due to flow stagnation. Clinical History The primary factor for developing peripheral vascular disease (PVD) is atherosclerosis. 1. Other maladies that often coexist with PVD are coronary artery disease (CAD), myocardial infarction (MI), atrial fibrillation, transient ischemic attack, stroke, and renal disease. Studies have suggested that even asymptomatic peripheral arterial disease (PAD) is associated with increased CAD mortality.1 2. 3. 4. 5. 6. 7. Risk factors for PVD include smoking, hyperlipidemia, diabetes mellitus, and hyperviscosity. Other etiologies for developing PVD may include phlebitis, injury or surgery, and autoimmune disease, including vasculitides, arthritis, or coagulopathy. PVD rarely exhibits an acute onset; it instead manifests a more chronic progression of symptoms. Patients with acute emboli causing limb ischemia may have new or chronic atrial fibrillation, valvular disease, or recent MI, whereas a history of claudication, rest pain, or ulceration suggests thrombosis of existing PVD. Radiation-induced PAD is becoming more common, perhaps due to the efficacy of current antineoplastic treatment and increased survival.2 Intermittent claudication may be the sole manifestation of early symptomatic PVD. The level of arterial compromise and the location of the claudication are closely related as follows: Aortoiliac disease manifests as pain in the thigh and buttock, whereas femoral-popliteal disease manifests as pain in the calf. Symptoms are precipitated by walking a predictable distance and are relieved by rest. Collateral circulation may develop, reducing the symptoms of intermittent claudication, but failure to control precipitant factors and risk factors often causes its reemergence. Claudication may also present as the hip or leg "giving out" after a certain period of exertion and may not demonstrate the typical symptom of pain on exertion. The pain of claudication usually does not occur with sitting or standing. Ischemic rest pain is more worrisome; it refers to pain in the extremity due to a combination of PVD and inadequate perfusion. Ischemic rest pain often is exacerbated by poor cardiac output. The condition is often partially or fully relieved by placing the extremity in a dependent position, so that perfusion is enhanced by the effects of gravity. Leriche syndrome is a clinical syndrome described by intermittent claudication, impotence, and significantly decreased or absent femoral pulses. This syndrome indicates chronic peripheral arterial insufficiency due to narrowing of the distal aorta. The patient's medications may provide a clue to the existence of PVD. Pentoxifylline is a commonly used medication specifically prescribed for PVD. Daily aspirin commonly is used for prevention of cardiac disease (CAD), but PVD often coexists, to some degree, in patients with CAD. Physical A systematic examination of the peripheral vasculature is critical for proper evaluation. 1. Peripheral signs of peripheral vascular disease are the classic "5 P's": o Pulselessness o Paralysis o Paraesthesia o Pain o Pallor 2. Paralysis and paraesthesia suggest limb-threatening ischemia and mandate prompt evaluation and consultation. 3. Assess the heart for murmurs or other abnormalities. Investigate all peripheral vessels, including carotid, abdominal, and femoral, for pulse quality and bruit. Note that the dorsalis pedis artery is absent in 5-8% of normal subjects, but the posterior tibial artery usually is present. Both pulses are absent in only about 0.5% of patients. Exercise may cause the obliteration of these pulses. 4. The Allen test may provide information on the radial and ulnar arteries. 5. The skin may have an atrophic, shiny appearance and may demonstrate trophic changes, including alopecia; dry, scaly, or erythematous skin; chronic pigmentation changes; and brittle nails. 6. Advanced PVD may manifest as mottling in a "fishnet pattern" (livedo reticularis), pulselessness, numbness, or cyanosis. Paralysis may follow, and the extremity may become cold; gangrene eventually may be seen. Poorly healing injuries or ulcers in the extremities help provide evidence of preexisting PVD. 7. The ankle-brachial index (ABI) can be measured at bedside. Using Doppler ultrasonography, the pressure at the brachial artery and at the posterior tibialis artery is measured. The ankle systolic pressure is divided by the brachial pressure, both measured in the supine position. Normally, the ratio is more than 1. In severe disease, it is less than 0.5. 8. A semiquantitative assessment of the degree of pallor also may be helpful. While supine, the degree of pallor is assessed. If pallor manifests when the extremity is level, the pallor is classified as level 4. If not, the extremity is raised 60°. If pallor occurs within 30 seconds, it is a level 3; in less than 60 seconds, level 2; in 60 seconds, level 1; and no pallor within 60 seconds, level 0. Differential Diagnoses Aneurysm, Abdominal Lumbar (Intervertebral) Disorders Ankle Injury, Soft Tissue Thrombophlebitis, Septic Back Pain, Mechanical Thrombophlebitis, Superficial Disk Deep Venous Trauma, Thrombosis and Injuries Thrombophlebitis Peripheral Vascular Workup Laboratory Studies 1. Routine blood tests generally are indicated in the evaluation of patients with suspected serious compromise of vascular flow to an extremity. CBC, BUN, creatinine, and electrolytes studies help evaluate factors that might lead to worsening of peripheral perfusion. Risk factors for the development of vascular disease (lipid profile, coagulation tests) can also be evaluated, although not necessarily in the ED setting. 2. An ECG may be obtained to look for evidence of dysrhythmia, chamber enlargement, or MI. 3. Elevated levels of inflammatory blood markers such as D dimer, C-reactive protein, interleukin 6, and homocysteine have been linked to decreased lower extremity tolerance of exercise. Higher levels of activity in daily life have been shown to decrease these levels. The applicability to practice in Emergency Medicine is unknown. Imaging Studies 1. Plain films are of little use in the setting of PVD. Doppler ultrasonographic studies are useful as primary noninvasive studies to determine flow status. Upper extremities are evaluated over the axillary, brachial, ulnar, and radial arteries. Lower extremities are evaluated over the femoral, popliteal, dorsalis pedis, and posterior tibial arteries. Note the presence of Doppler signal and the quality of the signal (ie, monophasic, biphasic, triphasic). The presence of distal flow does not exclude emboli or thrombi because collateral circulation may provide these findings. 2. Magnetic resonance imaging (MRI) may be of some clinical benefit due to its high visual detail. Plaques are imaged easily, as is the difference between vessel wall and flowing blood. MRI also has the benefits of angiography to provide even higher detail and can replace traditional arteriography. The utility of MRI is limited in the emergency setting, often due to location of the device and the technical skill required to interpret the highly detailed images. 3. Computerized tomography (CT) can be of use to the emergency physician since it does not have the time and availability constraints of MRI. Although noncontrast studies can be useful to image calcification and arteriosclerosis, contrast studies are most useful to image arterial insufficiency. Renal function should be confirmed before contrast administration, since PVD often coexists with risk factors for contrast-induced renal failure. Other Tests 1. The ankle-brachial index (ABI) is a useful test to compare pressures in the lower extremity to the upper extremity. Blood pressure normally is slightly higher in the lower extremities than in the upper extremities. Comparison to the contralateral side may suggest the degree of ischemia. 2. The ABI is obtained by applying blood pressure cuffs to the calf and the upper arm. The blood pressure is measured, and the systolic ankle pressure is divided by the systolic brachial pressure. Normal ABI is more than 1; a value less than 0.95 is considered abnormal. This test can be influenced by arteriosclerosis and small vessel disease (eg, diabetes), reducing reliability. Progressive PAD, indicated by ABI decline of greater than 0.15, has been associated with increased cardiovascular disease risk.5 3. Transcutaneous oximetry affords assessment of impaired flow secondary to both microvascular and macrovascular disruption. Its use is increasing, especially in the realm of wound care and patients with diabetes. Transcutaneous oximetry has not been studied extensively in emergent occlusion. Procedures The criterion standard for intraluminal obstruction has always been arteriography, although this is both potentially risky and often unobtainable in the emergency setting. The delay associated with obtaining arteriography in the setting of obvious limb ischemia can delay definitive treatment to deleterious effect. If time allows, arteriography can prove useful in discriminating thrombotic disease from embolic disease. Treatment Prehospital Care Prehospital care for peripheral vascular disease (PVD) involves the basics: control ABCs, obtain intravenous access, and administer oxygen. Generally, do not elevate the extremity. Note and record distal pulses and skin condition. Perform and document a neurological examination of the affected extremities. Emergency Department Care Attention to the ABCs, intravenous access, and obtaining baseline laboratory studies should occur early in the ED visit. Obtain an ECG and chest radiograph. Treatment of either thrombi or emboli in the setting of peripheral vascular disease is similar. Empirically, initiate a heparin infusion with the goal of increasing activated partial thromboplastin time to 1.5 times normal levels. Acute leg pain correlated with a cool distal extremity, diminished or absent distal pulses, and an ankle blood pressure less than 50 mm Hg should prompt consideration of emergent surgical referral. In some cases of emboli, intra-arterial thrombolytic agents may be useful. The exact technique of administration varies, in both dosage and time of administration. Remember that intra-arterial thrombolysis remains investigational. Obviously, such thrombolytic therapy is contraindicated in the presence of active internal bleeding, intracranial bleeding, or bleeding at noncompressible sites. Consultations Early surgical consultation in patients with acute limb ischemia is prudent. Depending on the case, the surgeon may involve interventional radiology or proceed operatively. Emboli may be treated successfully by Fogarty catheter (ie, an intravascular catheter with a balloon at the tip). The balloon is passed distal to the lesion; the balloon is inflated, and the catheter is withdrawn along with the embolus. This technique most commonly is used for iliac, femoral, or popliteal emboli. Definitive treatment of hemodynamically significant aortoiliac disease is usually by aortobifemoral bypass. Its 5year patency rate is approximately 90%. Those patients in whom PVD becomes significant, however, often have a plethora of comorbid medical conditions, such as cardiovascular disease, diabetes, and chronic obstructive pulmonary disease, which increase procedural morbidity and mortality. Axillobifemoral bypass and femoral-femoral bypass are alternatives, both of which have lower 5-year patencies but have lower procedural mortality. Some areas of arteriostenosis can be revascularized with percutaneous transluminal coronary angioplasty (PTCA). If the occlusion is complete, a laser may be useful in making a small hole through which to pass the balloon. Restenosis is a concern with PTCA, particularly for larger lesions. Stents and lasers are still considered experimental. An initial study shows promise in relieving the pain of PAD with topically applied lidocaine spray. Suzuki and colleagues studied 24 subjects with PAD and noted a significant drop in pain associated with PAD by applying an 8% lidocaine metered dose spray to the affected areas. Blood levels of lidocaine were minimal, and this technique may show promise for those affected with focal PAD pain.6 Medication The goal of pharmacotherapy is to reduce morbidity and to prevent complications. Anticoagulants Anticoagulants reduce thrombin generation and fibrin formation and minimize clot propagation. Heparin Augments activity of antithrombin III and prevents conversion of fibrinogen to fibrin. Does not actively lyse but is able to inhibit further thrombogenesis. Prevents reaccumulation of clot after spontaneous fibrinolysis. Adult 80 U/kg IV bolus, followed by infusion of 18 U/kg/h Follow-up Further Outpatient Care 1. Patients who have significant peripheral vascular disease but whose illness is not so severe or acute that it requires inpatient treatment may be discharged with appropriate follow-up. However, counsel these patients regarding the potential effects of various activities and medications on the course of their illness. Advise patients to stop smoking and to avoid cold exposures and medications that can lead to vasoconstriction, including medications used for migraines and over-thecounter medications. 2. Some recreational drugs (eg, cocaine) may have a deleterious effect on peripheral arterial tone, and betablockers may exacerbate the condition. 3. Consultation with providers who will be following the patient after ED discharge is advised when making decisions regarding the discontinuation of medications used for chronic medical conditions. Peripheral Arterial Occlusive Disease Introduction Background Claudication, which is defined as reproducible ischemic muscle pain, is one of the most common manifestations of peripheral vascular disease caused by atherosclerosis. Claudication occurs during physical activity and is relieved after a short rest. Pain develops because of inadequate blood flow. Pathophysiology Single or multiple arterial stenoses produce impaired hemodynamics at the tissue level in patients with peripheral arterial occlusive disease (PAOD), shown below. Arterial stenoses lead to alterations in the distal pressures available to affected muscle groups and to blood flow. Peripheral arterial occlusive disease. This angiogram shows a superficial femoral artery occlusion on one side (with reconstitution of the suprageniculate popliteal artery) and superficial femoral artery stenosis on the other side. This is the most common area for peripheral vascular disease. Under resting conditions, normal blood flow to extremity muscle groups averages 300-400 mm/min. Once exercise begins, blood flow increases up to 10-fold owing to the increase in cardiac output and compensatory vasodilation at the tissue level. When exercise ceases, blood flow returns to normal within minutes. In patients with PAOD, resting blood flow is similar to that of a healthy person. However, during exercise, blood flow cannot maximally increase in muscle tissue because of proximal arterial stenoses. When the metabolic demands of the muscle exceed blood flow, claudication symptoms ensue. At the same time, a longer recovery period is required for blood flow to return to baseline once exercise is terminated. Similar abnormal alterations occur in distal perfusion pressure in affected extremities. In normal extremities, the mean blood pressure drop from the heart to the ankles is no more than a few millimeters of mercury. In fact, as pressure travels distally, the measured systolic pressure actually increases because of the higher resistance encountered in smaller-diameter vessels. At baseline, a healthy person may have a higher measured ankle pressure than arm pressure. When exercise begins, no change in measured blood pressure occurs in the healthy extremity. In the atherosclerotic limb, each stenotic segment acts to reduce the pressure head experienced by distal muscle groups. Correspondingly, at rest, the measured blood pressure at the ankle is less than that of a healthy person. Once physical activity starts, the reduction in pressure produced by the atherosclerotic lesion becomes more significant and the distal pressure is greatly diminished. The phenomenon of increased blood flow causing decreased pressure distally to an area of stenosis is a matter of physics. Poiseuille calculated energy losses across areas of resistance with varying flow rates by using the following equation, in which Q is flow, v is viscosity, L is the length of the stenotic area, r is the radius of the open area within the stenosis, and k is constant: Resistance = pressure = Q8vL/kr4 Applying this equation, the pressure gradient is directly proportional to the flow and length of stenosis and inversely proportional to the fourth power of the radius. Therefore, while increasing the rate of flow directly increases the pressure gradient at any given radius, these effects are much less marked than those due to changes in the radius of the stenosis. As the radius is raised to the fourth power, it has the most dramatic impact on a pressure gradient across a lesion. This impact is additive when 2 or more occlusive lesions are located sequentially within the same artery. Frequency United States Atherosclerosis affects up to 10% of the Western population older than 65 years. With the elderly population expected to increase 22% by the year 2040, atherosclerosis is expected to have a huge financial impact on medicine. When claudication is used as an indicator, estimates are that 2% of the population aged 40-60 years and 6% older than 70 years are affected. Mortality/Morbidity The most feared consequence is severe limb-threatening ischemia leading to amputation. However, studies of large patient groups with claudication reveal that amputation is uncommon. Boyd prospectively followed 1440 patients with intermittent claudication for as long as 10 years and reported that only 12.2% required amputation.1 In the Framingham study, only 1.6% of patients with claudication reached the amputation stage after 8.3 years of follow-up. 1. Limb amputation largely depends on the number and severity of cardiovascular risk factors (ie, smoking, hypertension, diabetes). Continued smoking has been identified as the most consistent adverse risk factor associated with the progression of peripheral arterial occlusive disease (PAOD). Other factors are the severity of disease at the time of the initial patient encounter and, in some studies, the presence of diabetes. 2. As with most patients with vascular disease, survival is less than that of age-matched control groups. Coronary artery disease with a subsequent myocardial event is the major contributor to outcome. Predicted mortality rates for patients with claudication at 5, 10, and 15 years of follow-up are approximately 30%, 50%, and 70%, respectively. Race Peripheral arterial occlusive disease (PAOD) has no racial predilection. Sex 1. Intermittent claudication most commonly manifests in men older than 50 years. 2. Although younger patients may present with symptoms consistent with intermittent claudication, other etiologies of leg pain and claudication (eg, popliteal entrapment syndrome) must be strongly considered. Clinical History Intermittent claudication typically causes pain that occurs with physical activity. Determining how much physical activity is needed before the onset of pain is crucial. 1. Typically, vascular surgeons relate the onset of pain to a particular walking distance in terms of street blocks (eg, 2-block claudication). This helps to quantify patients with some standard measure of walking distance before and after therapy. 2. Other important aspects of claudication pain are that the pain is reproducible within the same muscle groups and that it ceases with a resting period of 2-5 minutes. 3. Location of the pain is determined by the anatomical location of the arterial lesions. Peripheral arterial occlusive disease (PAOD) is most common with the distal superficial femoral artery (located just above the knee joint), which corresponds to claudication in the calf muscle area (the muscle group just distal to the arterial disease). 4. When atherosclerosis is distributed throughout the aortoiliac area, thigh and buttock muscle claudication predominates. 5. The perceived significance of claudication is variable. Most patients appear to accept a decrease in walking distance as a normal part of aging. Investigators report that 50-90% of patients with definite intermittent claudication do not report this symptom to their clinician. 6. Atherosclerosis is a systemic disease process. Patients who present with claudication due to PAOD can be expected to have atherosclerosis elsewhere. A full assessment of the patient's risk factors for vascular disease should be performed. 7. The risk factors for PAOD are the same as those for coronary artery disease or cerebrovascular disease and include diabetes, hypertension, hyperlipidemia, family history, sedentary lifestyle, and tobacco use. 8. Smoking is the greatest of all the cardiovascular risk factors. The mechanism by which smoking causes or accentuates atherosclerosis is unknown. What is known is that the degree of damage is directly related to the amount of tobacco used. Counseling patients on the importance of smoking cessation is paramount in PAOD management. Physical Essential to the physical examination of a patient with claudication is a complete lower extremity evaluation and pulse examination, including measuring segmental pressures, as depicted in the image below. Atrophy of calf muscles, loss of extremity hair, and thickened toenails are clues to underlying peripheral arterial occlusive disease (PAOD). Peripheral arterial occlusive disease. Measuring segmental pressures. 1. 2. 3. Palpation of pulses should be attempted from the abdominal aorta to the foot, with auscultation for bruits in the abdominal and pelvic regions. This can be difficult in a patient who is obese, in whom palpable pulses may be hidden under a deep subcutaneous layer. Except in the rare case of a congenital absence of a pulse (eg, persistent sciatic artery), the absence of a pulse signifies arterial obstruction proximal to the area palpated. For example, if no femoral artery pulse is palpated, significant PAOD is present in the aortoiliac distribution. The same can be said if no palpable popliteal artery pulse is present because of existing superficial femoral artery occlusive disease. Patients who report intermittent claudication and have palpable pulses can present a clinical dilemma. If the history is consistent with typical claudication symptoms, the clinician can have the patient walk around the office (or perform toe raises) until the symptoms are reproduced and then palpate for pulses. The exercise should cause the atherosclerotic lesion to become significant and should diminish the strength of the pulses distal to the lesion. 4. When palpable pulses are not present, further assessment of the circulation can be made with a handheld Doppler device. An audible Doppler signal assures the clinician that some blood flow is perfusing the extremity. If no Doppler signals can be heard, a vascular surgeon should be immediately consulted. 5. Pressure measurements can be performed to gain objective data on the circulatory status. To obtain an accurate pressure reading, (1) place the pneumatic cuff around the ankle, (2) position the Doppler probe over the dorsalis pedis or posterior tibial artery, and (3) inflate the cuff to a reading above the systolic pressure and deflate. The systolic tone at the ankle vessel is the pressure recorded. A healthy person has no pressure drop from the heart to the ankle. In fact, the pressure at the ankle may be 10-20 mm Hg higher due to the augmentation of the pressure wave with travel distally. In patients with claudication, the measured pressure is diminished to some extent, depending on the severity of PAOD. 6. A useful tool in assessing a patient with claudication is the ankle-brachial index (ABI), which is calculated as the ratio of systolic blood pressure at the ankle to the arm. Determining the ABI provides an assessment of the impact that the PAOD is having on the patient. A normal ABI is 0.9-1.1. However, any patient with an ABI less than 0.9, by definition, has some degree of PAOD. The ABI decreases with worsening PAOD. One area of inaccuracy with the ABI is in patients with diabetes who have PAOD. Peripheral vessels in patients with diabetes may have extensive medial layer calcinosis, rendering the vessel resistant to compression by the pneumatic cuff. These patients should be referred to a vascular laboratory for further evaluation. Other Problems to Be Considered Some disease processes mimic claudication symptoms and must be excluded. They include the following: 1. Osteoarthritis: This is associated with arthritic pain that is variable from day to day and may be aggravated by certain weather patterns or movements. Rest does not relieve pain. 2. Venous disease: Described as a dull, aching pain that typically occurs at the end of the day or after prolonged standing, venous disease is not exacerbated by exercise. 3. Neurospinal disease: Pain occurs in the morning and is not relieved by short resting periods. Neurospinal pain is frequently relieved by leaning forward against a solid surface or by sitting. 4. Chronic compartment syndrome: This is rare. It is usually observed in runners and other athletes with large, developed calf muscles. Muscles swell during activity, leading to increased compartment pressure and decreased venous return. Consistent with claudication pain, this pain occurs with exercise and is relieved with rest. However, the type of exercise is at a more strenuous level and the recovery period is prolonged. 5. Popliteal entrapment syndrome: This syndrome is similar to intermittent claudication but is usually observed in active young people. The syndrome is caused by various abnormal anatomical configurations of the insertion of the medial gastrocnemius muscle head, which causes compression of the popliteal artery. Upon physical examination, tibial pulses may disappear when the knee is at full extension. Pain is aggravated with walking but not with running because knee extension is not as severe with running. 6. Reflex sympathetic dystrophy or minor causalgia: This is characteristically described as a burning pain. The superficial pain is often distributed along a somatic nerve and is often related to a past trauma in the extremity. 7. Diabetic neuropathy: Pain is due to a peripheral neuritis. Differentiation from intermittent claudication can be difficult because of accompanying skin discoloration and diminished pulses. An extensive neurologic evaluation is essential. 8. Venous thrombosis: Swelling and leg pain occur with walking. Pain is relieved by extremity elevation, which distinguishes this entity from arterial insufficiency. Workup Laboratory Studies A laboratory workup is only helpful for identifying accompanying silent alterations in renal function and elevated lipid profiles. Imaging Studies 1. Angiography still remains the criterion standard arterial imaging study used in the diagnosis of PAOD, as depicted in the image below. However, this test is usually reserved for when an intervention (either endovascular or traditional open surgery) is planned. 2. Monaco et al examined the effects of systematic (routine) coronary angiography, as shown below, on patients undergoing surgical treatment of peripheral arterial disease.2 Patients undergoing vascular surgery have a high-risk for cardiovascular complications and mortality. The authors found that routine coronary angiography had a positive impact compared with selectively determining if coronary angiography was needed. The routine coronary angiography improved survival (P=0.01) and no reports of death or cardiovascular events (P=0.003) occurred compared with those patients who were selectively chosen to have coronary angiography prior to vascular surgery. The authors recommend that multicenter trials confirm this finding in a larger population. 3. Magnetic resonance angiography (MRA) is useful for imaging large and small vessels. Although MRA was initially felt to provide inadequate images, this is no longer the case. With improved imaging capabilities, MRA can be used to not only diagnose but to help plan the type of indicated intervention. 4. Computerized tomographic angiography is another modality used to image arterial disease. Unfortunately, the study still requires a large amount of contrast media and requires an upgraded CT scanner to reconstruct helpful images. 5. Duplex ultrasonography is a method of evaluating the status of a patient’s vascular disease. Duplex scanning has the advantage of being noninvasive and requiring no contrast media. Unfortunately, duplex scanning is very technician dependent. Treatment Medical Care Treatment of claudication is medical, with surgery reserved for severe cases. 1. The goal of medical management is to impede the progression of peripheral arterial occlusive disease (PAOD). In patients who smoke, the most expedient way to impede the progress of PAOD is to stop tobacco use. Extensive evidence indicates that smoking cessation improves the prognosis. Improved walking distance and ankle pressure have been attributed to smoking cessation. 2. Exercise plays a vital role in the treatment of claudication. Patients reduce their daily walking because of claudication pain and fear of further damage. This leads to an increasingly sedentary lifestyle that is even more detrimental. Regular walking programs result in substantial improvement in most patients with claudication. Improvements have ranged from 80-234% in controlled studies. A daily walking program of 45-60 minutes is recommended. The patient is instructed to walk until claudication pain occurs, rest until the pain subsides, and repeat the cycle. While the exact mechanism for improvement in walking distance with exercise remains unknown, regular exercise is thought to condition muscles to work more efficiently (more extraction of blood) and increase collateral vessel formation. 3. Additional medical treatment includes control of the lipid profile, diabetes, and hypertension. Surgical Care Patients with limb-threatening ischemia or lifestyle-limiting claudication are referred to a vascular surgeon. Only then does evaluation warrant an arteriogram. Medication Daily aspirin is recommended for overall cardiovascular care. While standard dosages range from 81-325 mg/d, no consensus has been reached on the most effective dose. Pentoxifylline (Trental) shows promise. Numerous randomized trials have documented modest improvements in walking distance when compared with placebo treatment groups. Treatment can take 2-3 months to produce noticeable results. The use of clopidogrel bisulfate (Plavix) and enoxaparin sodium (Lovenox) in the treatment of this entity is increasing; however, further research is needed to establish clinical efficacy. Cilostazol (Pletal) has recently shown increasing promise in the treatment of intermittent claudication. Several randomized studies have shown benefits in increasing walking distances for both the distance before the onset of claudication pain and the distance before exercise-limiting symptoms become intolerable (ie, maximal walking distance). In a randomized, double-blind, placebo-controlled trial, O’Donnell et al assessed the vascular and biochemical effects of cilostazol therapy in individuals (n=80) with peripheral arterial disease. Arterial compliance, transcutaneous oxygenation, ankle-brachial index, and treadmill walking distance were measured. The cilostazol group had significant reduction in the augmentation index and also showed reduction in transcutaneous oxygenation levels compared with the placebo group. Mean percentage change in walking distance improved more in the cilostazol group from baseline compared with the placebo group. Lipid profiles were also improved in the cilostazol group. The results showed that cilostazol is an efficacious treatment of peripheral arterial disease. In addition to improving patients’ symptoms and quality of life, cilostazol also appeared to have beneficial effects on arterial compliance.3 In 2009, Momsen et al evaluated the efficacy of drug therapy in improving walking distance in intermittent 4 claudication. Their study determined that statins seemed to be the best in improving maximal walking distance. Cholesterol-lowering statin agents are beneficial in the medical therapy for peripheral arterial disease.5 In addition to effectively lowering blood cholesterol profiles, recent evidence from the Heart Protection Study showed that cholesterol-lowering statin agents (simvastatin) reduced the rate of first major vascular events (myocardial infarction, stroke, or limb revascularization), with the largest benefits seen in patients with peripheral vascular disease.6 The benefits were demonstrated regardless of the baseline cholesterol profile. As such, cholesterol-lowering statin agents should be considered for medical treatment in patients with peripheral arterial disease. Antiplatelet Agents Decrease overall risk of cardiovascular disease from myocardial infarction and stroke. Also improve walking distance by enhancing circulation. Aspirin (Anacin, Ascriptin, Bayer aspirin) Inhibits prostaglandin synthesis, which prevents formation of platelet-aggregating thromboxane A2. Adult 81-325 mg PO qd Clopidogrel (Plavix) Selectively inhibits ADP binding to platelet receptor and subsequent ADP-mediated activation of glycoprotein GPIIb/IIIa complex, thereby inhibiting platelet aggregation. Indicated for reduction of atherosclerotic events. Adult 75 mg PO qd Cilostazol (Pletal) Mechanism of effects on symptoms of intermittent claudication not fully understood. Cilostazol and several of its metabolites are PDE III inhibitors, inhibiting phosphodiesterase activity and suppressing cAMP degradation, with a resultant increase in cAMP in platelets and blood vessels, leading to inhibition of platelet aggregation and vasodilation, respectively. Reversibly inhibits platelet aggregation induced by various stimuli, including thrombin, ADP, collagen, arachidonic acid, epinephrine, and shear stress. Adult 100 mg PO bid at least 30 min before or 2 h after breakfast and dinner; consider 50 mg bid if coadministered with inhibitors of CYP3A4 (eg, ketoconazole, itraconazole, erythromycin, diltiazem) or with inhibitors of CYP2C19 (eg, omeprazole) Pentoxifylline (Trental) Indicated for treatment of patients with intermittent claudication due to atherosclerosis or other obstructive arteriopathies. Improves blood flow by increasing red blood cell deformability, which decreases viscosity of blood. Adult 400 mg PO tid Antilipemic Agents These agents are beneficial in lowering blood cholesterol profiles, which may reduce the rate of first major vascular events. Simvastatin (Zocor) Reduces cardiovascular heart disease mortality and morbidity (nonfatal myocardial infarction or stroke, revascularization procedures) in high-risk patients (ie, existing coronary heart disease, diabetes, peripheral vessel disease, history of stroke or other cerebrovascular disease). Competitively inhibits HMG-CoA, which catalyzes the rate-limiting step in cholesterol synthesis. Patients should be placed on a cholesterol-lowering diet; the diet should be continued indefinitely. Adult 40 mg PO hs if renal insufficiency not severe 5 mg PO hs in patients with severe renal insufficiency; not to exceed 10 mg/d when coadministered with fibrates (eg, gemfibrozil), niacin (>1 g/d), or cyclosporine; not to exceed 20 mg/d when coadministered with verapamil or amiodarone Follow-up Further Outpatient Care 1. Patients should be seen every 4-6 months to assess the effects of medical therapy. Review changes in walking distance, smoking habits, eating habits, and exercise performance. 2. Control hypertension and diabetes if necessary. A repeat pulse examination and ABI complete the follow-up evaluation. 3. Patients with worsening symptoms may require intervention and referral to a vascular surgeon. Complications 1. The most feared consequence is severe limb-threatening ischemia leading to amputation. However, studies of large patient groups with claudication reveal that amputation is uncommon. Boyd prospectively followed 1440 patients with intermittent claudication for as long as 10 years and reported that only 12.2% required amputation. In the Framingham study, only 1.6% of patients with claudication reached the amputation stage after 8.3 years of follow-up. Prognosis 1. Whether a patient progresses to limb amputation largely depends on the number and severity of cardiovascular risk factors (ie, smoking, hypertension, diabetes). 2. Continued smoking has been identified as the most consistent adverse risk factor associated with the progression of the disease. 3. Other factors are the severity of disease at the time of the initial patient encounter and, in some studies, the presence of diabetes. 4. As with most patients with vascular disease, survival is less than that of age-matched control groups. Coronary artery disease, with a subsequent myocardial event, is the major contributor to outcome. 5. Predicted mortality rates for patients with claudication at 5, 10, and 15 years of follow-up are approximately 30%, 50%, and 70%, respectively.