Improving Patient Safety with Team Training
advertisement

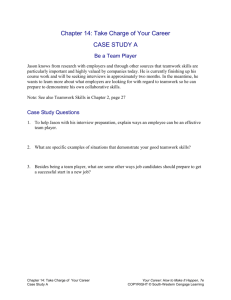
IMPROVING PATIENT SAFETY WITH TEAM TRAINING SANDON SAFFIER MD Simulation User Network OCTOBER 21, 2009 ssaffier@earthlink.net Objectives • Recall the overall risk for medical errors in the hospital environment and the top 10 specific Sentinel Events by type. • Recall the purpose of the 2009 Hospital National Patient Safety Goals. • List the components necessary for an effective team training program. • List the biggest challenges to implementing team training programs. National Patient Safety Goals Goal 2: Improve the effectiveness of communication among caregivers National Patient Safety Goal 2 • 2A For verbal or telephone orders or for telephonic reporting of critical test results, verify the complete order or test result by having the person receiving the information record and "read-back" the complete order or test result. • 2B Standardize a list of abbreviations, acronyms, symbols, and dose designations that are not to be used throughout the organization. • 2C Measure and assess, and if appropriate, take action to improve the timeliness of reporting, and the timeliness of receipt by the responsible licensed caregiver, of critical test results and values. • 2E Implement a standardized approach to “hand off” communications, including an opportunity to ask and respond to questions. Sentinel Events Communication Breakdowns are frequently the root cause of… undesirable outcomes 6 Sentinel Event Experience Sentinel events reviewed by the Joint Commission January 1995 through December 2006 531 events of wrong site surgery 520 inpatient suicides 488 operative/post op complications 385 events relating to medication errors 302 deaths related to delay in treatment 224 patient falls 153 deaths of patients in restraints 138 assault/rape/homicide 125 perinatal deaths/injury 94 transfusion-related events 85 infection-related events 72 deaths following elopement 66 fires 67 anesthesia-related events 51 retained foreign objects 763 “other” =4064 RCA’s PATIENT SAFETY MOVEMENT “To Err is Human” IOM Report MedTeams® ED Study 1995 JCAHO National Patient Safety Goals Institute for Healthcare Improvement 100K lives Campaign Executive Memo from President 1999 2001 TeamSTEPPS 2003 2004 Patient Safety and Quality Improvement Act of 2005 2005 2006 Medical Team Training 10 Slide 1-3 The Dynamic Research Corporation US ARMY AVIATION EXPERIENCE Crew coordination failures (FY84-89) 147 fatalities cost > $290 million. Mishaps involved highly experienced aviators with superior flight skills Failures attributed to: workload management communication task prioritization errors. MedTeams Medical Errors Reduction Research US Department of Defense Dynamics Research Corporation Harvard Risk Management Foundation ORGANIZATION OF THE TCC® • Maintain Team Structure and Climate • Plan and Problem Solve • Communicate With the Team • Manage Workload • Improve Team Skills 13 The MedTeamsTM Curriculum: Five Team Dimensions Team Dimension 1. Maintain Team Structure and Climate Primary Descriptors v v Establish leadership Organize the team v v Cultivate team climate DESC2 Script v v Situation Awareness Apply decision making processes v Cross monitoring 3. Team Communication v v v Maintain Situation Awareness Board Rounds Call Outs v v Check Backs Handoffs 4. Manage Workload v v Implement plan of care Prioritize tasks v Manage team resources and workload 5. Improve Team Skills v v Coaching Performance Evaluation v Engage in formal team improvement strategies 2. Plan & Problem Solve MedTeamsTM Concepts & Behaviors • • • • • • • • Team Climate DESQ2 Situational Awareness Cross Monitoring Advocacy & Assertion Two Challenge Rule Briefings Board Rounds • • • • • Call Outs Check Backs Handoffs Prioritization Planning Dr. Allen 16 Error Prevention Strategies • Cross-Monitoring • Advocacy and Assertion • Two-challenge Rule 17 Critical Language • Key phrases understood by all to mean “stop and listen to me – we have a potential problem” – When you hear this phrase, grab an elbow and join in the request for clarity • Allina – “ I need some clarity” • United Airlines CUS program – “I’m concerned…I’m uncomfortable…this is unsafe… I’m scared” • Politely Persist Information Transfer Techniques • Check-back • Call-out • Hand-off • SBAR 19 S-B-A-R • Situation • Background • Assessment • Recommendation S-B-A-R • Technique for communication between member of healthcare team • Framework for any conversation • Focused • Easy to remember • Esp. good for critical conversations Shared Mental Models • A mental model is a mental picture or sketch of the relevant facts and relationships defining an event, situation, or problem • The same mental model held by members of a team is referred to as a shared mental model 22 Shared Mental Model 23 Situational Awareness …the state of knowing the current conditions affecting the team’s work 25 RED FLAGS FOR LOSS OF SITUATIONAL AWARENESS • Ambiguity • Reduced/poor communication • Confusion • Trying something new under pressure • Deviating from established norms Michael Leonard, MD • • • • • • Verbal violence Doesn’t feel right Fixation Boredom Task saturation Being rushed/behind schedule Pre-procedural Briefing 27 Briefing • An exchange of concise and relevant information-getting on the same page • Communicating the plan • Briefings aid in: – Knowing the plan – Allowing for anticipation of problems with contingency plans – Monitoring a situation, watching for red flags Briefing • Other Situations to Consider Briefing – New Team Members – Fatigue or staffing challenges – Experienced and novices working side by side – Cultural differences Briefing • Key Elements – – – – – – – – – Got person’s attention Made eye contact, faced person Introduced self Use person’s name--familiarity is key Asked knowable information Explicitly asked for input Provided information Talk about next steps Encourage ongoing monitoring and cross checks Debriefing • • • • Plus / Delta Event Review Shift Review Situational Teaching Dr. Bridgeton 32 Comprehensive Unit Safety Program (CUSP) 1. Assess culture of safety -SAQ • Engage 2. Educate on Science of Safety 3. Identify unit safety concerns • Educate 4. Executive adopts a unit –Executive WalkRounds • Execute 5. Prioritize improvement efforts 6. Implement improvements • Evaluate 7. Share stories / disseminate results 8. Reassess culture - SAQ Reference: Peter Pronovost, et al. Implementing and Validating a Comprehensive Unit-Based Safety Program. SAQ Background • The SAQ collects input from “front-line” personnel to determine the strengths and weaknesses of organizations. – Used in medical, aviation, maritime, rail & military settings • Administered in over 500 hospitals (USA, United Kingdom, Switzerland, Germany, Italy, Turkey and New Zealand) – SAQ is a reliable tool and formally validated: • Aviation: linked to pilot performance, # of errors, % errors trapped (Helmreich, Foushee, Benson & Roussini, 1986; Sexton & Klinect, 2001) • High Speed Rail: linked to train incident and accident rates (Itoh & Andersen, 1999) • Medicine: linked to LOS, error rates & nurse turnover rates (Pronovost et al. 2002; Sexton, 2002) Bryan Sexton, Ph.D Teamwork Disconnect •RN: Good teamwork means I am asked for my input •MD: Good teamwork means the nurse does what I say •MD –RN: Different Communication Styles • Nurses are trained to be narrative and descriptive • Physicians are trained to be problem solvers “ what do you want me to do” – “ just give me the headlines” • Complicating factors: gender, national culture, the pecking order, prior relationship • Perceptions of teamwork depend on your point of view Physicians and RN Collaboration 100 90 88% 80 83% 70 90% 93% 60 50 40 48% 48% 54% 59% 30 20 10 0 RN rates Physician Bryan Sexton, Ph.D. Physician rates RN Teamwork level felt to be “high” Sexton, British Medical Journal, 2000 Believe that decisions of the “leader” should not be questioned Sexton, BMJ, 2000 Executive Perceptions vs. Frontline Perceptions: Executives overestimate: Teamwork Climate 4X Safety Climate 2.5X Executive Confidence vs. Executive Accuracy: -Often wrong but rarely in doubt… -Currently no incoming data-streams -Halo Effects -Frontline data fills the gap 40 Recommendations for Improving Teamwork & Safety Climate (For Clinical Areas With < 60% Agreement) TEAMWORK CLIMATE Morning/Shift Briefings Daily Goals Shadowing Exercise OR Briefings SBAR Use Critical Language (Start a “Grab an Elbow” campaign) Simulation Team Training Culture Checkup Tool Reach out within this hospital • Consult with other clinical areas that have 80% teamwork climate or higher, as they have a consensus of excellence SAFETY CLIMATE Executive Partnership Training and certification program • Use this for your lowest scoring clinical areas first, as it is a powerful intervention, more targeted than traditional executive walkrounds Hero Form (Feedback from Frontline Workers) Root Cause Lite Science of Safety Training • 45 Minute online course; free registration is required • http://distance.jhsph.edu/trams/index.cfm?event=tr aining.launch&trainingID=72 • Culture Checkup Tool Reach out within this hospital • Consult with other clinical areas that have 80% safety climate or higher, as they have a consensus of excellence 41 Bryan Sexton, Ph.D So Where’s the Proof? Proven Results and Patient Safety ED Observed Errors Length of ICU Stay After Team Training 35 30 Avg. Length of Stay (days) Average Rate of Errors 2.4 Exp 25 Control 55% Reduction 20 15 10 5 2.2 1.8 Pre-Teamwork Training Post-Teamwork Training % Re du cti on 1.6 1.4 1.2 1 0 50 2 June July August Sept Oct Nov Dec Jan Feb March April May (Pronovost, 2003), Johns Hopkins Journal of Critical Care Medicine (Morey, 2002), Dynamics Research Corporation Health Services Research L&D Adverse Outcomes OR Teamwork Climate and Postoperative Sepsis Rates (Weighted Adverse Outcome Score) (per 1000 discharges) 18 16 50% Reduction 14 12 Group Mean AHRQ National Average 10 Low Teamwork Climate 8 6 Mid Teamwork Climate 4 High Teamwork Climate 2 0 (Sexton, 2006), Johns Hopkins Teamwork Climate Based on Safety Attitudes Questionnaire Low High (Mann, 2002), Beth Israel Deaconess Medical Center 43 Contemporary OB/GYN Benjamin P. Sachs, MB, BS Perinatal Research Outcomes • Beth Israel Deaconess (Sachs) – Reduced rate of adverse outcomes • 53% over 4 years – Reduced cases in litigation • 30-40% in 2yrs – “Severe” cases reduced • from 45% to 25% – Able to reduce reserves • by 50% – Process Measures: emergency Cesarean-Sections “Decision to Incision” 18 minutes CHW Perinatal Patient Safety Pursuit • Assess– Climate of Safety Scores--SAQ – Facility Readiness • Education – Teamwork/Communication – Executive Walk Rounds – NICHD Language – Fetal Monitoring Competence • Clinical Practice Teamwork Training & Simulation: C+ • Emerging evidence is mixed but hopeful • Lots of targets – Improve procedures – Standardize communications – Dampen down hierarchies • Where is the money? Robert Wachter, MD Observation I 50 Observation II 51 Grassroots Patient Safety Tell me and I forget, Show me and I remember, Involve me and I understand. -Chinese Proverb 53