Hyperbilirubinemia
advertisement

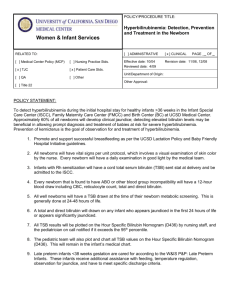
HYPERBILIRUBINEMIA and its TREATMENT By: Evgenia Klourfeld (evrblu@hotmail.com) Candy Pletzer (pletzerc@hotmail.com) Jane Lui (janelui@hotmail.com) Jan. 27, 2004 PHM 226, Example Instructor: Dr. Jeffrey Henderson What is Bilirubin? Is a bile pigment Is lipid soluble Is a product of heme metabolism Heme Metabolism Hemoglobin – 80% O2 Myoglobin Cytochrome P450s Hemoproteins Heme Fe3+ + CO NADP+ NADPH + H+ Heme Oxygenase Biliverdin Biliverdin Reductase Macrophage of the reticuloendothelial system Modified from Ganon, W.F. Review of Medical Physiology, (6th ed.). Bilirubin Blood The Fate of Bilirubin… Plasma Hepatic Cell Bile Alb B ? Alb B + GST B :GST B + UDPGA UGT1A1 CB sER Alb = albumin B = bilirubin GST = glutathione-S-transferase UDPGA = uridine diphosphoglucuronic acid; CB = conjugated bilirubin UGT1A1 = UDP-glucuronosyltransferase 1A1 MRP2 = Multi-drug Resistance Protein 2 Adapted from Harrison’s 15th Ed. “Principles of Internal Medicine”, 2001. MRP2 Bilirubin Excretion Liver B Enterohepatic circulation CB Bile B-glucoronidase CB bacteria Intestines B bacteria Urobilinogen ox Urobilin Stercobilingogen Stercobilin feces Bilirubin Excretion Liver B CB Kidney Enterohepatic circulation Bile B-glucoronidase CB Urobilinogen B bacteria bacteria Urobilinogen Urobilin ox Urine ox Urobilin Stercobilingogen Stercobilin Intestines feces Hyperbilirubinemia Interferences at any one of the points of bilirubin processing described above can lead to a condition known as HYPERBILIRUBINEMIA. As the name implies this disease is characterized by abnormally elevated levels of bilirubin in the blood. SYMPTOMS o Yellowing of the skin, scleras (white of the eye), and mucous membranes (jaundice) o Detectable when total plasma bilirubin levels exceed 2mg/100mL AHHH!!! I have symptoms of hyperbilirubinemia!!! Causes: 1. 2. 3. 4. 5. Increased bilirubin production Reduced bilirubin uptake by hepatic cells Disrupted intracellular conjugation Disrupted secretion of bilirubin into bile canaliculi Intra/extra-hepatic bile duct obstruction Lead to increases in free (unconj.) bilirubin Result in rise in conj. bilirubin levels 1) INCREASED BILIRUBIN PRODUCTION (unconj. Hyperbilirubinemia) Hemolysis Increased destruction of RBCs eg sickle cell anemia, thalassemia Drastic increase in the amount of bilirubin produced Unconj. bilirubin levels rise due to liver’s inability to catch up to the increased rate of RBC destruction Prolonged hemolysis may lead to precipitation of bilirubin salts in the gall bladder and biliary network result in formation of gallstones and conditions such as cholecystitis and biliary obstruction Other Degradation of Hb originating from areas of tissue infarctions and hematomas Ineffective erythropoiesis 2) DECREASED HEPATIC UPTAKE (unconj. Hyperbilirubinemia) Several drugs have been reported to inhibit bilirubin uptake by the liver e.g. novobiocin, flavopiridol Hepatic cell Plasma Alb Bile B B + GST Alb B :GST B + UDPGA CB UGT1A1 sER MRP2 3) DISRUPTED INTRACELLULAR CONJUGATION (unconj. Hyperbilirubinemia) Neonatal jaundice occurs in 50% of newborns fetal bilirubin is eliminated by mother’s liver causes: hepatic mechanisms are not fully developed resulting in decreased ability to conjugate bilirubin rate of bilirubin production is increased due to shorter lifespan of RBCs Acquired disorders hepatitis, cirrhosis impaired liver function 3) DISRUPTED INTRACELLULAR CONJUGATION (unconj. Hyperbilirubinemia) Crigler-Najjar Syndrome, Type I (CN-I) recessive allele; mutation-induced loss of conjugating ability in the critical enzyme glucuronosyltransferase CN-II greatly reduced but detectable glucuronosyltransferase activity due to mutation (predominantly recessive); enzymatic activity can be induced by drugs Gilbert’s Syndrome glucuronosyl transferase activity reduced to 10-30% of normal; also accompanied by defective bilirubin uptake mechanism Plasma Alb Hepatic cell Bile B B + GST B Alb B :GST CB + UDPGA UGT1A1 sER MRP2 4) DISRUPTED SECRETION OF BILIRUBIN INTO BILE CANALICULI (conj. Hyperbilirubinemia) Dubin–Johnson Syndrome mild conj. hyperbilirubinemia, but can increase with concurrent illness, pregnancy, and use of oral contraceptives; otherwise asymptomatic Inability of hepatocytes to secrete CB after it has formed Due to mutation in the MRP2 gene (autosomal recessive trait) Rotor Syndrome Autosomal recessive condition characterized by increased total bilirubin levels due to a rise in CB Caused by a defect in transport of bilirubin into bile Alb Hepatic cell Plasma Bile B B + GST B Alb B :GST + UDPGA CB UGT1A1 sER MRP2 5) Intra/extra-hepatic bile duct obstruction Intra-hepatic Obstruction of bile canaliculi, bile ductules or hepatic ducts Extra-hepatic Obstruction of cystic duct or common bile duct Cholecystitis Obstruction causes backup and reabsorption of CB which results in increased blood levels of CB Treatment & Therapeutic Considerations **PHOTOTHERAPY** Through absorption of the wavelengths at the blue end of the spectrum (blue, green and white light), bilirubin is converted into water-soluble photoisomers. This transformation enhances the molecule’s excretion into bile without conjugation. PHENOBARBITAL This drug is not approved by FDA for use in neither adult nor pediatric hyperbilirubinemia patients, due to possibility of significant systemic side-effects. Exact pathway is not known, but it is believed to act as an inducing agent on UDPglucuronosyltransferase, thereby improving conjugation of bilirubin and its excretion. ALBUMIN A 25% infusion can be used in treating hyperbilirubinemia (esp. due to hemolytic disease). It is used in conjunction with exchange transfusion to bind bilirubin, enhancing its removal. CLOFIBRATE (ATROMID-S) This drug has been shown to reduce bilirubin levels via an unknown mechanism. Clofibrate is also associated with increased risk of developing cholelithiasis, cholecystitis, as well as functional liver abnormalities, which can worsen hyperbilirubinemia. **PERCUTANEOUS TRANSHEPATIC CHOLANGIOGRAPHY** Allows extraction of stones and thus removal of the source of obstruction when present. ADVERSE THERAPEUTIC EFFECTS Flavopiridol – can induce hyperbilirubinemia. It shares Novobiocin – inhibits the UDP-glucuronosyltransferase Valspodar – causes an increase in bilirubin levels by P- the glucuronidation pathway that is involved in bilirubin conjugation, effectively reducing the amount of bilirubin that can be processed by the hepatic cells at any given time. activity, leading to hyperbilirubinemia. glycoproteins in the biliary canaliculi, thus interfering with bilirubin transport. REFERENCES 1. 2. 3. 4. 5. 6. 7. 8. 9. Braunwald, E., Fauci, A.S., Kasper, D.L. Harrison’s Principles of Internal Medicine, (15th ed.). McGraw-Hill Medical Publishing Division: New York, 2001. CPS Compendium of Pharmaceuticals and Specialties, (32nd ed.). Canadian Pharmaceutical Association: Ottawa, 1997. Ganong, W.F. Review of Medical Physiology, (6th ed.). Lange Medical Publications: Los Altos, 1973. MICROMEDEX. Mims, L., Gooden, D.S. Phototherapy for neonatal hyperbilirubinemia: a dose response relationship. Phys. Med. Biol. 1974;19: 263. www.aw-bc.com/mathews/ch21/bilirubi.htm www.emedicine.com/med/topic1065.htm www.emedicine.com/med/topic1066.htm www.rxlist.com/cgi/generic2/clofibrate_wcp.htm#P