Psychiatric Emergency
advertisement

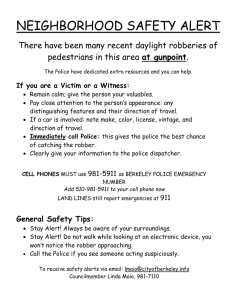
2nd Mental Health Case Manager Workshop 2012 Psychiatric emergency: Priorities for intervention. Session Outline Psychiatric emergency: What Where Who Police Involvement The Emergency Department Management of acute behavioural disturbance Psychiatric emergency. Severe behavioural disturbance: Aggression Self harm/Suicide Related Medical Emergencies: Intoxication Side effects. Where do psychiatric emergencies happen? In the community! In Emergency Department. In the inpatient unit. Who responds? Police Ambulance Community mental health Citizens Why? What do they do? What should they do? NSW Police: Mental health interactions 2000-2007 NSW Police Mental Health Intervention Team Comprehensive four day training program Police are trained in signs and symptoms of mental illness, Ambulance procedures, risk assessment, child and adolescent disorders, medications, personality disorders, substance abuse, legislation and communication techniques 2 Consumers and a carer also speak about their lives and what is is like to live with and care for someone with a mental illness Role play scenarios are used to allow police to put into practice the information they have learnt – role players are clinical health workers The Emergency Department The Emergency Department Macarthur presentations. Role of the ED The role of the Emergency Department is to diagnose and treat acute and urgent illnesses and injuries. (Peninsula health Victoria.) The role of emergency departments is to care for emergencies. An emergency is when an illness or injury is serious and requires urgent attention. SESAHS NSW) Management of acute and urgent aspects of illness and injury affecting patients of all age groups, with a full spectrum of undifferentiated physical and behavioural disorders. (The International Federation of Emergency Medicine) Role of the ED in psychiatric intervention. • • • • De-escalate Maintain safety Assess Treat Factors That Determine Response. Level of risk: To self To others Level of agitation Length of time the patient is expected to remain in the department. Stigma. Agitation and Disturbed Behaviours Severe anxiety associated with motor restlessness. (Kaplan & Sadock 1998) Internal tension associated with excessive motor activity eg. Pacing, restlessness, wringing hands, increased verbalisation, hypervigilance,threatening manner. (Centre for mental health 2001) In the context of psychotic features? Antipsychotic Medication in the ED Neuroleptization Rapid tranquilization Haloperidol Benzodiazepines Treatment Goals Prevention of harm Controlling disturbed behaviour Suppressing symptoms Effecting rapid return to best level of functioning Developing a therapeutic alliance Neuroleptic Side-effects Dystonia Akathisia Neuroleptic Malignant Syndrome QTc Interval prolongation Risperidone 2mg Risperidone + 2 mg Lorazepam = 5mg IM Haloperidol + 2mg IM Lorazepam. (Currier & Simpson 2001) Antipsychotic action at 30, 60 & 120 minute follow up intervals. Orthostatic Hypotension & Akathisia apparent with rapid titration. Olanzapine 5-20mg = or > Haloperidol for control of psychotic symptoms & agitation. More sedating than other Atypicals. Very low risk of EPSE. No requirement for titration. Variable administration. IM preparation available. Oral medication is always first line. Lorazepam is preferred benzodiazepine in some services. IM Midazolam most common +/- Oral or IM antipsychotic. Droperidol is used in some health services. IV protocols have changed little in the past 20+ years. Thanks for your Attention