TO INTEGRATE
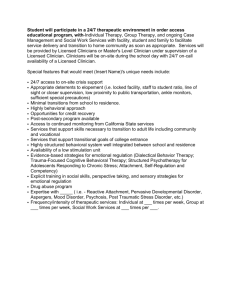
advertisement

TO INTEGRATE -- OR HOW? A Decision Model for Practices Charles Cooper, PhD Director of Professional Affairs North Carolina Psychological Association APA State Leadership Conference March 10, 2013 THE EXPECTED ENVIRONMENT: 2 THE MAUER MODEL THE EXPECTED ENVIRONMENT Low Physical Health Risk/Complexity High Physical Health Risk/Complexity High Behavioral Health Risk/Complexity QUADRANT II QUADRANT IV Clients served in primary care and specialty mental health settings Clients served in primary care and specialty mental health settings For treatment of: bipolar disorder, chronic pain Note: with MH stable, care can be transitioned to PCP For treatment of: schizophrenia, metabolic syndrome or hepatitis C QUADRANT I QUADRANT III Clients served in primary care setting Clients served in primary care setting For treatment of: moderate alcohol abuse, fibromyalgia For treatment of: moderate depression, uncontrolled diabetes Low Behavioral Health Risk/Complexity 3 Integrated Care – The Individual Model A Two-Dimension Model for Decision Making I. Top Margin: Level of Integration occurs along a spectrum, from No Integration to Full Integration. II. Side Margin: Actions would be based on the clinician's inclination towards integration and where the clinician is in his or her career. 4 The Individual Decision Model Level of Integration No Integration Ultra light Integration Light Integration Moderate Integration Full Integration Maintain current practice format while keeping watchful eye on developments Greatly improve communication with targeted primary care referral sources Offering contracted services to primary care, medical homes, or ACOs “Co-Location” maintaining part or all of a practice within a primary care setting Assuming an employed position within an integrated setting Clinician Practice Qualities Early Career inclined toward integration Early Career disinclined toward integration Mid Career Inclined toward integration Mid Career disinclined toward integration Late Career inclined toward integration Late Career disinclined toward integration 5 Level of Integration No Integration Ultra light Integration Light Integration Moderate Integration Full Integration Take advantage of learning opportunities to strengthen skills that might allow future move closer to integrated systems Identify target primary care practices; build relationships; determine what specific kinds of integration are mutually beneficial and clinically valuable; Then build the collaboration Be on high alert regarding integrating systems and design ways to serve patients in medical homes while continuing independent practice. Build your skills to address unmet needs of integrating systems Acquire specialty training if possible targeting some particular area of health psychology in which you can demonstrate high levels of skill Survey primary care provider community looking for colocation possibilities Acquire specialty training if possible targeting some particular area of health psychology in which you can demonstrate high levels of skill Survey fully integrated systems and their needs for behavioral health Clinician Practice Qualities Early Career inclined toward integration 6 Level of Integration No Integration Ultra light Integration Light Integration Moderate Integration Full Integration Develop a niche that will likely grow regardless of integration. Be prepared to change strategy should local system developments require it. Identify one or more niches that hold promise for creating practice distinction. Build on that niche and be aware of how it could be affected by integration in the larger health system Take advantage of medical homes and integrated systems and their organized care management. Seize marketing opportunities with care managers for niche offerings and specialized services not offered in the “home” Take advantage of rapidly growing awareness of unmet behavioral needs of primary care patients. Seize marketing opportunities by offering niche services especially tailored to those unmet needs. Take advantage of integrated systems and their organized care management. Seize opportunities with care coordinators for marketing your niche offerings and specialized services not offered in the “home” Clinician Practice Qualities Early Career disinclined toward integration 7 Level of Integration No Integration Ultra light Integration Light Integration Moderate Integration Full Integration Capitalize on strengths of your current practice. Be prepared to change strategy should local developments require it. Identify target primary care practices; build relationships; determine what specific kinds of integration are mutually beneficial and clinically valuable; Then build the collaboration Take advantage of your practice reputation in the community. Watch for compatible primary care or “medical home” organizations – particularly ones with likely unmet needs for behavioral services for which they may need to refer out. Take advantage of your practice reputation in the community. Survey primary care provider community looking for compatible colocation possibilities. Build relationships and explore how to put a “toe in the water” Capitalize and build on skills and interests that may be sought by fully integrated systems. Acquire additional training in areas that may be in demand within those systems. Get to know the developing integrated systems and their needs. Build relationships. Clinician Practice Qualities Mid Career inclined toward integration 8 Level of Integration No Integration Ultra light Integration Light Integration Moderate Integration Full Integration Capitalize on strengths of your current practice. Monitor your payer mix. Exploit niche opportunities. Be prepared to change strategy should local developments require it. Identify target primary care practices; build relationships; determine what current features of your practice (or reasonable adjustments in your procedures) might attract referrals; Then build the collaboration. Take advantage of medical homes and integrated systems and their organized care management. Seize marketing opportunities with care managers for niche offerings and specialized services not offered in the “home” Take advantage of rapidly growing awareness of unmet behavioral needs of primary care patients. Seize marketing opportunities by offering niche services especially tailored to those unmet needs. Take advantage of integrated systems and their organized care management. Seize opportunities with care coordinators for marketing your niche offerings and specialized services not offered in the “home” Clinician Practice Qualities Mid Career disinclined toward integration 9 Level of Integration No Integration Ultra light Integration Light Integration Moderate Integration Full Integration Take advantage of reputation, “health orientation” and relationships. If necessary, adjust practice to respond to new referral patterns that may emerge with some large integrating systems Identify target one or more primary care practices; Take advantage of reputation, “health orientation” and relationships to strengthen collaboration, communicatio ns, and coordination of care with mutual patients Take advantage of your practice reputation in the community. Watch for compatible primary care or “medical home” organizations – particularly ones with likely unmet needs for behavioral services for which they may need to refer out. If feasible, consider locating practice very near primary care setting or find other ways to reduce barriers to easy, “warm” referrals. Regular consultation / contact with primary care providers can approximate co-location If skills, interests, financial rewards and other compatibilities make practice “inside” a fully integrated setting desirable, explore part of full time affiliation with such a setting. Assess your readiness to accept significant work culture change. Clinician Practice Qualities Late Career inclined toward integration 10 Level of Integration No Integration Ultra light Integration Maintain awareness of changes that may occur and diversify referral and payer mixes. Enhance niche aspects of practice. Maintain awareness of changes that may occur and diversify referral and payer mixes. Enhance niche aspects of practice. Be open to making reasonable adjustments to foster referrals from primary care providers Light Integration Moderate Integration Full Integration Clinician Practice Qualities Late Career disinclined toward integration Maintain Watch with awareness. Do interest. an occasional assessment of yourself and of the developments in integrating health systems to ascertain if it is worth building relationships with, marketing to, and collaborating with primary health providers. See if what you already do can “sell” to them. Watch with interest. 11 Integrated Care – The Practice Model A Two-Dimension Model for Decision Making I. Top Margin – Level of Integration: occurs along a spectrum, from No Integration to Full Integration. II. Side Margin – Economic/Business Factors: strategic choices and actions would be based factors of “supply” and “demand” and an analysis of strengths, weaknesses, opportunites and threats, (SWOT). 12 Level of Integration No Integration Ultra light Integration Light Moderate Full Integration Integration Integration Business Conditions for Decision Making Demand •High and clear demand •Murky, ambiguous or unclear demand •Nil, low or mismatched demand Supply •Excellent •Uncertain, or Underdeveloped •Inadequate Additional Factors •SWOT •Wildcards 13 Level of Integration No Integration Ultra light Integration Light Integration Moderate Integration Full Integration Demand Conditions High and clear demand Strong demand with ready customers who have clear needs Murky, ambiguous or unclear demand Demand is Ambiguous, Still undeveloped but with significant potential Nil, low or mismatched demand Demand is non-existent or completely mismatched to your practice 14 Integrated Care Table Practice Decision Model Demand: High and Clear None Collaboration Full Integration Spectrum Build relationships, Explore needs, Match resources to need, Make concrete proposals, Work out logistics, potential roles and workflow, Develop contracts, Coordinate and/or educate Murky, Ambiguous, or Unclear Demand Establish early communications with potential collaborators; Explore mutual interests; Engage in “Integration Education”; Conduct needs assessments Low, Nil, or Completely Mismatched Demand Engage the primary care community; Find ways to start communications; Work on joint projects; Participate in basic education in “Integration Awareness Building” 15 Level of Integration No Integration Ultra light Integration Light Integration Moderate Integration Full Integration Supply Conditions Excellent Supply of well trained health psychologists who would be well matched and motivated to integrate Uncertain or undeveloped supply of appropriate clinicians motivated to integrate Inadequate Supply that is nil, ill-matched, or unmotivated to integrate 16 Integrated Care Table None Collaboration Full Practice Decision Model Integration Spectrum Supply: Excellent, Well-matched, or Develop contracts; Build promising well-motivated relationships; Introduce health psychologists to potential collaborators; Start joint ventures; Offer services that might lead to contractual integrations Uncertain, or Underdeveloped Conduct self-assessments in your practice; Procure training in behavioral health and/or recruit health psychologists; Develop services linked to primary care that start a “track record” for your practice in integrated care Nil, completely Unmotivated, or illmatched Look for hidden talent within the practice; Augment skills, retrain, or recruit behavioral health specialists 17 LEVEL OF INTEGRATION No Integration Ultra light Integration Light Integration Moderate Integration Full Integration Maintain current practice format while keeping watchful eye on developments Greatly improve communication with targeted primary care referral sources Offering contracted services to primary care, medical homes, or ACOs “Co-Location” maintaining part or all of a practice within a primary care setting Assuming an employed position within an integrated setting ADDITIONAL FACTORS STRENGTHS E.g., Management Capabilities are strong; reputation good and relationships excellent WEAKNESSES E.g., Risk Tolerance is low; technology and IT is underdeveloped OPPORTUNITIES E.g., To establish a strong referral network with primary care THREATS E.g., Gradual loss of referrals as medical homes pick treat internally WILDCARDS Timing (Especially bad or good) Internal and external cultures 18 Integrated Care Table Practice Decision Model SWOT: None Collaboration Full Integration Spectrum Strengths Build upon and exploit strengths Weaknesses Correct or “design around” weaknesses Opportunities Orient toward opportunities Threats Protect against threats Wildcards: Internal Culture Time Considerations Competition Prepare for the unexpected!!! 19 A Case Study in North Carolina A Case Study – The Demand Side • The Business Environment o o o o o The Research Triangle Area of NC (3 major cities) Large University-Based Health Systems Large Independent Practice Association (IPA) History of care integration in primary care settings (Medicaid) Interest in care integration by commercial carrier (Private Sector) 21 A Case Study – The Supply Side • HRC Behavioral Health & Psychiatry, PA Chapel Hill and Raleigh, NC 22 A Case Study – Early Days • • • • • • • Founded 1967 25 to 30 clinicians in two cities Multidisciplinary approach EAP Experience / Contract Experience General reputation in community Two experienced health psychologists High motivation to integrate (co-locate +) 23 A Case Study – The Supply Side • The Practice Group • • • Long history in the community Multi-specialty group practice o Psychologists ………………………………………………………..14 Health Psychologists ………………………………………….2 o Psychiatrists …………………………………………………………. .6 Mid-level providers (Physician’s Assistants)…………………. .2 o Social Workers………………………………………………………....2 o Licensed Professional Counselor (substance abuse specialist)….1 Total ……………………..…………………………….27 24 The HRC Integration Story: Phase I • Pre-Integration Days o Referral Promotion: Internal discussion and monitoring the local landscape to promote referrals o Relationship Building: with a nearby primary/urgent care practice, “The Family Doctor” o My Job as Director of Professional Affairs >> SLC attendance >> awareness of need to develop practice as business 25 • The HRC Integration Story: Phase II Early Integration • • • Conversations with medical director of biggest commercial carrier in area Discovered carrier’s strong interest in integration Invited conversations with nearby urgent care practice, “The Family Doctor” o How could we be more responsive? o How can we communicate most effectively? o How could we be better “integrated”? Discovery of a “Go Between” o Lawyer with interest in integrated care, provider group contracting, and compliance with referral and kick-back issues under federal and state law 26 • The HRC Integration Story: Phase III Integration Matures o o o o o o HRC contracts with Family Doctor practice to be their behavioral resource for “Medical Home” status The “go-between” Steve Shaber (Poyner & Spruill Raleigh) identifies prospective primary care practice HRC identifies a clinician from our group who wants to colocate. Discussions begin with Family Medical Associates of Raleigh (Key IPA) Contracting begins re: space, support services, coordination of health records, money flows, etc. Consultant/representative sent to the commercial carrier 27 The HRC Integration Story: Phase IV • Current Challenges: o Entering primary care culture o Clarifying expectations o Refining contracts Rent Services o Fixing logistics, documentation, and information flows o Dealing with insurance incompatibilities (panels and managed care problems) o Dealing with payer + CPT code constrictions Eg, Health and Behavior Code 96150 – limit to 3 28 The HRC Integration Story: Phase IV • Current Challenges, cont’d: o Dealing with time demands for unpaid services Hallway consults Uninsured patients and network incompatibility o How to demonstrate value to primary care patients o Implementation Science Initiative o How to reconfigure the “mother practice” to accommodate co-location Less need for space in original psychology practice Challenges to cohesion and connection to original group 29 Q&A • What are the implications for other kinds of • • • practices? What are implications for independent practice? How can our state, provincial, and territorial associations help practitioners? How can APA help? 30 Resources • • • • • • Collins, C et.al. Evolving Models of Behavioral Health Integration in Primary Care, Milbank Memorial Fund, May 2010. http://www.milbank.org/reports/10430EvolvingCare/EvolvingCare.pdf Community Care of North Carolina (CCNC). https://www.communitycarenc.org/population-management/behavioral-health-page/ Mauer, B. 2006. Behavioral Health/Primary Care Integration: The Four Quadrant Model and Evidence-Based Practices. Rockville, MD: National Council for Community Behavioral Healthcare. Mechanic, David. Seizing Opportunities Under The Affordable Care Act For Transforming The Mental And Behavioral Health System. Health Affairs, 31, no.2 (2012): 376-382 Trend Watch; Bringing Behavioral Health into the Care Continuum: Opportunities to Improve Quality, Costs and Outcomes. American Hospital Association. January 2012 Multiple articles on integrated care at APA’s Practice Central http://www.apapracticecentral.org/ (Search terms: “Integrated Care”) 31