Crohn*s disease - Professional Nursing Portfolio Narjess Yazback
advertisement

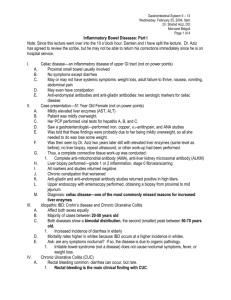
CROHN’S DISEASE Marlee Griggs & Narjess Yazback, INTRODUCTION: WHAT IS CROHN'S DISEASE? Crohn disease (CD) is a chronic regional enteritis that can affect any part of the gastrointestinal tract (GI) from mouth to anus but it is most commonly seen in the terminal ileum (Rendi, 2013). This inflammatory bowel disease (IBD) was initially described in 1932 by Crohn, Ginzburg, and Oppenheimer, but it was not distinguished from Ulcerative colitis (UC) until 1959. The difference is that UC typically affects lower parts of the GI: colon and rectum (Rendi, 2013) Prevalence & Incidence Approximately 7 per 100,000 people in the US are affected with CD. Members of European Jewish heritage have a 3-5 times higher prevalence than the general population. Two peaks of incidence are seen: Early adulthood (teens-20’s) & elderly (60-70’s) CD is mainly seen in urban areas and northern climates, but it is increasingly growing in regions such as Africa, South America, and Asia (Rendi, 2013). Smokers are more likely to develop CD than nonsmokers (National Digestive Diseases Information Clearinghouse (NDDIC), 2013). PATHOPHYSIOLOGY Crohn’s disease is an inflammatory bowel disease (IBD) meaning it causes irritation, inflammation and swelling that can manifest in different parts along the GI tract. Due to the chronic inflammation, strictures (narrowed intestinal passageways) are formed resulting in the most common symptom: abdominal cramps & pain. Although the cause of Crohn’s disease is unknown, there is an evident genetic predisposition. It is often seen in Px with biological relatives who suffer from some form of IBD, and there is a 13-18% increase in incidence in first degree relatives (Rendi, 2013). PATHOPHYSIOLOGY Risk factors Genetic NOD2 (nucleotide binding domain 2) Chromosomes 3,7,12, 16 (However less than 10% of people with mutations of these chromosomes or NOD2 develop the disease) (Rendi, 2013). Environmental Tobacco (smoking) Infective agents although bacteria trigger excessive inflammation, they are not the single causative agent. “The search for an infectious cause of inflammatory bowel disease continues, but it seems more likely that the ultimate cause is polyfactorial” (Rendi, 2013) PATHOPHYSIOLOGY Signs and Symptoms Abdominal pain/ cramping LRQ (Most common) Diarrhea Nausea & Vomiting Weight loss Fever Rectal bleeding Anemia (General fatigue) Dermal manifestation PATHOPHYSIOLOGY Complications of Crohn’s disease Intestinal blockage caused by the thickening of the intestinal wall due to swelling and scar tissue. Ulcers Fistulas (Tunnels in the affected area)– These can often become infected. Fissures Impaired nutrient absorption which results in protein, calories and vitamin deficiency. Risk factor for colon cancer. (National Digestive Diseases Information Clearinghouse (NDDIC), 2013) PATIENT CASE SCENARIO Primary Medical Diagnosis Crohn’s Disease HPI A forty-one year old woman presents to the ED with c/o abdominal pain and n/v since colonoscopy performed on 2/3/14 Reports pain as constant and 10/10 Patient reports taking oxycodone every 6 hours for pain relief at home Admitted to the ICU and scheduled for an exploratory laparotomy with possible drainage of an abdominal abscess and possible ileostomy Past Medical History Diagnosed with Crohn’s disease and Diverticulitis in 2012 History of ileostomy and ostomy reversal that has possibly reopened PATIENT CASE SCENARIO Assessment Febrile Severe abdominal pain-10/10 Watery stool in ileostomy bag Malnourished, weight of 78 lbs Complaints of n/v DIAGNOSIS (MDGuidelines, 2009) Colonoscopy: Provides view of the entire colon Tissue for biopsy and laboratory analysis The presence of granulomas (clusters of inflammatory cells) confirm the diagnosis because they only occur with Crohn’s disease CT Scan: Provides image of the whole bowel Allows the doctor to see the location and extent of the disease Also checks for complications like partial blockages, abscesses or fistulas MRI: Creates detailed images of organs and tissues Very useful in the diagnosis and management of the disease Capsule Endoscopy: Swallow a capsule that has a camera in it Takes pictures as it moves through the digestive tract The images are downloaded which can be checked for signs of Crohn’s disease (Mayo Clinic, 2011) TREATMENT OVERVIEW Medication Management (Mayo Clinic, 2011) Surgery (Chandra & Moore, 2011) Reduce inflammatory process that leads to exacerbation Long-term remission through limiting complications Symptom relief Correction of disease complications Restore individual’s health and function Nutrition (Richman & Rhodes, 2013) Diet low in animal fat30% of energy requirements Avoid foods that are high in insoluble fiber Avoid processed foods high in fat Include supplemental Vitamin D and dairy products if tolerated TREATMENT (MAYBERRY, LOBO, FORD, & THOMAS, 2013); (MAYO CLINIC, 2011) Using monotherapy to encourage remission: Corticosteroids Budesonide Useful in patients with a first presentation of the disease or a single inflammatory exacerbation in a 12-month period Less effective than traditional corticosteroids, but have fewer adverse effects 5-aminosalicylate (5-ASA) Less effective than the above drugs, but also with fewer adverse effects Not recommended for long-term use Effective for short-term treatment and to induce remission TREATMENT (MAYBERRY, LOBO, FORD, & THOMAS, 2013); (MAYO CLINIC, 2011) Immunosuppressant Drugs: azathioprine or mercaptopurine Suppress the immune system response which reduces the inflammatory process Most commonly used immunosuppressant's for the treatment of Crohn’s disease Combined with corticosteroid or budesonide therapy in patients that: Have two or more inflammatory exacerbations in a 12month period Cannot be tapered off the corticosteroid therapy TREATMENT (MAYBERRY, LOBO, FORD, & THOMAS, 2013); (MAYO CLINIC, 2011) Anti-Tumor Necrosis Factor-Alpha Therapy: Infliximab and adalimumab Neutralizes tumor necrosis factor-alpha in the bloodstream and prevents inflammation Treatment option for patients with severe Crohn’s disease Unresponsive to conventional therapy TREATMENT (CHANDRA & MOORE, 2011) Surgery may be indicated if: The disease is not responsive to medication therapy Treatment requires excessive steroid use Complications from medications arise Patients have difficulty with medication adherence SURGERY OPTIONS (CHANDRA & MOORE, 2011) Bowel Resection Preferred surgery Involves removing part of the diseased bowel Healthy ends may be reconnected, or a stoma may be created Strictureplasty Heineke-Mikulicz strictureplasty most commonly used For stricture sites <5 cm A longitudinal cut is made along the bowel which is then sewn together transversely Allows for the narrowed area of the bowel to be enlarged and prevents bowel obstruction PATIENT TREATMENT Not currently taking any maintenance medications Patient was admitted into the ICU and was prepped for an exploratory laparotomy Drainage of pelvic abscess Resection of terminal ileum Ileostomy with Hartman’s pouch Dissection of fistula Dietician reviewed patients chart and provided information for nutritional supplements NURSING DIAGNOSIS (NANDA) Alteration in nutrition: Less than body requirements R/T abdominal pain, nausea &vomiting, diarrhea, and decreased absorption of the intestines AEB patient’s weight of 78 Ibs. NCLEX QUESTION 1. The nurse is reviewing the record of a female client with Crohn’s disease. Which stool characteristics should the nurse expect to see documented in the client’s record? a. Diarrhea b. Chronic constipation c. Constipation alternating with diarrhea d. Stools constantly oozing form the rectum NCLEX ANSWER NCLEX QUESTION A) B) C) D) E) Which area of the alimentary canal is the most common location for Crohn’s disease? Ascending colon descending colon sigmoid colon, terminal ileum rectum REFERENCES Chandra, R., & Moore, J. W. E., (2011). The surgical options and management of intestinal Crohn’s disease. Indian Journal of Surgery, 73, 432-438. Mayberry, J. F., Lobo, A., Ford, A.C., & Thomas, A. (2012). NICE clinical guidelines (CG152): The management of Crohn’s disease in adults, children, and young people. Alimentary Pharmacology & Therapeutics, 37, 195-203. Mayo Clinic (2011, August 9). Diseases and conditions: Crohn’s disease. Retrieved from http://www.mayoclinic.org/diseases-conditions/crohns-disease/basics/definition/CON20032061 MDGuidelines (2009, April). Crohn’s disease. Retrieved from http://www.mdguidelines.com/crohns-disease National Digestive Diseases Information Clearinghouse (NDDIC) (2013, July). Retrieved 2014, from NIDDK: National Institute of Diabetes and Digestive and Kidney Diseases: http://digestive.niddk.nih.gov/ddISeases/pubs/crohns/#causes Rendi, M. M. (2013, July). Crohn disease pathology. Retrieved from Medscape: http://emedicine.medscape.com/article/1986158-overview Richman, E., & Rhodes, J. M. (2013). Review article: Evidence-based dietary advice for patients with inflammatory bowel disease. Alimentary Pharmacology & Therapeutics, 38, 11561171.