Crohn's case study
advertisement

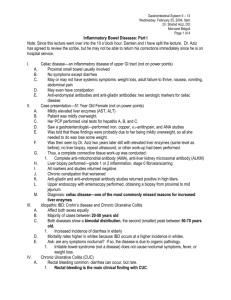
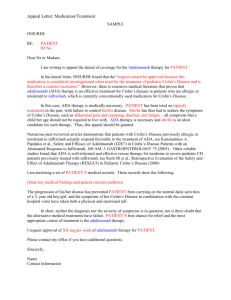
Crohn’s Disease A Case Study Isabella Bourke Jaymie McAllister Jessica Nemerovsky NUR 4216 Objectives • Student will be able to identify causative factors of Crohn’s Disease • Student will be able to explain the pathophysiology of Crohn’s Disease • Student will learn about the incidence and prevalence of Crohn’s Disease • Student will be able to identify an appropriate nursing diagnosis for a patient with Crohn’s Disease and possible nursing interventions What is Crohn’s Disease? • Genetically linked inflammatory disorder of GI tract classified as an inflammatory bowel disease (Alisa & Siew, 2011) • Involves all layers of intestinal wall • Characteristic skip lesions from intermittent patterns of inflammation • Affects any portion of the GI tract from mouth to anus • Causes are not definitively known – Combination of heredity, abnormal immune response, and imbalance of gastrointestinal flora Clinical Manifestations • Systemic S/S – Fever, fatigue, joint pain, mouth sores, fatty liver, autoimmune hepatitis • Diarrhea (Osborn, Wraa & Watson, 2009) – As many as 10-20 bowel movements per day • Weight loss • Abdominal pain – Right lower quadrant • Anemia • Malnutrition • Deficiency of fat-soluble vitamins Diagnostic Procedures • Endoscopy (Osborn, Wraa & Watson, 2009) – Gold standard • Radiography – Not favored due to risk of colonic perforation • Blood tests – Detect CBC r/t anemia • Stool sample – Checks for blood or infectious microbes • Barium enema • http://www.youtube.com/watch?feature=player_em bedded&v=yB-wm2x6woc#! Pathophysiology • Chronic inflammation from T-cell activation leading to tissue injury • Activation by antigen presentation results in unrestrained release of helper lymphocytes type 1 (Th1) • Defective regulation of Th1 cytokines such as interleukin (IL) 12 and tumor necrosis factor (TNF)-alpha stimulate the inflammatory response • Nonspecific inflammatory substances, like platelet activating factor and free radicals are released, resulting in direct injury to intestine (Medscape) • http://www.youtube.com/watch? v=obL6OB6My1Y Incidence & Prevalence • Men and women equally affected by IBD – Women, however, more likely to have Crohn’s Disease • Crohn’s disease affects every 133 people per 100,000 • Genetic link to Crohn’s Disease – Chromosome 10 – Chromosome 7 Patient Scenario • A 22 year old woman presents to the E.R. with a 6 week history of five loose, non-bloody stools daily, right lower quadrant abdomnial pain (especially after eating), a twenty pound weight loss, and bilateral knee and ankle pain. Findings from physical examination shows a definite and moderately tender 5 cm mass in the right lower quadrant of her abdomen. Stool culture are negative for enteric pathogens and blood work results show mild anemia (Hmg 11.2), with a normal metabolic panel and normal thyroid stimulating hormones. Radiographic findings show a 10cm narrowing of the terminal ileum and a separate of bowel loops around the terminal ileum. • This patient is then diagnosed with Crohn’s disease. The patient is started on 5-aminosalcylic acid (5ASA), antibiotics and nutritional therapy. Research • A gap between research exists when looking at antibiotic treatment for Crohn's disease patients. • A study by Feller, Huwiler, Schoepfer, Shang, Furrer, and Egger (2010) determined the effectiveness of long-term antibiotic treatment in 865 patients with Crohn’s disease. • This study suggested that “long-term treatment with nitroimidazoles or clofazimine appears to be effective in patients with Crohn’s disease.” • The current antibiotic treatment is Cipro and Flagyl. This study is level one and found that clofazimine and nitroimidazoles have been researched and are recommended for long-term antibiotic treatment. This is important because diarrhea is a very common and painful symptom in these patients. Antibiotics are known to cause diarrhea so it is imperative that we use these researched antibiotics to prevent this as much as possible. • • • • • • Treatment Modalities No current cure Diet therapy: – No specific diet is recommended other than a balanced regular diet and avoidance of triggers – High fiber can lessen diarrhea and improve rectal urgency Antibiotics – Flagyl – Cipro Anti-inflammatory drugs Immune system suppressors – Azathioprine – 6-mercaptopurine (6-MP) Aminosalicylate – Azulfidine • Decreases fever, pain, diarrhea and rectal bleeding Treatment Modalities Continued • Corticosteroids – used when traditional therapy does not work • Antidiarrheals • Laxatives • Pain relievers (tylenol) • Surgery – Can correct fistulas that may have formed – Anastomosis of affected portion of GI tract – Ostomy placement • ("Crohn's disease: Treatment," 2011) Elijah’s New Ostomy • http://www.youtube.com/watch?v=eBry_Msq cVs&feature=player_embedded Prognosis • Varies depending on the severity – Possible to have one episode in a lifetime while others suffer from chronic episodes • Rarely the direct cause of death, and many people live a normal lifespan • 3 out of 4 people with Crohn’s disease will end up needing surgical intervention (SIMON, 2008) ("Crohn's disease: Treatment," 2011) Nursing Diagnoses • Diarrhea related to inflammatory process (Ackley & Ladwig, 2011) • Acute pain related to increased peristalsis • Imbalanced nutrition related to diarrhea and altered ability to absorb and digest food • Risk for fluid volume deficit related to abnormal loss of fluid from diarrhea Nursing Interventions • • • • • • • • Assess defecation patterns. Assessment will help direct treatment If the diarrhea is related to IBS, interventions may include the use of complementary or alternative treatment such as probiotics. Probiotics enhance the normal intestinal microflora and decrease symptom of diarrhea Observe for signs and symptoms of sodium and electrolyte loss (weakness, abdominal or leg cramps, dysrthmias). Excessive diarrhea causes electrolyte abnormalities Monitor intake and output. Dark, concentrated urine is an indication of deficient fluid volume With chronic diarrhea, observe for signs and symptoms of malnutrition and consult with primary care provider for dietary consult and the possibility of supplemental feeding methods such as TPN. Provide a readily available bathroom, commode or bedpan at all times Ensure stringent perianal care for the patient daily and as needed using and a skin protectant (barrier cream)administral of antidiarrheal medications. At risk for perineal skin injury (Ackley & Ladwig, 2011) Conclusion • A definitive cure for Crohn’s disease does not currently exist • Treatment modalities depend upon the severity and the progression of the disease • Research is still being conducted to improve treatment modalities for Crohn’s disease • Inflammatory bowel diseases, including Crohn’s, contribute to a high incidence of colon cancers • These cancers are almost completely preventable with a proper diet that consists of bulk forming and low fat foods • With the exponential rise of obesity in America, it is important to promote awareness and teach preventative dietary methods. NCLEX Question #1 • The nurse is reviewing the record of a female client with Crohn’s disease. Which stool characteristics should the nurse expect to note documented in the client’s record? – A. Diarrhea – B. Chronic constipation – C. Constipation alternating with diarrhea – D. Stools constantly oozing from the rectum NCLEX Answer #1 • A! • Crohn’s disease is characterized by nonbloody diarrhea of usually not more than four to five stools daily. Over time, the diarrhea episodes increase in frequency, duration, and severity. Options B, C, and D are not characteristics of Crohn’s disease. NCLEX Question #2 • The nurse is preparing a client with Crohn’s disease for discharge. Which of the following statements indicates that he needs further teaching? – A. “Stress can make it worse.” – B. “Since I have Crohn’s disease, I am not likely to get colon cancer.” – C. “I realize I will always have to monitor my diet.” – D. “I understand there is a high incidence of familial occurrence with this disease.” NCLEX Answer #2 • B! • Persons with Crohn’s disease are at high risk for the development of colon cancer. The other options are all correct and do not indicate a need for further instruction References • • • • • • • • Ackley, B. J., & Ladwig, G. B. (2011). Nursing diagnosis handbook an evidence-based guide to planning care. (9th ed.). St. Louis,Missouri: Mosby Elsevier. Ailsa L., H., & Siew C., N. (n.d). Inflammatory bowel disease: Crohn’s disease. Medicine, 39(Gastroenterology Part 3 of 4), 229-236. doi:10.1016/j.mpmed.2011.01.004 Crohn's disease: Treatment and drugs. (2011, August 09). Retrieved from http://www.mayoclinic.com/health/crohns-disease/DS00104/DSECTION=treatments-and-drugs Feller, M., Huwiler, K., Schoepfer, A., Shang, A., Furrer, H., & Egger, M. (2010). Long-term antibiotic treatment for Crohn's disease: systematic review and meta-analysis of placebo-controlled trials. Clinical infectious diseases, 50(4), 473-480. Gastrointestinal diseases nclex review questions part 1. (n.d.). Retrieved from http://www.rnpedia.com/home/exams/nclex-exam/gastrointestinal-diseases-nclex-reviewquestions-part-1 Osborn, K. S., Wraa, C. E., & Watson, A. B. (2009).Medical-surgical nursing, preparation for practice. (Vol. 1). Prentice Hall. Simon, H. (2008, December 01). Crohn's disease: Prognosis. Retrieved from http://www.umm.edu/patiented/articles/who_gets_crohns_disease_000103_5.htm WebMD, LLC (2012). Medscape For Android (Version 2.2) [Mobile Application Software]. Retrieved from Google Play Store.