File
advertisement

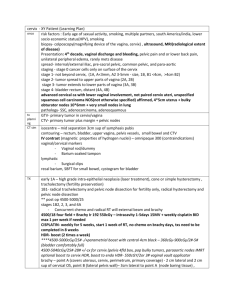
Genital prolapse Dr. Rupak Bhattarai Support to the Uterus Pubo-cervical ligament: The pubocervical ligament is a ligament connecting the side of the cervix to the pubic symphysis. Transverse ligament”) cervical(“cardinal Extend from cervix and lateral parts of the fornix to the lateral walls of pelvis ( ischial spine). Uterosacral ligament: Pass superiorly and slightly posteriorly from sides (base) of cervix to middle of sacrum; palpable during rectal exam Round ligament: attaches anteroinferiorly to uterotubal junction Broad ligament: These are 2 layered folds of peritoneum which suspend the uterus to the lateral pelvic wall It has anterior & posterior layers. A free upper border, lower, medial & lateral Superiorly the 2 layers are continuous over the uterine tube Inferiorly & laterally the 2 layers spread out to cover the pelvic floor Genital prolapseIt refers to the downward displacement of the uterus or vagina from its normal anatomical position. Etiology of prolapse These are usually seen during vaginal delivery with consequent injury to the supporting structures. 1.Premature bear down effort prior to the full dilatation of the cervix. 2.Application of the forceps or ventouse prior to the full dilatation of cervix. Precipitate labour. Early resumption of activites after delivery which increases intra abdominal pressure before they gain their normal tone. Repeated childbirth at frequent intervals. Increase in the intrabdomial pressure as in chronic cough and constipation. Clinical types 1.Vaginal prolapse: Anterior wall: A) Cystocele-is a medical condition that occurs when the tough fibrous wall between a woman's bladder and her vagina (the pubocervical fascia) is torn by childbirth, allowing the bladder to herniate into the vagina. Urethroceles often occur with cystoceles. Cystocele B) Urethrocele-is the prolapse of the female urethra into the vagina. Weakening of the tissues that hold the urethra in place cause it to move and to put pressure on the vagina, leading to the descent of the anterior distal wall of the vagina.Urethroceles often occur with cystoceles, (involving the bladder as well as the urethra).In this case, the term used is a cystourethrocele. Posterior wall: Rectocele:-results from a tear in the rectovaginal septum (which is normally a tough, fibrous, sheet-like divider between the rectum and vagina). Rectal tissue bulges through this tear and into the vagina as a hernia. There are two main causes of this tear: childbirth, and hysterectomy. Enterocele:-Laxity of the upper third of the posterior vaginal wall results in herniation in the pouch of douglas and contain omentum or even intestine. Uterine prolapse 1.First degree-The uterus descend down from the normal anatomical position (i.e external os at the level of the ischial spines) but external os still remains inside the vagina. 2.Second degree-The external os protudes outside the vaginal introitus but uterine body still inside. 3.Third degree (Procidentia ,complete prolapse)The uterine body descends to lie outside the introitus. Predisposing factors Congenital pelvic floor weakness Difficult or traumatic labour • Multiparity - trauma • Chronic disorders – chronic obstructive airway, constipations, straining • Abdominal tumours • Obesity, smoking, heavy lifting • Steroids, menopause, pelvic surgery Changes that may occur after prolapse Vaginal mucosa: The vaginal mucosa becomes stretched and if exposed to the air for long time becomes thickened and dry with surface keratinization. Decibutis ulcer: Trophic ulcer always found at the dependent part of the prolapsed mass lying outside the introitus There is initial surface keratinisation –cracksinfection-sloughing and ulceration. There is diminished circulation due to the constriction of the prolapsed mass by vaginal opening and narrowing of the vessels by the stretching effect. Cervix: The supravaginal portion of the cervix becomes Elongated due to the strain imposed by the pull. Obstruction to the urinary tract due to the huge cystocele which causes obstructive uropathy and leads to hypertrophy of the bladder walls. The kinking of distal ureter in procedentia leads to hydronephrosis and hydroureter. There may be infection of the bladder producing pyelitis or pyelonephritis. Incarceation: Infection of the paravaginal and cervical tissues makes the entire prolapsed mass odematous and congested and as a result the mass is irreducible. Peritonitis: The peritoneal infection may occur through the posterior vaginal wall. CLINICAL FEATURES Symptoms: Feeling of something coming out per vagina . Initially it is reducible but later it becomes irreducible. There may be variable discomfort that the mass comes out when she walks. Backache or dragging pain in the pelvis. Urinary symptoms like difficulty in passing urine,incomplete evacuation . If infection----- urgency ,frequency. Stress incontinence i.e while doing strenous work there is dribbling of urine. Bowel symptom in presence of rectocele like difficulty in passing stool and feeling of incomplete evacuation of the faeces. Excessive white or blood stained discharged per vaginum if there is associated vaginits or decibutis ulcer. Signs When you ask the patient to cough it raises the intra-abdomial pressure leading to: Bulge in anterior vaginal wall in case of cystocele. Bulging of the anterior and lower 1/3rd of vagina in case of cystourethocele, Bulging of the posterior vaginal wall in case o f rectocele and enterocele. Pinch Test: Cough impulse in uterine prolapse leads to the expulsion of the mass PV. In case of first degree prolapse examination is made by introducing speculum and one may see the cervical descent below the level of ischial spines. Treatment: Conservative: In case if first degree uterine prolapse pelvic floor exercise can be done. In case of 2nd or 3rd degree ring pessasary treatment can also be done if the patient doesn’t want have any operation. For Incarceation: For Ulcer: Surgical operation : Anterior colporaphy: Surgical procedure to correct cystocele and uretheocele. It involves making a cut in the front (anterior) wall of the vagina so the bladder and/or urethra can be pushed back into place. Once this is done, stitching together existing tissues to provide a new support for the bladder and urethra. Colpoperinorraphy: Surgical procedure to repair the prolapse of the posterior part of vaginal wall i.e rectocele and enterocele. The operation is done through the vagina. A cut is then made in the back (posterior) wall of the vagina and the rectum and/or small bowel is pushed back into place stitching together the existing tissues to create a new support for the prolapsed organ(s) and then removes some of the tissue from the vaginal wall to make it stronger. Pelvic floor repair(PFR): It includes the combination of anterior colporraphy or colpoperinorraphhy. Fothergills operation: To corect the uterine descent associated with cystocele and urethrocele with preservation of uterus is done. Vaginal hystrectomy with PFR.