Srdeční revoluce, srdeční akční potenciál, elektrická aktivita srdce
advertisement

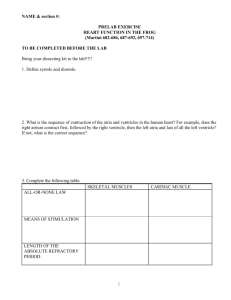
Heart revolution, cardiac action potential, cardiac electrical activity, ECG Romana Šlamberová, MD PhD Department of Normal, Pathological and Clinical Physiology Slides from the lecture. Respecting the copyrights it was not possible to publish pictures showed at the lecture at our website. Heart The heart is a hollow, muscular organ responsible for pumping blood through the blood vessels by repeated, rhythmic contractions. The heart is composed of cardiac muscle, an involuntary muscle tissue which is found only within this organ. Metabolism of cardiac muscle mostly depends on oxidative processes. Source of energy are fatty acids, lactate, glucose and sometimes aminoacids. Cardiac muscle Myocardium = syncytium – muscle cells are connected by plasmatic bridges. Cell nucleus is located in centrum of the cell (as in smooth muscles) and there is striated (as skeletal muscle). The thickness of heart cavities is different (the thickest is in left ventricle). Except muscle fibers that have as a main function contraction, myocardium has also muscle tissue that is specialized in production and spread of excitation = conducting system of the heart. Basic characteristic of myocardium Chronotrophy = ability of myocardium to produce impulse (excitation). Result = regular rhythmic muscle contractions without external impulse. Dromotrophy = impulse transfers to the entire muscular unit (atriums and ventricles), providing synchronous contraction of all muscle fibers. Bathmotrophy = ability to induce muscle contraction that is strong enough (supraliminal input). While input that is lower than threshold does not induce contraction, supraliminals input of different intensity induces the same response if it comes in sensitive period. Inotrophy = ability of muscle contraction and its dependency on other factors, e.g. initial tension of muscle fiber. Blood circulation Blood circulation are two separated circuits = Small (pulmonary) circulation is powered by right heart ventricle and large (systemic) circulation by left ventricle. Volume of blood pumped in time unit to pulmonary and systemic circulation is the same = Minute heart volume Heart distribution is given by amount of systolic pulse volume (volume of blood ejected by one heart contraction) and by heart rate frequency. Pulmonary and systemic circulation differs in their pressure and resistence. Pressure in pulmonary circulation is about 4 – 5 times lower than in systemic one. Heart works as pressure pump. It has two parts: static component - breaks through the pressure gradient between ventricle and artery, and kinetic component – induces acceleration to ejected amount of blood. Heart cycle Tension – isovolumic phase. At the beginning of systole the intraventricular pressure increases and atrioventricular valves close (systolic sound). Ejection phase. Intraventricular pressure exceeds the pressure in large arteries and the ejection of blood from ventricles begins (systolic pressure in arteries). Ejection phase ends when the intraventricular pressure decreases to a level a little bit lover than the pressure in large arteries. Blood flow turns around and semilunar valves close (diastolic sound). Phase of isovolumic relaxation. Intraventricular pressure decreases. Filling phase. The pressure in ventricles decrease so that it is lower than the pressure in atria and the atrioventricular valves open. At the beginning – phase of fast filling, later phase of slow filling. Systole of atriums = last phase of ventricle diastole. Pressures and volumes • Pulse (systolic) volume (PV)= 70 ml • Final diastolic volume (FDV)= 120 ml • Final systolic volume = 50 ml = functional reserve of heart • Normal systole ejects around 60% of FDV = Ejection phase = PV/FDV. • Heart distribution = PV x frequency Rokyta: Fyziologie Conducting system of heart (1) The entire heart muscle is able to produce impulses and to induce contraction = Automacy. Myocardium of ventricles and atria use the automacy function in pathological cases. There is a system of heart tissue in the heart that differs from myocardium of atria and ventricles. It specializes to production and spread of impulses that induce contraction of heart muscle. Structure of cells of conducting system differs from cell of myocardium in lower number of myofibres, high amount of glycogen and especially electro-physiologist characteristic. Nodal part of conducting system (sinoatrial node and atrioventricular node), has low speed (0.02-0.1 m/s) of impulse spread, but high ability of automacy. Other parts of the conducting system have ability of high speed of impulse spread – depolarisation wave (4 m/s). Conducting system of heart (2) Sinoatrial node (Keith-Flack) = pacemaker – located in entrance of right atrium (sinusoidal rhythm 60 – 80/min). If the SA node doesn't function, or the impulse generated in the SA node is blocked before it travels down the electrical conduction system, a group of cells further down the heart will become the heart's pacemaker. Internodal tracks – connect SA node with AV node (The AV node receives two inputs from the atria: posteriorly via the crista terminalis, and anteriorly via the interatrial septum) Atrioventricular node (Aschoff-Tawar) – located by base of tricuspidal valve (nodal rhythm 30 – 40/min). Time needed for impulse transfer through AV node is 130 ms. Unique for AV node is decremental conduction = property of the AV node that prevents rapid conduction to the ventricle in cases of rapid atrial rhythms, such as atrial fibrillation or atrial flutter. The atrioventricular node delays impulses for 0.1 second before spreading to the ventricle walls. Importance = to ensure that the atria are empty completely before the ventricles contract. Conducting system of heart (3) Bundle of His = a collection of heart muscle cells specialized for electrical conduction that transmits the electrical impulses from the AV node (located between the atria and the ventricles) to the point of the apex of the fascicular branches. (the only conducting connection between atriums and ventricles) Right and left (anterior and posterior) bundle branches (Tawar branches) – going to myocardium of ventricles. Purkynje fibers – going to periphery and end in myocytes of ventricles. Together, the bundle branches and Purkinje network comprise the ventricular conduction system. It takes about 0.03-0.04s for the impulse to travel from the bundle of His to the ventricular muscle. Conducting system of heart (4) Impulse spreads: • from endocardium to epicardium • from apex to base • Synchronous activation of myocardium – systole of ventricles. Conducting system of heart (5) • Fibers of SA node are easy permeable for Na+, that enter the cells and decrease their resting membrane potential (only –55 to –65 mV). • This process of decreased polarisation ends when it reaches level of –40 mV – prepotential (spontanous depolarisation). • At this level the sodium-calcium channels opens and action potential is produced. • During action potential the K+ channels are closed and again open during repolarisation. Action potential SA node Myocardium Myocardium – contraction Contraction – begins just after the start of depolarization and lasts about 1.5 x longer than the action potential Absolute refractory period – cardiac muscle cannot be excited again = therefore tetanus (as in the skeletal muscle) cannot accur Shortly after the end of repolarisation myocardium response only to strong impulse and the power of contraction is lower even during high intensity of stimulation. This period is called relative refractory period. Vulnerable period = period at the end of the action potential during which the fibrilation of the heart may accur. Myocardium – correlation length x tension Frank-Starling’s law = initial length of the fibers is determined by the degree of diastolic filling of the heart, and the pressure developed in the ventricle is proportionate to the total tension developed. The developed tension increases as the diastolic volume increases until it reaches a maximum, then tends to decrease. Ganong: Review of Medical Physiology Electric expression of heart action Ganong: Physiology Record of summary electric activity of hear is called electrocardiogram (ECG). ECG curve is summary potential that is a result of all action potentials of myofibers. Beginnings of QRS complex and action potentials of ventricles are the same and ending of ventricle action potentials is the same as the end of wave T. History ECG Description of animal electricity by Luigie Galvani (1783) and discovery of galvanometer by Hans Oerstad (1819) started the period of experimental electrophysiology. Electric changes dependent on heart action described as first Italian physicist Carlo Matteuci (1842) by using frogs. The term electrocardiogram used as first British physiologist Augustus D. Waller, it came to our subconscious mind by attempt of Dutch physiologist Willem Einthoven (1893). Einthoven constructed fiber galvanometer (1901, Nobel price 1925) that showed the same curve as ECG. He described the PQRST curve. At year 1906 he published atlas of normal and abnormal ECGs, in which he described left and right hypertrophy of ventricles and atriums, wave U (repolarisation of Purkynje fibers), flutter of atriums etc. ECG Limb leads: V1-V2 = right ventricle V3-V6 = left ventricle Eithoven’s leads I., II, III. V1 – 4th intercostal, right parasternal V2 – 4th intercostal, left parasternal V3 – between V2 and V4 V4 – 5th intercostal medioclavicular V5 – between V4 and V6 V6 – 5th intercostal, anterior axial Goldberg’s leads aVL, aVR, aVF V8 – 5 intercostal, scapular V9 – 5th intercostal, paravertebral Bipolar limb leads (measure changes in potential between two electrodes) Red – right arm Yellow – left arm Green – left leg Black – right leg (grounding) Thoracic leads (Wilson’s) Unipolar limb leads it is possible to use also (measure changes in potential Nehb’s leads between electrode and V7 – 5th intercosta, posterior axial Wilson’s clamp) th Leads and electrodes Limb Thoracic Trojan: Fyziologie Evaluation of the ECG Pulse: regular, irregular Rhythm: sinusoidal or other (nodal = from AV node) Frequency: Normal 60-90 pulses/min Heart electrical axis inclination: normal (the same way), to left (outside), to right (inside) just generally from limb leads I and III. Exactly by using Einthoven’s triangle. Description of waves, their duration and intervals. Frequency Heard frequency = 72 pulses/min, = pulse interval 0.83 s During relaxation the frequency changes based of the respiration (RESPIRATION ARYTMIA) = inspiration - increased frequency, expiration – decreased frequency. Bradycardia = fysiological = deep long-term inspiration, deep forward bend and knee band = reflex changes of vagal tonus. Tachycardia = fysiological = swallow (decrease of vagal tonus), change of position from lying or sitting to standing (ORTOSTATIC REACTION). Description of curves P = Impulse spread through atria PQ = neutral (isoelectric) line after depolarisation of all atria myocardium QRST = ventricle complex Q = negative oscillation – beginning of ventricle depolarisation in septum R = continue of depolarisation wave through the ventricle S = negative oscillation – activation of last part of ventricle myocardium in left ventricle base ST = neutral (isoelectric) line after ventricle depolarisation (plató phase in action potential) T = repolarisation from epicardium to endocardium Examples of pathological ECG Sinusoidal rhythm and fibrilation of atria & AV block Fibrilation of ventricles Heart attack Electric expression of heart action Ganong: Physiology Record of summary electric activity of hear is called electrocardiogram (ECG). ECG curve is summary potential that is a result of all action potentials of myofibers. Beginnings of QRS complex and action potentials of ventricles are the same and ending of ventricle action potentials is the same as the end of wave T. heart electrical axis average (largest) electrical heart vector) if positive in the lead aVF (←) and positive in the lead I (→) then must lie where overlap Heart electrical axis inclination Each myocyte produce dipole during action potential - vector with specific dimension and direction. Cell vector head from depolarised to polarised part, i.e. in direction of action potential spread. If the cell is completely depolarised (plató phase) or polarised (resting phase), vector is neutral. Electrical heart vector is a summary of all cell’s vectors in one time point Normal value is -30° až +105° Shift of the axis to right above 105 ° = hypertrophy of RV or long and slim Shift of the axis to left below -30° = hypertrophy of LV or obese people Examination of the heart Mitral valve (bicuspidal) – 5th intercostal space in mediclavicular line (apex) Tricuspidal valve – 5th intercostal space right parasternal line Semilunar valve of aorta – 2nd to 3rd intercostal space righ parasternal line Semilunar valve of pulmonary artery – 2nd to 3rd intercostal space left parasternal line