Cardiac Arrhythmia
advertisement
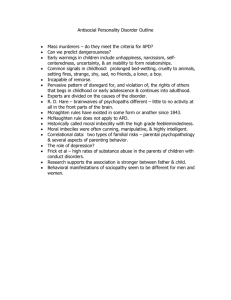
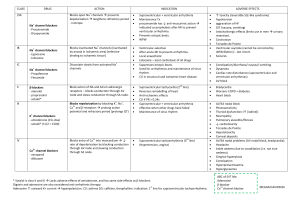
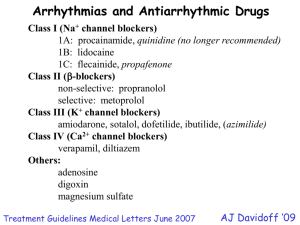
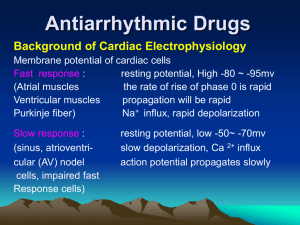
Cardiac Arrhythmias Types of cardiac arrhythmias: •Bradyarrhythmias •Tachyarrhythmias •Bradyarrhythmias: treat with atropine, pacing •Tachyarrhythmias can occur due to: Enhanced automaticity Afterdepolarization and triggered activity Re-entry Tachyarrhythmias: •Enhanced automaticity: In tissues undergoing spontaneous depolarization -stimulation, hypokalemia, mechanical stretch of cardiac muscle Automatic behaviour in tissues that normally lack spontaneous pacemaker activity e.g. ventricular ischaemia depolarizes ventricular cells and can cause abnormal rhythm •Afterdepolarization: EAD: when APD is markedly prolonged Occur in phase 3 May be due to inwards Na+ or Ca2+ current Excessive prolongation of APD- torsades de pointes syndrome EAD DAD Torsades de pointes: polymorphic ventricular tachycardia along with prolonged QT interval DAD: precipitating conditions are intracellular or sarcoplasmic Ca2+ overload, adrenergic stress, digitalis intoxication, heart failure If afterdepolarizations reach a threshold, an AP is genererated which is called ‘triggered beat’ DAD occur when the HR is fast, EAD occur when the HR is slow •Re-entry: when a cardiac impulse travels in a path such as to return to and reactivate its original site and self perpetuate rapid reactivation independent of normal sinus node conduction Requirements for re-entry rhythm: slowing or conduction failure due to either an anatomic or functional barrier Anatomic barrier- Wolff-Parkinson-White syndrome Functional barrier- ischaemia, differences in refractoriness Presence of an anatomically defined circuit Heterogenecity in refractoriness among regions in the circuit Slow conduction in one part of the circuit •What are channels? – they are macromolecular complexes consisting of a pore forming subunit, subunits and accessory proteins •They are: Transmembrane proteins Consist of a voltage sensitive domain A selectivity filter A conducting pore and, An inactivating particle •In response to changes in membrane voltage, the channel changes conformation so as to allow or prevent the flow of ions through it along their concentration gradient K+ (Transient) K+ (delayed rectifier) Ca2+ Na+ Ca2+ Na+ Na+K+ATPase K+ K+ channel blocker -blocker, CCB Na+ channel blocker Ca2+ channel blocker & -blocker How can drugs slow the cardiac rhythm? Decreasing phase 4 slope Increase in threshold potential for excitation Increase in maximum diastolic potential Increase in APD •Fast response tissues •Slow response tissues Na+ channel blocker: •Na+ channel block depends on: HR Membrane potential Drug specific physiochemical characteristic- recovery •Blockade of Na+ channels results in: Threshold for excitability is increased (more current) Increase in pacing and defibrillation threshold Decrease conduction velocity in fast response tissues Increase QRS interval Some drugs tend to prolong PR interval- flecainide (possibly Ca2+ channel blockade) •Some sodium channel blockers shorten the PR interval (quinidine; vagolytic effect) •APD unaffected or shortened •Increase in threshold for excitation also decreases automaticity •Can also inhibit DAD/EAD •Delays conduction so can block re-entry •In some cases, it can exacerbate re-entry by delaying conduction •Shift voltage dependence of recovery of sodium channels from inactivated state to more negative potentials and so increases refractoriness •Net effect- whether it will suppress or exacerbate re-entry arrhythmia depends on its effect on both factors- conduction velocity and refractoriness •Most Na+ channel blockers bind to either open or inactivated state and have very little affinity for channels in closed state, drug binds to channels during systole & dissociates during diastole •ADRs: Decrease in conduction rate in atrial flutter- slows rate of flutter and increases HR due to decrease in AV blockade Especially common with quinidine due to its vagolytic property; also seen with flecainide and propafenone Cases of ventricular tachycardia due to re-entrant rhythm following MI may worsen due to slowing of conduction rate Slowing of conduction allows the re-entrant rhythm to persist within the circuit so that complicated arrhythmias can occur Several Na+ channel blockers have been reported to exacerbate neuromuscular paralysis by d-tubocurarine •K+ Channel blockers: Prolong APD (QT interval) and reduces automaticity Increase in APD also increases refractoriness Effective in treating re-entrant arrhythmias Reduce energy requirement for defibrillation Inhibit ventricular arrhythmias in cases of myocardial ischemia Many K+ channel blockers also have blocking activity also like sotalol Disproportionate prolongation of APD can result in torsaides de pointes, specially when basal HR is slow •CCBs: Major effect on nodal tissues Verapamil, diltiazem and bepridil cause slowing of HR, nifedipine and other dihydropyridines reflexly increase HR Decrease AV nodal conduction so PR interval increases AV nodal block occurs due to decremental conduction and increase in AV nodal refractoriness DAD leading to ventricular tachycardia respond to verapamil Verapamil and diltiazem are recommended for treatment of PSVT Bepridil increases APD in many tissues and can exert antiarrhythmic action in atria and ventricles but it use is associated with increased incidence of torsades de pointes- rarely used

![Applied Heat Transfer [Opens in New Window]](http://s3.studylib.net/store/data/008526779_1-b12564ed87263f3384d65f395321d919-300x300.png)