CHAPTER 25
advertisement

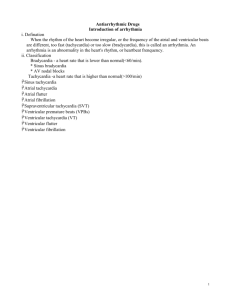
CHAPTER 25 ANTIARRHYTHMIC DRUGS 1 2 Arrhythmia: Arrhythmias consist of cardiac depolarizations that deviate from the sinus rhythm--ie, There is an abnormality in the site of origin of the impulse, its rate or regularity , or its conduction . 3 The types of Arrhythmia: 缓慢型 : 窦性心动过缓 (sinus bradycardia) 房室传导阻滞 (atrio-ventricular block) 快速型 : 房性早搏 (atrial premature contraction) 房性心动过速 (atrial tachycardia,AT) 心房颤动 (atrial fibrillation, AF) 心房扑动 (atrial flutter, AFL) 阵发性室上性心动过速 (paroxysmal supraventricular tachycardia) 室 性 早 搏 (ventricular premature contraction) 室性心动过速 (ventricular tachycardia,VT) 心室颤动 (ventricular fibrillation, VF) 4 Section 1 The Physiological Basis of Arrhythmia 1. The electrophysiology of normal cardiac rhythm 5 6 7 2. The electrophysiological mechanism of arrhythmias (1) Disturbances in impulse formation: Increased automaticity (2) Afterdepolarization and triggered activity: Early afterdepolarization (EAD) Delayed afterdepolarization (DAD) 8 9 (3) Disturbances in impulse conduction 1) Simple conduction disturbances: conduction ↓ conduction block 2) Reentry (circus movement) 10 11 Section 2 The Basic Electrophysiology Action of Antiarrhythmic Drugs and The Classification of Drugs 12 1. The basic electrophysiology action 1)↓automaticity (autorhythmicity) a.↓slope of phase 4 depolarization: ↓Na+in or Ca2+in b.↑Threshold potential c.↑maximum diastolic potential: ↑K+out + ↑APD ↓ K D. out 13 14 15 16 17 2)↓EAD or DAD: Accelerate repolarization, Block Na+ in or Ca2+ in 3) Avoid reentry: a.↑conduction:↓unidirectional block b.↓conduction : unidirectional block → bidirectional block c.↑ERP 18 2.The classification Class by Vaughan Williams (1971) ClassⅠ Sodium channel-blocking agents: IA , IB, IC ClassⅡ β-R blockers Class Ⅲ Prolonging APD agents Class Ⅳ Calcium channel blockers Sicilian gambit (1991) 19 Section 3 Specific Antiarrhythmic Agents 1. ClassⅠ Sodium channelblocking agents 20 钠通道阻滞剂的分类 分类 药物 钠阻滞强度 结合/解离常数 心电图表现 状态依赖 IA IB 奎尼丁 普鲁卡因胺 ++ 1—10秒 延长QT 激活态 利多卡因 美西律 + <1秒 不明显 失活态 IC 普罗帕酮 氟卡尼 +++ >10秒 QRS增宽 激活态 21 1) ClassⅠA a. Inhibit Na+ influx moderately : ↓Vmax, ↓conduction ↓phase 4 slope, ↓automaticity b. ↓ K+ efflux , Increase the ERP 22 Quinidine(奎尼丁) Pharmacological Effects: Cardiac Effects: ↓autorhythmicity;↓conduction;↑ERP ↓myocardial contractility Extracardiac Effects: α-adrenergic blocking anticholinergic effect 23 Therapeutic Uses: Broad-spectrum Atrial fibrillation; Atrial flutter; Supraventricular and ventricular tachycardia; Supraventricular and ventricular premature beat 24 Toxicity: CVS: Heart failure; hypotension; quinidine syncopy Chichonic reaction(金鸡纳反应) 25 2) Class IB ↓Na+ influx lightly ↑K+ efflux, shorten the APD>ERP , ERP/APD ↑ 26 Lidocaine (利多卡因) Pharmacological effects: Act on Purkinje fibers and ventricular cells a. ↓autorhythmicity ↓the slope of phase 4 and ↑the threshold for excitability. 27 b. Altering the conduction: Myocardial ischemia →↓conduction, unidirectional block→bidirectional block K+↓→↑K+ efflux →↑conduction → ↓unidirectional block c. Relative increase ERP: ERP/APD↑ Pharmacokinetics: Therapeutic use: Ventricular arrhythmias 28 Phenytoin sodium It has been used in the acute and chronic ventricular arrhythmias, especially in digitalis intoxication. 29 3) Class IC Severely depress Na+ influx, markedly↓Vmax , ↓conduction. ↓phase 4 slope. ↓automaticity Serious adverse reactions are provocation of potentially lethal arrhythmias. 30 CAST试验I(心律失常抑制试验) 心律失常抑制标准:室早减少80%以上,室速 减少90%以上。 入选病人2309例。结果可见1727例心律失常抑制 良好;135例部分抑制;447例室性心律失常增加,治 疗组死亡率7.3%,安慰剂组死亡率3.0%。其中心律失 常或心跳骤停者治疗组4.5%,安慰剂组1.7%。 结果说明英卡尼和氟卡尼虽能较好的抑制MI后 的心律失常,但明显增加所致死亡率及总病死率,其 原因为该类药物有负性肌力作用,另外其致心律失常 作用亦不容忽视。 31 Propafenone(普罗帕酮) Block Na+and Ca+ channel, also blockβ-R ↓conduction, ↓automaticity, ↑ERP Used to treat Supraventricular and ventricular tachycardia; Supraventricular and ventricular premature beat, Atrial fibrillation. 32 Class Ⅱ β-R Blockers Propranolol Metoprolol Atenolol 1) β-R blocking action 2) Membrane-stabilizing effect(↓Na+in) 33 Pharmacological effects: a.↓autorhythmicity,↓afterdepolarization by CA, prevent triggered activity. b.↓ conduction of AV node and P-f ( >100ng/ml) c.↑ERP of AV node,↓reentry d. Improve myocardial ischemic Therapeutic uses Supraventricular arrhythmias Acute myocardial infarction(AMI) 34 BHAT(急性心肌梗死后普萘洛尔对室 性心律失常的影响) 美国,加拿大37个临床中心采用多中心,随机 安慰剂双盲对照试验。入选标准: AMI后5-21天经 ECG检查发现频发室性早搏,短阵室速,共入选 3837例。 药物用法为第一天普萘洛尔20mg或安慰剂, 如无副作用第二天用40mg,每日三次,之后逐渐 增加到80mg,每日三次,最长随访时间36个月。 结果可见6周后安慰剂组心律失常减少 1.6%,治疗组减少15.4%,安慰剂组死亡率9.8%, 治疗组7.2%(P<0.005)。研究结果说明普萘洛尔 用于AMI可明显降低死亡率,并可长期应用,安全 有效。 35 Class Ⅲ Prolonging APD agents Blocking K+ channel , ↓ K+ efflux , ↑ repolarization, ↑ APD and ERP 36 Amiodarone(胺碘酮) Pharmacological effects: ↓ions channel: K+, Na+, Ca2+ Blocking α,βreceptor 1) ↑APD and ERP, no reverse use-dependence 2) ↓autorhythmicity 3) ↓ conduction of AV node and Purkinje fibers 4) Dilatation coronary artery, ↓ myocardial oxygen consumption 37 Pharmacokinetics: F: 40%, t1/2 40 d, last 4~6 w Therapeutic uses: Broad-spectrum antiarrhythmic drug 38 Adverse effects: CVS reactions: Sinus bradycardia Atrio-ventricular block Torsades de pointes(Tdp, long QT syndrome, LQTS) Pulmonary fibrosis Hypo- or hyperthyroidism 39 BASIS(巴塞尔心肌梗死后心律失常研究); CASCADE (西雅图胺碘酮和其他抗心律失常药物 对心脏骤停作用的评价);CAMIAT (加拿大心肌 梗死后胺碘酮抗心律失常试验);EMIAT (欧洲 心肌梗死后胺碘酮试验);IAMT (静脉内胺碘酮 抗心律失常研究)。 入选病人多数为AMI后室性心律失常患者,服 药方法为:第一周每天800mg,第二周每天400mg 用6天,持续12个月,有显著心动过缓,QT间期明 显延长者剂量减少至100mg/日。 结果显示:胺碘酮组心脏性死亡率明显减少 (P=0.048),严重室性心律失常的发生率胺碘酮 组7.5%,对照组19.5%(P< 0.001) 40 Sotalol (索他洛尔) Nonselective β-R antagonist Block Ik, ↑APD、ERP F=90%~100% Broad-spectrum 41 Dofetilide(多非利特) 阻滞Ikr,延长不应期但不减慢传导,无负 性肌力和负性血流动力学效应,用于房颤复律和 维持窦律,有效且不增加心衰死亡率,左室功能 重度障碍者可用。 具有reverse use-dependence, 主要 副作用为Tdp(2%~4%)应监测QTc变化。 Ibutilide (伊波利特) Sematilide (司美利特) 42 Ikur只分布于心房肌,在调控心房复极 中起重要作用 ,而对心室肌无影响,开发 选择性Ikur阻滞剂用于治疗房性心律失常, 是III类药物开发方向之一。胺碘酮、氨巴 利特(ambasilide)对Ikur有阻滞作用。 43 Class Ⅳ Calcium channel blocking agents Block the L-Ca2+ channel of cardiac,↓sinus and AV node. 44 Verapamil(维拉帕米) Major clinical uses: Supraventricular arrhythamias. 45 Others Adenosine(腺苷) Act on A-R, ↑KACh ,↑K+ efflux ↓cAMP-induced Ca2+ influx, ↑ERP of AV node. Choice for prompt conversion of paroxysmal supraventricular tachycardia. 46 抗心律失常药的合理应用 用药原则 1. 先单用药,后联合用药。 2. 小剂量, 个体化用药, 。 3. 充分注意药物的不良反应, 特别是致心律失常作用。 47 药物的致心律失常作用 The proarrhythmia action of drugs 应用抗心律失常药物过程中,原有心 律失常加重或恶化,或出现新的心律失常。 发生率:6%~30% 所有抗心律失常药物都有引起折返性 心动过速的基础,因此是双刃剑。 防治:明确指征,纠正诱因,抗心律 失常( β阻断药、胺碘酮) 48 The Choice of Drug Therapies 1. Sinusal tachycardia: β- Blockers or Verapamil 2. Atrial premature beat: β- Blockers , Verapamil 3. Atrial fibrillation, Atrial flutter: Verapamil, β- Blockers , Amiodarone, Cardiac glycosides, 4. Supraventricular tachycardia: Verapamil, Cardiac glycosides, β- blockers, Adenosine. 49 5. Ventricular premature beat: Lidocaine, Amiodarone ,Propafeone 6. Ventricular tachycardia: Lidocaine, Amiodarone, Propafeone 7. Ventricular fibrillation: Lidocaine, Amiodarone. 50 抗心律失常药物作用最佳靶点假说 在心肌细胞膜上存在多种离子通道及亚型。 正常情况下,各通道间有一定数目和比例,保 持一定的平衡。当某种通道数目上调或下调到 一定范围,通道间比例失调,将出现心律失常。 与心律失常发生发展有关的通道,称为抗心律 失常药作用的靶点。在心律失常发生发展中起 主导作用的通道,称为抗心律失常药作用的最 佳靶点。一个理想的抗心律失常药应对最佳靶 点有作用,且至少对两种或两种以上的离子通 道有作用。 51