BMW25: Myelodysplastic/Myeloproliferative Neoplasm with
advertisement
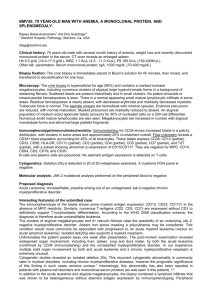
BMW25: MYELODYSPLASTIC/MYELOPROLIFERATIVE NEOPLASM WITH ACTIVATING CBL MUTATION Annette Schmitt-Graeff , Juliana Popa , Torsten Haferlach and Andreas Reiter 1.Universityhospital Freiburg, Pathology, Freiburg, Germany 2.Universitätsmedizin Mannheim, III. Medizinische Klinik, Mannheim, Germany 3.MLL Munich, Leukemia laboratory, München, Germany 1 2 3 2 annette.schmitt-graeff@uniklinik-freiburg.de Clinical History: This 68-year-old female patient initially presented with anemia, leukocytosis and mild thrombocythopenia. The WBC was 45.1 x 109/L , the hemoglobin 10.2g/dL, the platelets 113 x109/L and the LDH 286 U/L.The peripheral blood smears showed 1% promyelocytes, 2% myelocytes, 2% metamyelocytes, 32% band forms, 52% granulocytes, 2% monocytes and 9% lymphocytes. The neutrophils showed atypical features including cytoplasmic hypogranularity, bizarrely segmented nuclei and pseudo-Pelger forms. Since no BCR-ABL1 fusion gene mutation was detected, the findings were suggestive of an atypical chronic myeloid leukaemia (aCML) and treatment with hydroxyurea was started. Two years later, the patient was admitted to the hospital with increasing splenomegaly and thrombocytopenia. Hb 9,7.2g/dL, WBC 87.8 x 109/L, Plt 14 x 109/L. Other lab. parameters: LDH 495 U/L. Biopsy fixation: Fixative: 30 ml formaldehyde 30%, 20 ml glutardialdehyde 25%, 15,8g calciumacetate, aqua dest ad 1000 ml; decalcification in EDTA. Microscopy: The trephine bone marrow biopsy obtained at initial presentation was hypercellular with a striking increase in a left shifted atypical myelopoiesis with <5% blasts. Both erythropoiesis and megakarypoiesis were diminished. Dysplastic micromegakaryocytes were loosely distributed without without a tendency to form clusters. The reticulin meshwork was not significantly increased. In the sequential biopsy which is submitted to the workshop, immature myeloid cells with nuclear features of blasts represent >70% of nucleated bone marrow cells. Small groups of erythroid cells and rare dysplastic megakaryocytic microforms were highlighted by anti-hemoglobin and CD61 immunohistochemistry. Smear: The differential count at this time was: 21% blasts, 14% promyelocytes, 25 metamyelocytes, 1% band forms, 4% segmented granulocytes, 2% eosinophils, 6% monocytes, 26% lymphocytes and 3% normoblasts. Immunophenotype/immunohistochemistry: By flow cytometry, the blast cells expressed MPO (44%), CD13 (76%) and CD33 (84). Two leukaemia-associated phenotypes were detected: CD64+CD87+CD4+CD56+CD45+; and CD34, CD56+CD19-CD33+CD45(+). Immunohistochemistry showed a strong immunolabelling for myeloeroxidase and CD33 by abundant immature myeloid precursors which were also positive for naphtol AS-D chloroacetatesterase. Cytogenetics: The karyotype was 47,XX,+8 [5]; 46,XX [17]. Molecular analysis: FISH analysis confirmed a trisomy 8. ISCN IP-FISH: nuc ish 8cen (D8Z2x3) [7]; nuc ish 8cen (D8Z2x2) [93]; No BCR-ABL1-, JAK2-V617F-, FLT3, NPM1- or MLL-mutations were present. However, additional molecular studies revealed an activating CBL mutation (C384R) which was also detected in samples obtained at the initial presentation. Proposed diagnosis Atypical CML harbouring a CBL mutation transforming into an acute myeloid leukaemia. Interesting feature(s) of the submitted case Acquired uniparental disomy leads to loss of heterozygosity with loss-of-function mutations of tumor suppressor genes in tumor cells, but may also be associated with a gain-of- function mutation of protooncogenes. The C-CBL proto-oncogene negatively regulates the signal transduction of tyrosin kinases. It has recently been shown that acquired transforming CBL mutations are a key event in the pathogenesis of a rare subset of myeloid malignancies most often presenting with a myelomonocytic phenotype. Our observation provides evidence that the pathogenesis of atypical CML which remains until now a clinically assigned myelodysplastic/myeloproliferative neoplasm, may also be associated with an acquired activating CBL mutation. Other comments: The patient was treated according to an AML therapy protocol but failed to respond adequately and died of progressive disease. The rapid clinical progression and the failure to respond to conventional AML therapy that was observed in our patient confirm the aggressiveness of the CBL mutated subsets of MDS/MPNs.