Vascular Ultrasound and Wound Care
advertisement

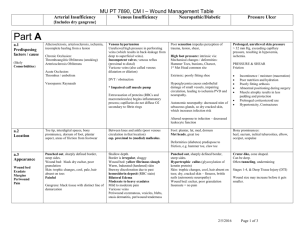
Lower Extremity Wounds: The role of the vascular technologist Jesse Thomas, RVT UNC Health Care DISCLOSURES NO RELEVANT CONFLICTS OF INTEREST TO DECLARE Objectives • Review types of wounds • Discuss risk factors • Role of Duplex Imaging • Role as a Technologist • This presentation will NOT address the use of ultrasound as a wound management and/or treatment tool. Types of Wounds • Arterial • Venous • Neuropathic • Small vessel/Vasculitis • Pressure ulcers Arterial • Ischemic wounds • Result of inadequate blood supply • Tissue hypoxia and tissue damage • Most commonly result of atherosclerotic disease (PAD) PAD • Narrowing of arteries to the limbs that reduces blood flow • More common in LE • Atherosclerosis – build up of fatty deposits (plaque) Arterial • Risk Factors • High cholesterol • Aging • HTN • Diabetes • Smoking • Family hx of cardiovascular disease • Obesity PAD • Approximately 8 million people in the US • 12-20% in those >60 • Public awareness around 25% • Associated with significant morbidity and mortality Source: National Center for Chronic Disease Prevention and Health Promotion PAD • May present with variety of signs/symptoms • Claudication – to limp • Aching, cramping pain brought on by exercise and relieved with rest • Calf, thigh, hips or buttocks PAD • Rest pain • Non-healing ulceration • gangrene Arterial Ulcers • Characteristics • “punched out” appearance • Smooth wound edges • Surrounding skin may exhibit dusky erythema • Cool to touch • Hairless, thin, brittle with shiny texture Arterial Ulcers • Typically lower leg • Lateral foot • Toes • Pressure points or where injury has occurred Arterial Ulcers • Jesse, why do I care what these look like and are you done showing these nasty pictures? Role of Sonographer • Patient history • Physical exam • ABI’s • Clues to what is going on before you put the transducer on the patient Role of Duplex • Presence or absence of disease • Severity • Physiologic • Anatomic • Location • Single level • Asymptomatic • claudication • Multi-level • Claudication • Rest pain • ulcerations Pressures • Ankle/Brachial Index (ABI) • 1.0-1.2 Normal • 0.92-0.99 may indicate presence of arterial obstruction • <0.92 Evidence of arterial obstruction, claudication • <0.40 associated with rest pain or tissue loss Pressures--Toe • Photoplethysmography (PPG) • Infrared light which responds to changes in blood content near the surface of the skin • Waveform analysis and pressure measurement Pressures--Toe • Disease from the level of the ankle to the toe • Diabetics • Wound healing potential • Absolute number and index Pressures--Toe • A toe/ankle index >0.60 suggests the absence of hemodynamically significant obstruction between the ankle and the toe • A toe/brachial index >0.60 suggests the absence of hemodynamically significant obstruction between the heart and the digit Pressures--Toe TCPo2 • Transcutaneous oxygen tension • Evaluates oxygen delivery to tissue • Indirect measure of local blood flow • Aids in determining wound healing potential • Patient in supine position • Small electrodes placed at chest, below knee, and 2 over dorsum of foot • Electrodes in the sensors heat area underneath the skin to dilate capillaries • Results recorded and measured in mmHg • >30 mmHg – greater success for wound healing • <30 mmHg - suggests high likelihood of wound not healing Pressures--Segmental • Typically 3 or 4 cuff system • High thigh, above knee, calf, ankle • Measures pressure at each level • >30mmHg gradient from level to level is significant • >40mmHg indicates occlusion • >20mmHg from side to side is also significant Pressures--Segmental • Pitfalls include • Medial arterial calcification • Limb girth • Inappropriate cuff size • Can be uncomfortable for patient Pressures--Segmental Pulse Volume Recordings (PVR) • Measures pressure changes in the bladder of the cuff wrapped around the leg • These changes reflect change in cuff volume • Can use same cuffs as used for segmental pressures PVR • A 1mmHg pressure change detected in the cuff produces a 20mm deflection (amplitude) on the chart recorder • Using appropriate size cuffs, a preset pressure is obtained • A recording is then obtained PVR PVR/Segmental Pressures • PVR waveforms and segmental pressures are complimentary tests • If differences exist then a source of error should be investigated Duplex • Image based evaluation • Looking for anatomic disease and physiologic disease Duplex – Segmental Duplex PW Doppler--Duplex Velocity Ratio = v2/v1 V2= highest peak systolic velocity V1= proximal normal vessel Velocity Ratio (VR) = 6.1 Arterial Ulcers • Role of Duplex essential to understanding presence, location, and severity of disease • Guides intervention and management • Indicator wound healing potential Changing Gears Venous Ulcers • Result of sustained venous hypertension (Chronic venous insufficiency) • Incompetent valves or poor calf muscle pump • Local venous dilatation and pooling • Traps leukocytes that may release proteolytic enzymes that destroy tissues • May also “trap” important growth factors within vein rendering them unavailable for wound repair Venous • 70%-90% of chronic wound cases • Estimated 2.5 million patients in the US • Rarely fatal - can severely diminish quality of life Venous Ulcers • CVI Risk factors • > Age • Hx DVT • Surgery • Restricted mobility • CHF • Cancer • Obesity • Smoking • Family hx VTE • Hypercoable state (Factor V Leiden, Protein C/S deficiency, etc.) • Sedentary lifestyle • Varicosities Venous Ulcers • Wound characteristics • Gaiter region – medial malleolus • Superficial, irregular shape • Skin shiny and tight (edema) • Brown or purple discoloration – “stasis skin changes” Stasis Skin Changes Varicose Veins Varicose Veins Varicose Veins Varicose Veins • Complications • • • • • • • • Swelling Pain/aching itching Leg heaviness Phlebitis – inflammation of vein Superficial thrombophlebitis bleeding Cosmetic • Not commonly associated with venous ulcers when isolated to the superficial system Role of the Sonographer • Patient history • Physical exam • Clues to what is going on before you put the transducer on the patient Role of Duplex • Presence or absence of disease • Severity • Physiologic • Anatomic • Location • Deep • Superficial Venous Obstruction • Presence or absence of deep or superficial venous obstruction • Compression ultrasound Venous Obstruction • Thrombus Characteristics • Acute • • • • Softly echogenic Spongy Dilated vein Smooth borders • Chronic • • • • • Brightly echogenic Rigid Contracted vein Irregular borders Presence of collaterals Acute or Chronic? • These distinguishing characteristics are not absolute • “Can be useful in estimating the age of a thrombus and the risk of its embolization.” (Techniques of Venous Imaging. Talbot, Oliver. 1992) Venous Duplex • Complete and careful evaluation • Deep • • • • • CFV Fv Pop Tibials Gastrocs, soleals, etc. • Superficial • Great Saphenous Vein (GSV) • Small Saphenous Vein (SSV) • tributaries Venous Insufficiency • Evaluation of reflux (deep and superficial) • Supine • Manual hand augments • Standing • Rapid inflation/deflation cuff system • “stresses” vein – hydrostatic pressure • Valsalva • Patient unable to stand Venous Insufficiency • Patient standing • Cuff around calf • Rapidly inflates • Measure reflux on cuff deflation • Ergonomic challenges • Patient limitations Venous Insufficiency • Normal values • < 0.5 seconds • Abnormal • > 0.5 seconds • Indication of valvular incompetency (reflux) Perforator Assessment • Connection between deep and superficial systems • Drains superficial into deep system • Contain valves • Associated with ulcer formation Perforator Assessment • Dodd’s • Boyd’s • Cockett’s • Name given by 1st physician who described them Venous Duplex • Other considerations • Size of veins • May help determine intervention method • Too large may not respond well to local sclerotherapy or some types of venous ablation • “map” of veins • Anatomical blueprint sometimes required • Help guide intervening physician Venous Ulcers • Role of Duplex essential to understanding presence, location, and severity of disease • Guides intervention and management Conclusion • Patients presenting with ulcerations to the vascular lab is a common occurrence • Technologist and physician education important • Use all available skills and tools to assess your patients • Wound management is complex and your role is critical in providing the necessary vascular information Thank you!