Renal Physiology: Kidney Function & Urine Formation
advertisement

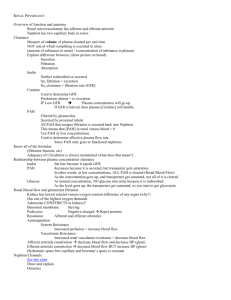
Renal Physiology PART ONE Renal Physiology Overview PART TWO Renal Clearance PART THREE Renal Acid-Base Balance 1 Role of the kidney in maintaining water, electrolytes, and pH balance Plasma leaks out of the capillaries in the glomerulus. The kidneys return the nutrients to the plasma, while removing the waste products. This also maintains the pH balance, since some of the wastes are acids and bases. Under the direction of aldosterone, they keep the balance between electrolytes, especially sodium and potassium. This keeps the plasma volume constant to maintain BP. 2 Role of Kidneys The kidneys can adjust blood volume, blood pressure, and blood composition BLOOD VOLUME Adjusts the volume of water lost in urine by responding to ADH, aldosterone, and renin BLOOD PRESSURE Releasing renin and adenosine (increases blood pressure) BLOOD COMPOSITION Releasing erythropoietin (increases RBC production) 3 Sympathetic Nervous System Effect on Kidneys Changes the rate of blood flow (and therefore, the pressure) to the glomerulus by telling the precapillary sphincters when to contract or relax. Sympathetic nervous system is stimulated by renin, which is released by the kidney. Causes changes in water and sodium reabsorption by the nephron 4 Hypothalamus The hypothalamus monitors the concentration of water in the plasma. If the plasma is too concentrated (high osmotic pressure), it means there are many electrolytes and not enough water inside the blood vessels (the person is dehydrated, and blood pressure will drop). Since water goes to the area that has the most particles (particles SUCK water!), water will be drawn out of the nearby cells, which will cause them to shrink. If the plasma is too dilute (low osmotic pressure), it means there is too much water and too few electrolytes inside the blood vessels (the person is over-hydrated, and blood pressure will rise). Water will be drawn out of the blood vessels to enter the nearby cells (causing them to swell) or the space between them (interstitial space). 5 Hypothalamus and Adrenal Gland When a person is dehydrated and has low blood pressure, the hypothalamus will sense that the osmotic pressure of the plasma is too high (above homeostatic levels; plasma is too concentrated: too many electrolytes and not enough water is in the plasma), it tells the pituitary gland to release ADH (antidiuretic hormone) to cause the kidneys to retain additional water to dilute the plasma. This will make the low blood pressure go back up. The adrenal cortex will also release aldosterone, which causes sodium ions to be reabsorbed by the kidneys, and water will follow. This will also increase the plasma volume (which will dilute it), and also help the low blood pressure to go back up. If the osmotic pressure is too low (plasma is too dilute: too much water and not enough electrolytes in the plasma), ADH and aldosterone are not released, and excess water will pass out of the body as urine. This will make the high blood pressure go back down. 6 Quiz Yourself What does it mean when the osmotic pressure is too high? Too low? What are the causes of each of these situations? How does the body compensate for each of these situations? What does it mean when the plasma is too dilute? Too concentrated? What are the causes of each of these situations? How does the body compensate for each of these situations? 7 pH Imbalances Many things can alter the pH of the blood Beverages we drink Acids produced by metabolism Breathing rate Vomiting (loss of acid) Diarrhea (loss of base) pH imbalances are dangerous because many enzymes only function within a narrow pH range. 8 Renal Physiology Basic Mechanisms of Urine Formation 1) Glomerular filtration 2) Tubular reabsorption 3) Tubular secretion 4) Excretion How do we determine these rates? Master formula 9 Glomerular Filtration The capillaries in the glomerulus contain many holes, called fenestrations. As blood passes through the glomerulus, the plasma passes through the fenestrations. Proteins and other large substances do not cross through; they stay in the bloodstream. The filtered plasma leaves the bloodstream in this way, and enters the glomerular capsule, and then enters the proximal convoluted tubule. 10 Glomerular Filtration In a sprinkler hose, the higher the water pressure, the faster the water squirts through its holes. The same process is also true for the glomerulus. The blood pressure inside the glomerulus affects how fast the fluid can filter through the fenestrations. Therefore, blood pressure affects the glomerular filtration rate (GFR). The higher the blood pressure, the higher the GFR. The pre-capillary sphincters can also control how much pressure is in the glomerulus, much like the water faucet controls the pressure in a hose. 11 Glomerular Filtration Rate GFR is used as a measure of kidney function. Normal GFR is 125 ml per minute for both kidneys combined. That means 7.5 liters per hour, or 180 liters per day. That is 45 gallons of filtrate produced per day! Of course, most of that is reabsorbed. Average urine output is about 1.2 liters per day. That means you need to drink 1.2 liters of fluid per day (remember that caffeine and alcohol are diuretics, so you need more than that to compensate if you drink those beverages). You need to drink more (about 2 liters per day) if you are getting a cold or flu. 12 Altering GFR Several different mechanisms can change the diameter of the afferent and efferent arterioles to alter the GFR: Hormonal (hormones) Autonomic (nervous system) Autoregulation or local (smooth muscle sphincters around the arterioles or capillaries near the glomerulus) 13 Remember the route the fluid takes: Glomerulus Proximal convoluted tubule (PCT) Descending limb of LOH Ascending limb of LOH Distal Convoluted tubule Collecting duct Tubular Reabsorption This is the process by which substance in the renal tubules are transferred back into the bloodstream. Reabsorption is the removal of water and solute molecules from filtrate after it enters the renal tubules. Fluid goes from the glomerulus to the proximal convoluted tubule (PCT), down the loop of Henle and back up, then into the distal convoluted tubule (DCT), and into the collecting duct. In the PCT, the nutrients are reabsorbed. If there are more nutrients than can be reabsorbed (such as excess sugar), it will be excreted in the urine. When the nutrients are reabsorbed (in the PCT), the inside of the tubule will have more water and less nutrients. Since water goes to the area that has a higher concentration of particles (osmosis), water will also leave the tubules; this occurs in the DCT. By the time the fluid has reached the collecting duct, nothing but 15 waste products are left, such as urea, ammonia, and bilirubin. Tubular Reabsorption Capillaries follow the renal tubules and wrap around them. The straight capillaries that travel longitudinally next to the tubules are called vasa recta, and the capillaries that wrap around the tubule are called peritubular capillaries. There is a space between the capillaries and the tube, called the peritubular space. 16 Tubular Reabsorption Tubular Cells Peritubular Capillaries Filtrate arriving from Bowman’s Capsule Lumen of Tubule The peritubular capillaries are nearby, and the particle concentration is low inside of them. Therefore, the particles in the peritubular space (high concentration of particles) will leave that space and enter into the peritubular capillaries by osmosis. That is how the nutrients are reabsorbed from the tubules back into the bloodstream. 17 Tubular Reabsorption The ascending limb of the Loop of Henle and the DCT are impermeable unless hormones cause substances to be moved through their walls. If the blood is low in sodium, (after excessive sweating), aldosterone (from the adrenal cortex) will cause more sodium to be pumped out of the tubule and into the peritubular space. The sodium will then enter the capillaries. Since water follows where salt goes, whenever the body needs more water (such as dehydration), ADH is released (from the neurohypophysis = posterior pituitary). ADH is also called vasopressin. Aldosterone and ADH will increase blood volume, increasing blood pressure. These two hormones begin their action in the ascending limb and continue to work in the DCT. 18 Tubular Secretion Some substances are unable to filter through the glomerulus, but are not wanted by the body. Examples are pollutants like pesticides, and many drugs, such as penicillin and non-steroidal anti-inflammatory drugs (NSAID’s). As blood passes through the peritubular capillaries, those substances are moved from the capillaries directly into the PCT and DCT. This is called tubular secretion. 19 Juxtaglomerular Apparatus The distal end of the renal tubule passes next to the glomerulus to form the juxtaglomerular apparatus (juxta means “next to”). 20 Juxtaglomerular Apparatus: Alters BP and GFR by autoregulation Two types of cells: 1) Macula densa cells 2) Juxtaglomerular cells 21 Juxtaglomerular Apparatus: Macula Densa Cells If blood pressure is too low, the macula densa releases adenosine, which causes vasoconstriction of the afferent arteriole. This will slow the GFR, so less water is lost, and blood pressure increases. 22 Juxtaglomerular Apparatus: Macula Densa Cells If blood pressure is too high, the macula densa stops releasing adenosine, which allows the sphincters to relax. This will increase GFR so more water is lost, and blood pressure decreases. 23 Juxtaglomerular Apparatus: Juxtaglomerular Cells Juxtaglomerular cells secrete renin if the blood pressure is still too low after adenosine has caused vasoconstriction. Renin causes more sodium to be reabsorbed, and water follows, so blood volume increases, so blood pressure increases. 24 Summary of Autoregulation The nephron can alter the blood pressure and flow into the glomerulus by autoregulation. The JGA senses the blood pressure going into the glomerulus and the flow rate of the fluid going through the renal tubule. If the GFR is too low, the JGA (macula densa) will cause the pre-capillary sphincters on the nearby arterioles to contract, increasing blood pressure, like turning up the faucet on a hose. If that restores the desired filtration rate and flow, no further action is needed. If not, the kidneys produce the enzyme renin, which makes the lungs produce angiotensin converting enzyme (ACE), which turns A1 into A2, which constricts blood vessels, and also causes the release of aldosterone, raising the blood pressure. 25 Hormonal Regulation If a person sweats from activity, eats very salty food, or has diarrhea, it changes the sodium and water content of the plasma. Two hormones that affect the ascending limb of the Loop of Henle are aldosterone and antidiuretic hormone (ADH). Adosterone is produced by the adrenal cortex and causes additional sodium ions to be pumped our of the tubule and into the bloodstream. Water comes with it by osmosis, and the blood pressure increases. ADH is produced by the posterior pituitary gland and causes retention of additional water from the DCT and collecting ducts. Sodium is not included in this process, so the result is to dilute the plasma during dehydration, when the plasma is becoming to concentrated with particles. 26 Erythropoietin The kidneys also monitor the oxygen content of the blood. If O2 levels are low, the JGA releases erythropoietin to stimulate the bone marrow to produce more red blood cells. 27 Neural Regulation The kidneys receive about 22% of the blood pumped out of the heart, so that is a substantial quantity passing through the kidneys at any given time. If there is a stressor and the sympathetic nervous system causes us to go into fight or flight mode, the skeletal muscles need to have a maximum amount of blood flow. Neurons from the sympathetic nervous system innervate the kidneys to decrease renal blood flow during critical situations. 28 Urine Urine contains ions such as sodium, chloride, and potassium, as well as suspended solids, known as sediments, such as cells, mineral crystals, mucus threads, and sometimes bacteria. The pH of urine is normally 4.6-8 A urinalysis can identify abnormal processes occurring in the body. Because urine is a waste product, its contents are influenced by the foods and drinks we ingest. We may lose fluid elsewhere, such as through sweating or diarrhea, which causes the urine to become more concentrated. Acids produced through metabolism can also change the pH of our urine. Even changes in breathing rate can change the urine pH as excess acids or bases are excreted to maintain normal plasma pH. 29 Abnormal Urinalysis These substances should not be in the urine. When they are, it is abnormal. Glucose Blood Protein Pus Bilirubin Ketones 30 Causes of abnormal UA Glucose: diabetes mellitus Blood: bleeding in urinary tract from infection or kidney stone Protein: kidney disease, hypertension, excessive exercise, pregnancy Pus: bacterial infection in urinary tract Bilirubin: liver malfunction Ketones: excessive breakdown of lipids 31 Micturition Urination is technically known as micturition. Once the volume in the urinary bladder exceeds 200 ml stretch receptors in its walls send impulses to the brain, indicating the need to eliminate. When you make the decision to urinate, the parasympathetic nervous system stimulates the smooth muscle in the urinary bladder’s internal sphincter to contract. Remember, the internal sphincter is smooth muscle (involuntary) and the external sphincter is skeletal muscle (voluntary). Both must relax for urine to exit. 32 Diuretics for hypertension and congestive heart failure Diuretics decrease plasma volume. This group of drugs are thiazide diuretics (such as Lasix). They inhibit the reabsorption of sodium and potassium from the renal tubule, causing more water to pass out as urine. Compared to sodium, the homeostatic range of potassium is quite narrow. Lasix (Furosemide) inhibits reabsorption of potassium more than other diuretics. Low blood levels of potassium are called hypokalemia. It is important for someone on Lasix to take potassium supplements or eat fruits or vegetables that have a lot of potassium (such as cantaloupe). However, too much potassium from excessive supplements can have fatal side effects. 33 Diuretics Furosemide (Lasix) Mannitol Spironolactone Amiloride 34 Homeostasis Maintaining the proper concentration of sodium and water is critical. If the plasma is too concentrated with particles, nearby cells can shrink and lose their function. If the plasma is too dilute, water can enter the nearby cells and cause them to expand, also decreasing their function. This is especially dangerous in the brain. Studies have shown a close link between obesity, diabetes, and kidney disease. Exercise helps maintain normal kidney function by increasing blood flow, and it decreases the incidence of high blood pressure. People receiving dialysis and those who have had kidney transplants especially need to exercise. 35