chapt12_lectureanimation_5e - Body-Health-and
advertisement

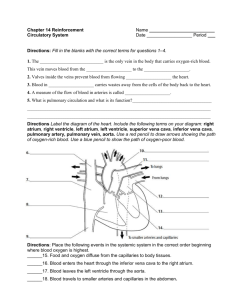
Chapter 12 Lecture Slides Copyright © The McGraw-Hill Companies, Inc. Permission required for reproduction or display. Learning Outcomes • Anatomy of the Heart 1. Identify the protective coverings of the heart. 2. Identify the parts of the heart and describe their functions. • Cardiac Cycle 3. Describe the events of the cardiac cycle. 4. Trace the flow of blood through the heart. • Heart Conduction System 5. Identify parts of the heart conduction system and describe their functions. Learning Outcomes • Regulation of Heart Function 6. Explain how the heart rate is regulated. • Types of Blood Vessels 7. Describe the structure and function of arteries, arterioles, capillaries, venules, and veins. 8. Describe how materials are exchanged between capillary blood and interstitial fluid. • Blood Flow 9. Describe the mechanism of blood circulation. Learning Outcomes • Blood Pressure 10. Compare systolic and diastolic blood pressure. 11. Describe how blood pressure is regulated. • Circulation Pathways 12. Compare the systemic and pulmonary circuits. • Systemic Arteries 13. Identify the major systemic arteries and the organs or body regions that they supply. Learning Outcomes • Systemic Veins 14. Identify the major systemic veins and the organs or body regions that they drain. • Disorders of the Heart and Blood Vessels 15. Describe the common disorders of the heart and blood vessels. • Heart and blood vessels are part of the cardiovascular system • Heart pumps blood • Arteries carry blood away from the heart to capillaries • Veins carry blood from capillaries to heart 12.1 Anatomy of the Heart • Four chambered muscular pump • Lies between the lungs, superior to the diaphragm • Pointed apex extends to left side at level of 5th rib • Protective Coverings – Pericardium surrounds the heart and associated blood vessels – Parietal and visceral pericardia are serous membranes • Secrete serous fluid into pericardial cavity • Functions to reduce friction during contraction – Parietal and visceral pericardia are serous membranes • Secrete serous fluid into pericardial cavity • Functions to reduce friction during contraction • The Heart Wall – Myocardium • Layer of cardiac muscle • Provides force for contraction – Epicardium (visceral pericardium) • Outer most layer • Contains blood vessels that nourish the heart – Endocardium • Inner layer • Heart Chambers – 2 atria • Receive blood from veins – 2 ventricles • Pump blood to arteries – Interventricular septum – Heart is a double pump • Left atria and ventricle: left pump • Right atria and ventricle: right pump – Differences in wall thickness depend upon work performed by the chamber • Ventricles have more muscle then atria: atria pump to ventricle, ventricles pump out to body areas • Left ventricle is most muscular: pumps blood to body • Right ventricle has less muscle: pumps blood to lungs only • Heart Valves – Blood flows in one direction through the heart due to valves – Atrioventricular valves • Prevents backflow • Tricuspid valve: between R atrium and R ventricle • Bicuspid valve (or mitral valve): between L atrium and L ventricle – Semilunar valves • Pulmonary semilunar valve: between R ventricle and pulmonary trunk • Aortic semilunar valve: between L ventricle and aorta 12.2 Cardiac Cycle • Includes: – Systole: contraction phase – Diastole: relaxation phase • Flow of Blood Through the Heart – Two basic circuits of blood flow • Pulmonary circuit – Deoxygenated blood flows from R ventricle to lungs – Oxygenated blood flows from lungs to L atrium • Systemic Circuit – Oxygenated blood flows L ventricle to body – Deoxygenated blood flows from body to R atrium • Steps of heart circulation – Superior and inferior vena cava return blood from body to R atrium – Pulmonary veins return blood from lungs to R atrium – Atria push blood into ventricles – R ventricle pumps blood into pulmonary trunk • Blood moves into R and L pulmonary arteries, which head to lungs – L ventricle pumps blood into the aorta, which carries blood out to body 12.3 Heart Conduction System • Conduction system consists of specialized muscle tissue that acts as neural tissue – Spontaneously form impulses – Impulses cause myocardium to contract • Components include – Sinoatrial (SA) node – Atrioventricular (AV) node – AV bundle – Purkinje fibers • Sinoatrial node – Pacemaker of the heart – Rhythmically forms impulses to initiate each heartbeat – Impulses cause simultaneous contraction of atria • Atrioventricular node – Receives impulse from SA node – Delay in passing through node allows time for ventricular filling and the completion or atrial contraction – Passes impulse to the AV bundle • AV bundle – Divides into L and R branches – Carries impulse down ventricular septum and up lateral ventricle walls – Forms Purkinje fibers • Purkinje fibers – Carry impulse to myocardium of ventricles – Contraction occurs from the apex upward • Electrocardiogram (ECG or EKG) – Recording of the electrical current generated during heart contraction – Performed by an electrocardiograph – Electrocardiogram has three distinct waves • P wave: atrial depolarization • QRS wave: ventricular depolarization • T wave: ventricular repolarization • Other factors affecting heart rate – Age: resting rate declines with age – Sex: females slightly faster than males – Physical condition: good condition means lower heart rate – Temperature: increase in temperature increases rate – Epinephrine: increases strengthens heart rate – Thyroxine: produces a lesser but longer lasting increase in heart rate – Blood calcium levels • Low levels slow heart rate • Increased levels increase heart rate and prolong contraction – Blood potassium levels • Increased layers decrease both heart rate and force of contraction • Low levels can cause abnormal heart rhythms • Arteries – Carry blood away from the heart – Branch into smaller arteries, eventually forming arterioles • Play an important role in controlling blood flow and blood pressure 12.7 Blood Pressure • Arterial blood pressure in the systemic circuit – Systolic blood pressure • Highest pressure during ventricular systole – Diastolic blood pressure • Lowest pressure during ventricular diastole • Factors Affecting Blood Pressure – Cardiac output • Volume of blood pumped by heart in one minute – Determined by heart rate and blood volume pumped in contraction • Increase cardiac output, increase blood pressure • Decrease cardiac output, decrease blood pressure – Blood volume • Decrease in blood volume, decrease in blood pressure • Increase in blood volume, increase in blood pressure – Peripheral resistance • Friction of blood against blood vessel walls • Constriction of arterioles increase both resistance and blood pressure • Dilation of arterioles decreases both resistance and blood pressure 12.11 Disorders of the Heart and Blood Vessels • Grouped into – Heart disorders – Blood vessel disorders Heart Disorders • Arrhythmia – Abnormal heart beat – Caused by factors such as damage to conduction system and drugs – Includes: • Bradycardia – Heart rate less then 60 beats/min • Tachycardia – Heart rate over 100 beats/min • Heart flutter – Heart rate over 200-300 beats/min • Fibrillation – Very rapid heart rate with uncoordinated contraction – Blood is not pumped from ventricles • Congestive heart failure (CHF) – Acute or chronic inability of hear to pump out returned to it – Symptoms include fatigue, edema, accumulation of blood in organs – Possible cause is atherosclerosis • Heart murmurs – Unusual heart sounds associated with defective heart valves • Myocardial infarction – Death of myocardium due to coronary artery blockage – Heart attack • Pericarditis – Inflammation of pericardium due to viral or bacterial infection Blood Vessel Disorders • Aneurysm – Weakened vessel wall bulges, forming balloon-like sac filled with blood – Rupture can be fatal • Arteriosclerosis – Hardening of the arteries – Due to calcium deposits accumulating in tunica media • Atherosclerosis – Formation of fatty deposits in the tunica interna of arteries – Plagues reduce lumen size and increase probability of blood clot formation • Hypertension – Chronic high blood pressure – Pressure exceeds 140/90 – Pre-hypertension • A systolic pressure between 120-139 and diastolic pressure between 80-89 – Causes include stress and smoking • Phlebitis – Inflammation of a vein – Most common in the legs – Thrombophlebitis involves the formation of blood clots at the inflammation site • Varicose veins – Dilated, swollen veins due to malfunctioning valves – Causes include heredity, pregnancy, and lack of physical activity – Hemorrhoids