Metabolic acidosis

Acidosis
Dr. Elmukhtar Habas
PhD
Fachärzt Internal Medicine
Fachärzt Nephrology
Dr. med.
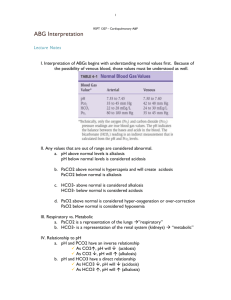
Normal ABG
PaCO2
PaO2
pH
Bicarbonate
BE
4.8-6.1 kPa
10-13.3 kPa
7.35-7.45
22-26 mmol/L
Base Excess
(35-45 mmHg)
(75-100 mmHg)
[H+] 35-45 mol/L
-2 to +2
Acid-Base disturbance disturbance PH
Metabolic Low
Acidosis
Respiratory Low
Acidosis
Metabolic
Alkalosis
Respiratory
Alkalosis
High
High
Pco2
Low
High
High
Low
HCO3
Low
High
High
Low
Normal ABG 7,36-7,44 35-45mmHg 22-26 mmol/l
EC pH
LOW NORMAL HIGH
Acidemia
Metabolic
Acidosis
Respiratory
Acidosis
No disturbance
Or
Mixed disturbance
Mixed if PCO2+HCO3 both low or both high or plasma anion gap wide
Metabolic
Alkalosis
Alkalemia
Respiratory
Alkalosis
Low HCO3
High PCO2
High HCO3 Low PCO2
Definition of Acidosis
Is a process that tends to lower the extracellular fluid pH (which is equivalent to raising the hydrogen concentration) that can be either by
A) a fall in the ECF (or plasma ) bicarbonate concentration.
b) an elevation in the PCO2 in ECF.
Types of Acidosis
Metabolic acidosis.
-Low bicarbonate, low PH, normal PCO2.
-Usually associated with hyperK .
Respiratory acidosis:
-Low PH, high PCO2 &Normal or high Hco3
-can be hyperk+
Each day approximately 15,000 mmol of carbon dioxide (which can generate carbonic acid as it combines with water) and 50 to 100 meq of nonvolatile acid
(mostly sulfuric acid derived from the metabolism of sulfur-containing amino acids) are produced.
Acid-base balance is maintained by normal pulmonary and renal excretion of carbon dioxide and acid, respectively.
Renal excretion of acid involves the combination of hydrogen ions with urinary titratable acids, particularly phosphate (HPO42- + H+ —> H2PO4-) or with ammonia to form ammonium.
since ammonia production from the metabolism of glutamine can be appropriately increased in the presence of an acid load.
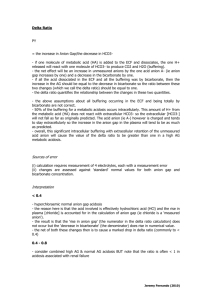
Henderson-Hasselbalch equation:
pH = 6.10 + log ([HCO3-] ÷ [0.03 x PCO2])
-pH is equal to (-log [H+])
-6.10 is the pKa (equal to -log Ka).
-Ka is the dissociation constant for the reaction
-0.03 is equal to the solubility constant for CO2 in the extracellular fluid.
-PCO2 is equal to the partial pressure of carbon dioxide in the extracellular fluid .
Metabolic acidosis diagnostic chart
diagnosis
Lab diagnostic
Metabolic acidosis Low Hco
3
, low Ph normal
AG= Na+ - (Cl- +HCO -
3
)
AG > 12mmol/l
Lactat, Acetoacetic, β-hydrxybutyric acid high
HCO -
3 loss, RF, RTA
Lactic or ketoacidosis normal
Osmatic gape= measured osmolality-
(Na+ + K+)+glucose/18+ urea/2.8
High OG>10mosm/Kg
Methanol, ethylglycol or other intoxication
Renal Tubular acidosis
Four types
Type 1. Distal renal tubular acidosis characterized by…….
Type II. Proximal renal tubular acidosis characterized by…….
Type III Mixed
Type IV
ANION GAP
AG = Na - (Cl + HCO3).
The normal plasma AG had been considered to range between 7 and 13 meq/L.
knowing the normal range in a particular laboratory is often essential.
Calculation
Anion gap AG = Na+ - (Cl- +HCO-3).
8-10mmol/l. hypoabulminaemia reduce AG.
Osmotic gape (OG) =measured osmolality- calculated osmolality.
<10mosm/Kg
Calculated Osmolality = (Na + + K + )+glucose/18+ urea/2.8.
ANION GAP
primarily determined by the negative charges on the plasma proteins, particularly albumin. patients with hypoalbuminemia. AG falling by about
2.5 meq/L for every 1 g/dL (10 g/L) reduction in the plasma albumin concentration.
ANION GAP
A.
B.
C.
an increase in the AG can be induced by a fall in unmeasured cations (hypocalcemia or hypomagnesemia) more commonly and more markedly, by a rise in unmeasured anions (as with hyperalbuminemia due to volume contraction or the accumulation of an organic anion in metabolic acidosis).
Hypoalbuminemia (decreased unmeasured anions) and hyperk+ (increased unmeasured cations) lower the AG.
Initial screening to differentiate the high-AG acidose
(1) history for evidence of drug and toxin ingestion and measurement of arterial blood gas to detect coexistent respiratory alkalosis
(salicylates).
(2) determination of whether diabetes mellitus is present (diabetic
Ketoacidosis)
(3) a search for evidence of alcoholism or increased levels of -hydroxybutyrate (alcoholic ketoacidosis)
(4)observation for clinical signs of uremia and determination of the blood urea nitrogen (BUN) and creatinine (uremic acidosis)
(5) Inspection of the urine for oxalate crystals (ethylene glycol).
(6) Recognition of the numerous clinical settings in which lactate levels may be increased (hypotension, shock, cardiac failure, leukemia, cancer, and drug or toxin ingestion).
Elevated anion gap
The diagnostic utility of a high AG is greatest when the
AG is above 25 meq/L.
Lactic acidosis, usually due to marked systemic hypoperfusion or to malignancy.
Ketoacidosis due to diabetes mellitus, alcohol, or fasting, in which ß-hydroxybutyrate is the primary unmeasured anion.
Is modestly in nonketotic hyperglycemia even though there is little or no metabolic acidosis. In this setting, due to the phosphate &other anions release from the cells .
Elevated anion gap
Most of renal failure, in whom there is retention of both hydrogen and anions, such as sulfate, phosphate, and urate.
Ingestion of methanol, glycolate and oxalate with ethylene glycol &aspirin. metabolic acidosis may be absent and the anion gap may be normal in methanol or ethylene glycol intoxication if there is concurrent alcohol ingestion.
Urinary anion gap
To evaluate metabolic acidosis in normal anion gap.
As to distinguish the cause is from renal or GIT (
Diarrhoea )
URINARY ANION GAP =
( Urinary Na + Urinary K ) – Urinary Cl
If –ve the cause is diarrhea GIT
If +ve the cause is distal renal tubular acidois.
HIGH-ANION-GAP ACIDOSES
The goal is to increase the [HCO3]to 10 meq/L and the pH to 7.15, not to increase these values to normal.
There are four principal causes of a high-HIGH
AG acidosis:
(1) lactic acidosis.
(2) ketoacidosis.
(3) ingested toxins.
(4) acute and chronic renal failure.
normal anion gap metabolic acidosis
U ureterosignoidostomy
S saline in presence of CRI
E endocrine - hypoaldosteronism
D diarrhoea
C carbonic anhydrase inhibitor
A ammonia or alimentation eg TPN
R renal tubular acidosis
Metabolic acidosis with High AG
Cause
Lactic acidosis.
Shock, hypoxia, metformin, hepatitis.
Ketoacidosis.
DM,alchol, hunger
Main anion lactate
Clinic/lab
Kussmaul breath
Intoxications.
Aspirin. methanol, ethylachol, paraldehyde
ARF &CRF
Acetoacetic, βhydrxybutyric acid
Salicylic, format,glycol/ lactat, acetat
Kussmaul breath, Eventually coma, ketonurea
High OG, ARF
Sulphate, phosphate
S Urea, Cr. Olig/anuria
Metbolic acidosis with normal AG
Acid infusion
.
- Arginin chloride.
HCO
3
loss:
- Urtersigmoidostoy, ileum conduct to ureter or bladder.
- Diarrhoea.
- Carbonic anhydrase inhibitor. Timolol.
- RTA type II.
Reduced H+-secretion, NHr-excretion.
- RTA typeI&IV.
Reduced NH3+ formation, reduced distal Nh3+ excretion.
- ARF, hypoaldosternism & hyperkalaemia.
Metabolic acidosis and anion gap
High Anion gape M. A.
High A.G with normochloremic M.A.
Normal A.G metabolic acidosis
Hypercholeraemic M.A.
Increased production of acid or acid equivalant substances
Ketoacidosis: DM, Hunger, Alchol.
Lactatic acidosis: Tissue hypoxia by cardiac shock, respiratory insufficiency, malignacy, liver cell failure.
Intoxication with Methanol, Ethyle glycole,Biguanides.
Decrease in acid excretion by kidney as in CRF, ARF
Renaltubular dysfunction as in RTA
Loss of HCO3: Diarrhea, carbonic anhydrase inhibitor (dimox
Ingestion of acid with chloriode
Clinical presentation
Tachycardia.
Breathlessness.
Low BP.
Headache.
Electrolyte disorder.
Dizziness.
Coma.
General principles of treatment 1
A.
B.
C.
varies markedly with the underlying disorder.
The aim Rx is restoration of a normal extracellular pH.
exogenous alkali may not be required if the acidemia is not severe (arterial pH >7.20), the patient is asymptomatic, and the underlying process, such as diarrhea that can be controlled
General principles of treatment 2
In other settings, correction of the acidemia can be achieved more rapidly by the administration of sodium bicarbonate IV.
The initial aim of therapy is to raise the systemic pH to above 7.20; this is a level at which the major consequences of severe acidemia should not be observed.
HIGH-ANION-GAP ACIDOSES
The goal is to increase the [HCO3]to 10 meq/L and the pH to 7.15, not to increase these values to normal.
There are four principal causes of a high-HIGH
AG acidosis:
(1) lactic acidosis.
(2) ketoacidosis.
(3) ingested toxins.
(4) acute and chronic renal failure.
Treatment
Treat the underlying cause.
NaHCO
3
+ . Indication of NaHCO
3
+ infusion.
- Significant hyperkalaemia with PH < 7.1.
- Bicarbonate < 8 & K + <3mmol/l substitution is given.
Calculation of bicar mmol/l . Substitution=
KG(kg)x0,7x(desired NaHCO3+– NaHCO3+).
Haemodialysis. In severe RF or sever acidosis with hyperkalaemia
Calculation of bicarbonate deficit
If the respiratory function is normal, pH of 7.20 usually requires raising the plasma bicarbonate to
10 to 12 meq/L .
HCO3 deficit = HCO3 space xHCO3 deficit /L.
Bicarbonate space =[0.4 + (2.6 ÷[HCO3])
] x body weight ( kg).
If more alkali is given, oral Nahco3 or citrate
(metabolised to Hco3can replace IV therapy.
Treatment
In server case when PH < 7.1
NaHCo3 8,4 can be given: 1ml=Immol/.
Needed NaCO3= neg. Bace excess x 0,3. Kg(KG).
-divided to halfs… the last half according to ABG
Be careful about Hypokalemia and over correction.
In chronic metabolic acidosis:
slow correction with oral calcium or sodium bicarbonate up to 10g/day
Advice
In acidosis
Do not be hurry for Bicarbonate infusion before you are sure that PH of blood
< 6.9 and you should contact your superior
.
Respiratory acidosis (RA)
High CO 2 and low PH.
Acute RA:
Respiratory passage obstruction cardiopulmary arrest neuromuscular defect restrictive LD mechanical defect of respiration respiratory centre defect.
Chronic RA.:
COAD lesion of respiratory centres defect obesity
COAD restrictive LD.
Treatment
Acute RA.
Treat the underlying diseases.
O
2 inhalation.
Chronic RA.
Therapy of the underlying disease.
Controlled O2 inhalation and slow correction.
Slow correction of PCO
2
.
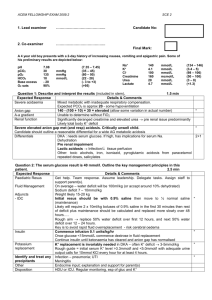
Case 1
A patient with diarrhea has an arterial pH of 7.23, bicarbonate concentration of 10 meq/L, and PCO2 of
23 mmHg. The low pH indicates acidemia, and the low plasma bicarbonate concentration indicates
What?
pH
PCO2
PO2
HCO3
BE
Na
K
Cl
1
st
Example
7.24
35 mmHg
90 mmHg
12 mmol/L
- 10 mmol/L
145 mmol/L
4 mmol/L
100 mmol/L
pH
PCO2
PO2
HCO3
BE
Na
K
Cl
2
nd
Example
7.30
40 mmHg
85 mmHg
18 mmol/L
- 5 mmol/L
130 mmol/L
4 mmol/L
104 mmol/L
pH
PCO2
PO2
HCO3
BE
Na
K
Cl
3
rd
Example
7.25
60 mmHg
70 mmHg
22 mmol/L
- 8 mmol/L
139 mmol/L
4.3 mmol/L
105 mmol/L
7.00
20 mmHg
88 mmHg
13 mmol/L
- 10 mmol/L
139 mmol/L
4.3 mmol/L
105 mmol/L
5.3 mg/dl
250 mg/dl
299mg%
4
th
Example
pH
PCO2
PO2
HCO3
BE
Na
K
Cl
Crea.
Urea
FBS