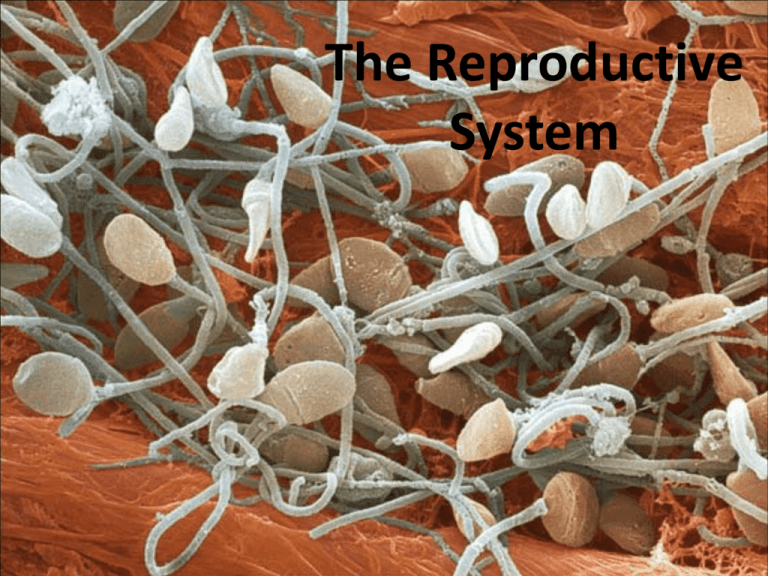
The Reproductive
System
Reproduction
• Sexual determination and differentiation
• Gross anatomy
• Functions
• Gametogenesis
Prenatal Hormones and Sex Differentiation
• Fetus is sexually undifferentiated as to which sex it will become
• Gonads begin to develop at 5 or 6 weeks as gonadal ridges
• Two sets of ducts adjacent to each gonadal ridge
– mesonephric ducts develop into male reproductive system
• paramesonephric ducts degenerate
– paramesonephric ducts (müllerian ducts) develop into female reproductive tract
• mesonephric ducts degenerate
• SRY gene (sex-determining region of Y chromosome)
– in males, codes for a protein, testes-determining factor (TDF), that initiates
development of testes
• begin to secrete testosterone 8 to 9 weeks
• stimulates mesonephric ducts to develop into the male anatomy
• secrete müllerian-inhibiting factor = degeneration of the paramesonephric ducts
• Female development occurs in absence of androgen hormones
– Estrogen levels always high during pregnancy
Copyright © The McGraw-Hill Companies, Inc. Permission required for reproduction or display.
Development
of Reproductive
Tracts
Mesonephros
Mesonephric duct
Gonadal ridge
Paramesonephric
(müllerian) duct
Kidney
Cloaca
5- to 6-week embryo;
sexually indifferent stage
Male
Testes
Ovaries
Efferent ductules
Paramesonephric
duct forming the
uterine tube
Epididymis
Paramesonephric
duct (degenerating)
Mesonephric duct
(degenerating)
Mesonephric duct
forming the
ductus deferens
Fused paramesonephric
ducts forming
the uterus
Urinary bladder
Urinary bladder
(moved aside)
Seminal vesicle
Urogenital sinus
forming the urethra
7 to 8 weeks
Urinary
bladder
Urogenital sinus
forming the urethra
and lower vagina
8 to 9 weeks
Uterine
tube
Ovary
Seminal
vesicle
Prostate gland
Bulbourethral
gland
Uterus
Urinary bladder
(moved aside)
Ductus deferens
Epididymis
Figure 27.3
Female
Vagina
Testis
Urethra
Urethra
Hymen
Vestibule
Penis
At birth
At birth
Development of External Genitalia
• Similarity of external genitalia of both sexes :
– genital tubercle becomes the head (glans) of the penis or glans
clitoris
– pair of urogenital folds encloses urethra of male forming the penis
or forms the labia minora
– pair of labioscrotal folds becomes either scrotum or labia majora
• Distinct male or female genitalia developed by week 12
• Homologous organs - male and female organs that develop
from same embryonic structure
– penis is homologous to the clitoris
– scrotum is homologous to the labia majora
Copyright © The McGraw-Hill Companies, Inc. Permission required for reproduction or display.
Genital tubercle
Urogenital fold
Development of
External Genitalia
Labioscrotal fold
Tail
6 weeks
8 weeks
Female
Male
Phallus:
Developing glans
of penis
Developing glans
of clitoris
Urethral groove
Labia minora
Urethral groove
Labia majora
Anus
Anus
10 weeks
10 weeks
Urethral orifice
Glans of penis
Prepuce
Prepuce
Glans of clitoris
Urethral orifice
Vaginal orifice
Scrotum
Perineal raphe
Perineal raphe
Anus
Figure 27.4
Anus
27-6
12 weeks
12 weeks
Functions
• Production of haploid gametes
• Endocrine functions
• Copulatory organs
• Nurture and develop embryos
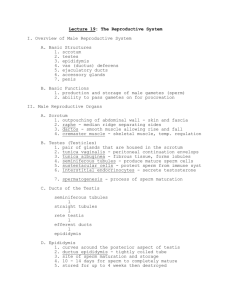
Male Reproductive System
• Primary sex organs
– Testis
• Accessory organs
– Duct system
• Epididymis
• Vas deferens
• Urethra
– Glands
• Seminal vesiscle
• Prostate
• Bulbourethral
– Penis
Testes
• Sperm production
• Secretion of
testosterone
– Interstitial cells
Histology of Testis
Copyright © The McGraw-Hill Companies, Inc. Permission required for reproduction or display.
Interstitial cells
Blood vessel
Germ cells
Blood vessel
Sustentacular cell
Seminiferous
tubule
Tails of spermatozoa
Spermatids
Sustentacular
cell nuclei
Tubule lumen
Germ cells
(a)
Connective tissue
wall of tubule
Interstitial cells
(b)
50 µm
a: Copyright by R.G. Kessel and R.H. Kardon, Tissues and Organs: A Text-Atlas of Scanning Electron Microscopy, 1979, W.H. Freeman, All rights reserved; b: © Ed Reschke
Figure 27.10 a-b
The Scrotum and Spermatic Cord
Copyright © The McGraw-Hill Companies, Inc. Permission required for reproduction or display.
External inguinal ring
Spermatic cord:
Cremaster muscle
Testicular artery
Fascia of spermatic cord
Superficial fascia of penis
Deep fascia of penis
Ductus deferens
Pampiniform plexus
Prepuce (foreskin)
Epididymis
Glans
Tunica vaginalis
Median septum of scrotum
Testis
Cremaster muscle
Dartos muscle
Scrotal skin
Figure 27.7
Countercurrent Heat Exchanger
Copyright © The McGraw-Hill Companies, Inc. Permission required for reproduction or display.
Pelvic cavity
37°C
Testicular artery
Pampiniform plexus
Blood flow
Blood flow
Heat transfer
Arterial blood cools
as it descends
Venous blood carries
away heat as it ascends
Key
35°C
Figure
27.8
Warmest
blood
Testis
Coolest
blood
Spermatogenesis
Spermiogenesis
Copyright © The McGraw-Hill Companies, Inc. Permission required for reproduction or display.
• Spermiogenesis changes that
transform
spermatids into
spermatozoa
– discarding excess
cytoplasm and
growing tails
Golgi complex
Acrosomal
vesicle
Nucleus
Bridge to
adjacent
spermatid
Acrosome
Head
Axoneme
Mitochondria
Basal
body
Flagellum
Midpiece
of tail
Excess
cytoplasm
Appearance
of
1
acrosomal vesicle
and flagellum in
2 Growth of
spermatid
acrosome
and flagellum
3 Shedding of
excess
cytoplasm
Figure 27.16
4 Mature sperm
Spermatozoon
• Spermatozoon two parts: head and tail
– head is pear-shaped
• 4 to 5 microns long structure containing the nucleus, acrosome and
basal body of the tail flagella
• nucleus contains haploid set of chromosomes
• acrosome – enzyme cap over the apical half of the nucleus that contains
enzymes that penetrate the egg
• basal body – indentation in the basal end of the nucleus where flagellum
attaches
• Tail is divided into 3 regions:
– midpiece contains mitochondria around axoneme of the
flagella, produces ATP for flagellar movement
– principal piece is axoneme surrounded by sheath of supporting
fibers
• constitutes most of tail
– endpiece is very narrow tip of flagella
Spermatozoon
Copyright © The McGraw-Hill Companies, Inc. Permission required for reproduction or display.
Acrosome
Head
Nucleus
Basal body
Mitochondrion
Midpiece
of tail
Axoneme
Figure 27.17 a-b
Principal
piece of
tail
Endpiece
of tail
2 µm
(b)
(a)
a: Visuals Unlimited
Duct System
• Epididymis
– Stores sperm until ejaculation
– Mature and gain motility
• Vas deferens
– Peristaltic contractions propel sperm toward
urethra
– Terminates at ejaculatory duct (seminal vesicle)
• Urethra
– Used in urinary system as well
– Three regions
• Prostatic
• Membranous
• spongy
Copyright © The McGraw-Hill Companies
Glands
• Seminal Vesicles (seminal fluid)
– Alkaline fluid
• Fructose, prostaglandins, vesiculase
• Prostate
– Citrate
– Sperm activating enzyme
• Bulbourethrals
– Neutralizing and cleansing mucus
• Sperm + glandular secretions = semen
– 2 – 5 ml, 110 million sperm per ml
Copyright © The McGraw-Hill Companies
Penis
• Copulatory organ in males
• Erectile tissue
– Corpora spongiosum
– Corpora cavernosa
Anatomy of Penis
Copyright © The McGraw-Hill Companies, Inc. Permission required for reproduction or display.
Dorsal vein
Dorsal
Dorsal artery
Dorsal nerve
Corpus spongiosum
Corpus cavernosum
Deep artery
Deep fascia
Tunica
albuginea
Superficial fascia
Skin
Lacunae
Urethra
Median septum
Corpus spongiosum
Prepuce
Glans of penis
External urethral orifice
(a)
Figure 27.12 a-b
(b)
Ventral
Male Sexual Response
• Excitement marked by erection
• Orgasm marked by ejaculation
• Resolution
Hormonal Regulation
• GnRH
• LH and FSH
• Testosterone
– Sperm production
– Male secondary sexual
characteristics
Aging and Sexual Function
• Decline in testosterone secretion
– peak secretion at 7 mg/day at age 20
– declines to 1/5 of that by age 80
• decline in the number and activity of interstitial cells (testosterone) and
sustentacular cells (inhibin)
• Rise in FSH and LH secretion after age 50 produces male
climacteric (andropause)
– little or no effect to mood changes, hot flashes and “illusions of
suffocation”
• Erectile dysfunction (impotence)– the inability to produce or
maintain an erection sufficient for intercourse
– 20% of men in 60s to 50% of those in 80s
Functions
• Same as in male
– Gametogenesis
– Hormone production
– Copulatory organs
• Nurture and develop embryo
Sexual Differentiation
• Female reproductive tract develops from the
paramesonephric ducts
– not because of the positive action of any hormone
– Due to absence of testosterone and müllerian-inhibiting factor
(MIF)
• Absence of testosterone:
•
•
•
•
causes mesonephric ducts to degenerate
genital tubercle becomes the glans clitoris
urogenital folds become the labia minora
labioscrotal folds develop into the labia majora
• Absence of MIF:
• paramesonephric ducts develop into the uterine tubes, uterus, and
vagina
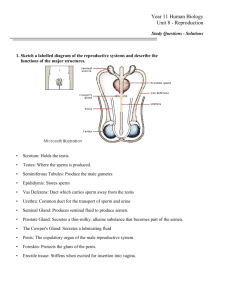
Female Reproductive System
• Primary Sex organ
– Ovaries
• Accessory Organs
– Duct system
• Uterine tubes
• Uterus
• Vagina
– External genitalia
•
•
•
•
•
Mons pubis
Labia
vestibule
Greater vestibular gland
clitoris
tutorvista.com
Duct System
• Uterine tubes
– Receives oocytes
– Site for fertilization
• Uterus
– Receive, nourish fertilized ovum
– Site of embryological and fetal
development
• Vagina
– Copulatory organ
– Birth canal
Uterine Wall
• Perimetrium - external serosa layer
• Myometrium - middle muscular layer
– constitutes most of the uterine wall
– composed mainly of smooth muscle
• sweep downward from fundus and spiral around the body
• less muscular and more fibrous near cervix
• produces labor contractions, expels fetus
• Endometrium – inner mucosa
– simple columnar epithelium, compound tubular glands, and a stroma
populated with leukocytes, macrophages, and other cells.
• stratum functionalis – superficial half, shed each menstrual period
• stratum basalis - deep layer, stays behind and regenerates a new stratum
functionalis with each menstrual cycle
– during pregnancy, the endometrium is the site of attachment of the embryo
and forms the maternal part of the placenta from which the fetus is
nourished
Histology of Endometrium
Copyright © The McGraw-Hill Companies, Inc. Permission required for reproduction or display.
Surface epithelium
Endometrial gland
Lamina propria
Figure 28.6 (1)
© Ed Reschke
0.1 mm
Vessels of Reproductive Tract
Copyright © The McGraw-Hill Companies, Inc. Permission required for reproduction or display.
Suspensory
ligament
Ovarian branch
of uterine artery
Mesosalpinx
Aorta
Common
iliac artery
Arcuate artery
Ovarian
artery
Ovary
Vaginal
artery
Uterine
artery
Internal iliac artery Spiral arteries
Figure 28.7
28-30
Ligaments
• Uterus supported by the muscular floor of the pelvic outlet
and folds of peritoneum that form ligaments around the
organ
– Broad ligament has two parts
• mesosalpinx
• mesometrium on each side of the uterus
– Cardinal (lateral cervical) ligaments – supports the cervix and superior
part of the vagina extending to the pelvic wall
– Uterosacral ligaments – paired and attach posterior side of the uterus
to the sacrum
– Round ligaments – paired and arise from the anterior surface of the
uterus, pass through inguinal canals, and terminate in the labia
majoris
• much like the gubernaculum terminating in the male scrotum
Uterus
Copyright © The McGraw-Hill Companies, Inc. Permission required for reproduction or display.
Infundibulum Ampulla
Isthmus
Fundus
Body
Ovarian
ligament
Mesosalpinx
Uterine
tube
Ovarian artery
Ovarian vein
Suspensory
ligament
Ovary
Fimbriae
Myometrium
Endometrium
Internal os
Cervical canal
Round
ligament
Lateral fornix
Cardinal
ligament
Mesometrium
Uterosacral
ligament
Cervix
External os
Vagina
(a)
Figure 28.3a
28-32
Vagina
• Vagina (birth canal) – 8 -10 cm distensible muscular tube
– allows for discharge of menstrual fluid, receipt of penis and semen, and
birth of baby
– outer adventitia, middle muscularis, and inner mucosa
– tilted posteriorly between rectum and urethra
– vagina has no glands
• transudation lubricates vagina – “vaginal sweating”
– serous fluid through its walls and by mucus from the cervical gland above it
– fornices – blind-ended spaces formed from the vagina extends slightly
beyond the cervix
– transverse friction ridges (vaginal rugae) at lower end
– mucosal folds form hymen across vaginal opening
• Vaginal epithelium
– childhood - simple cuboidal
– puberty - estrogens transform to stratified squamous
• bacteria ferment glycogen rich cells producing acidic pH in vagina
– an example of metaplasia – the transformation of one tissue type to
another
– antigen-presenting dendritic cells – route by which HIV from infected
semen invades the female body
The External Genitalia
• External genitalia are collectively called the vulva or pudendum
– mons pubis - mound of fat over pubic symphysis bearing most of the
pubic hair
– labia majora – pair of thick folds of skin and adipose tissue inferior to the
mons
• pudendal cleft – slit between labia majora
– labia minora – medial to labia majora are thin hairless folds
• space between forms vestibule which contains urethral and vaginal openings
• anterior margins of labia minora join to form hood-like prepuce over clitoris
– clitoris - erectile, sensory organ with no urinary role
• primary center for erotic stimulation
• glans, body, and crura
– vestibular bulbs - erectile tissue deep to the labia majora
• cause the vagina to tighten around the penis, enhancing sexual stimulation
– greater and lesser vestibular and paraurethral glands open into vestibule
for lubrication
Ovaries
• Ova production
• Secretions
– Estrogens
– Progesterone
med.saisayan.com
Oogenesis
Ovarian Cycle
• Follicular phase
– Maturation of
primordial follicle
– Production of secondary
oocyte
• Ovulation
• Luteal phase
– Corpus luteum
– Progesterone secretion
med.saisayan.com
The Uterine Cycle
• Cyclic changes to endometrium
• Days 1-5, menstrual phase
– Shedding of stratum functionalis
– Bleeding 3-5 days
• Days 6-14, proliferative phase
– Proliferation of endometrium
– Prep for implantation
• Days 15-28, secretory phase
– Secretion of glycoproteins
– Thickening of cervical mucus
• Hormonal
regulation
of ovarian
and uterine
cycles
Breasts and Mammary Glands
• Breast – mound of tissue overlying the pectoralis major
– enlarges at puberty
– most of time contains very little mammary gland
• Mammary gland – develops within the breast during
pregnancy
– remains active in the lactating breast
– atrophies when a woman ceases to nurse
• Principal regions of the breast:
– body – conical to pendulous, with the nipple at its apex
– axillary tail – extension toward the armpit
• lymphatics in axillary tail are important as a route for breast cancer metastasis
Breasts and Mammary Glands
• Nipple surrounded by circular colored zone the areola
– sensory nerve fibers of areola trigger a milk ejection reflex
when an infant nurses
– areolar glands – intermediate between sweat glands and
mammary glands
• secretions protect the nipple from chapping and cracking during
nursing
– smooth muscle fibers in dermis of areola that contract in
response to cold, touch, and sexual arousal wrinkling the skin
and erecting the nipple
Anatomy of Lactating Breast
Copyright © The McGraw-Hill Companies, Inc. Permission required for reproduction or display.
Rib
Intercostal muscles
Pectoralis minor
Pectoralis major
Fascia
Suspensory ligament
Lobules
Lobe
Adipose tissue
Nipple
Lactiferous sinus
Lactiferous duct
Figure 28.9c
28-42
(c) Sagittal section
Climacteric and Menopause
• Climacteric -midlife change in hormone secretion
– accompanied by menopause – cessation of menstruation
• Female born with about 2 million eggs, climacteric begins when there are
about 1000 follicles left
–
–
–
–
–
–
–
–
–
–
follicles less responsive to gonadotropins
less estrogen and progesterone secretion
uterus, vagina, and breast atrophy
intercourse becomes uncomfortable as vagina becomes thinner, less distensible, and drier
vaginal infections more common
skin becomes thinner
cholesterol levels rise increasing the risk of cardiovascular disease
bone mass declines producing increased risk for osteoporosis
blood vessels constrict and dilate in response to shifting hormone balances
hot flashes – spreading sense of heat from the abdomen to the thorax, neck, and face
• Hormone replacement therapy (HRT) – low doses of estrogen and
progesterone to relieve some of these symptoms
– risks and benefits are still being debated
Female Sexual Response
• Excitement
• Orgasm
– Not marked by ejaculation
– Rhythmic muscular contractions
• No refractory period