Diagnosis, Prevention and Treatment of CA-UTI in Adults
advertisement

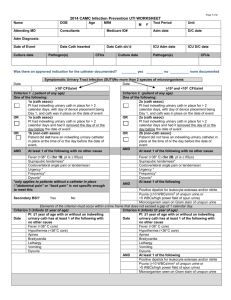
Diagnosis, Prevention and Treatment of CA-UTI in Adults Review of 2009 IDSA Clinical Practice Guidelines CID 2010;50: 625-663. Nov 09 2011 Savitri Aguiar, MD MOTIVATION UTI AS AN EXPLANATION FOR A.M.S IN OLDER ADULT WITH A CATH UTI IS THE MOST COMMON ILNESS IN ADULTS > 65 YO (1) Incidence > 80 yo: 10% in women and 5.3% in men. ASB: 6 to 16% of women in the community and 25-54% in nursing homes (men is about half of those percentages) (2) with caths: 85-100% of ASB U.S. hospitals have not widely implemented strategies to reduce H.A. UTI (3) CMS will no longer pay for it MOTIVATION HOW DO WE GO FROM UTI TO AMS? -pro inflammatory cytokines (ILs and TNF alpha) may play a role in pathogenesis of delirium -hypoperfusion Do we overdiagnosis CA-UTI? - excessive ATBC’s Not to do something is a much harder thing to do in our culture INTRODUCTION CA-UTI in adults ≥ 18 yo Short-term cath (<30 days) Long-term cath (≥ 30 days) Indwelling / intermittent / condom cath NOT COVERED: single in/out cath for diagnostic purposes; complicated urologic procedures (i.e., ureteral stents, nephrostomy tubes); or fungal UTI. INTRODUCTION CA-Bacteriuria is the most common hospital acquired infection in the world. Largely due to too many Foley's. 40% of hosp acquired infections in U.S. (NNIS 1992-2004) 15% of H.A. bacteremia (mainly Gram Neg) attributable to CA-B; however only 1-4% of CA-B evolves to bacteremia. Association with increased mortality (NEJM 1982;307:637-642); confounding? Most of the 900,000 yearly nosocomial bacteriuria have a cath 15-25% of patients in a general hosp will have some cath days Incidence of CA-B: 3%-8% per day; BY ONE MONTH: 100% bacteriuric < 25% of CA-B develop UTI symptoms. Catheter literature nomenclature 1)CA-ASB 2)CA-B (asymp or non): predominantly CA-ASB Very few are reports on CA-UTI Therefore, most recommendations in these guidelines refer to CA-B. Because this is the only or predominant outcome measure DIAGNOSIS (=DEFINITIONS) Cath (indwelling urethral, indwelling suprapubic or intermittent cath) CA-UTI: signs / symptoms compatible w/ UTI no other identifiable source of infection ≥103 CFU/ml of ≥ 1 bacterial species in a single cath-urine specimen or in a midstream voided urine from a patient whose urethral, suprapubic or condom cath was removed within 48 h not clear the number of CFU for men with condom cath (to diagnose UTI) DIAGNOSIS (=DEFINITIONS) CA-ASB: Same caths: ≥ 105 CFU/ml of ≥ 1 bacterial species in a single cath urine specimen in a patient WITHOUT symptoms compatible with UTI Condom cath (freshly applied): same 105 CFU SHOULD NOT BE SCREENED FOR, EXCEPT IN RESEARCH AND PREGNANT WOMEN VERY IMPORTANT Pyuria (≥ 10 WBC/mm3 of uncentrifuged urine) is NOT diagnostic of CA-B or CA-UTI presence, absence or its degree is of NO USE to differentiate CA-ASB from UTI pyuria plus CA-ASB: NOT and indication for ATBC's absence suggests another diagnosis other than CA-UTI presence or absence of odorous / cloudy urine alone should not be used to differentiate CA-ASB from CA-UTI: DO NOT CULTURE; DO NOT RX ATBC'S. Leukocyte esterase and nitrites: NO VALUE either CORE OF THE PROBLEM SIGNS / SYMPTOMS OF UTI flank pain, CVA tenderness, acute hematuria, pelvic discomfort (rare) and, if cath was removed: dysuria, urgency, frequency, suprapubic pain / tenderness CORE OF THE PROBLEM SIGNS / SYMPTOMS OF UTI spinal cord injury: increased spasticity, autonomic dysreflexia, sense of unease (SUBJECTIVE) new onset fever, rigors, A.M.S, malaise, lethargy WITHOUT OTHER IDENTIFIABLE CAUSE EXCLUSION DIAGNOSIS!!!!!!!!!!! CLINICAL DILEMA: what defines symptomatic in frail, often cognitively impaired seniors? PREVENTION=REDUCE USE OF URIN. CATHETERIZATION using clear indications (absent in up to 50% of the times) removing cath ASAP The strategies to do the above have more impact on the incidence of CA-ASB and CA-UTI than anything else!!! Implementing those should be a priority for all health care facilities Acceptable Indications for Indwelling Urinary Catheter Use. Hooton T M et al. Clin Infect Dis. 2010;50:625-663 © 2010 by the Infectious Diseases Society of America PREVENTION: LIMIT UNNECESSARY CATHS No cath for urinary incontinence, except per patient request (I’d add informed consent with risks of infection) Institution must develop a list of appropriate indications Institution should require a physician order before indwelling cath is placed Institution should consider portable bladder scanners to determine whether cath is necessary for post-op patients PREVENTION: DISCONTINUE CATH Remove indwelling cath ASAP Institution should consider NURSE based or ELECTRONIC based physician reminder systems to reduce inappropriate caths Institution to consider AUTOMATIC STOP orders to reduce inappropriate urine caths PREVENTION: INFECTION PREVENTION: develop, maintain and enforce policies and procedures for recommended cath insertion indications, insertion and maintenance techniques and replacement indications may consider feedback of CA-B rates to providers on a regular basis to reduce risk of CA-B (unclear if this will drop CA-UTI) place patients with urinary caths in different rooms? PREVENTION: UNCERTAINTIES: ALTERNATIVES TO INDWELLING CATHS 1)Condom / 2)intermittent / 3)suprapubic cath: insufficient definitive data to support one over another INSERTION TECHNIQUES: INTERMITTENT: clean is enough; multiple use caths are ok INDWELLING: aseptic technique is required PREVENTION:TECHNIQUES AFTER INSERTION CLOSED CATHETER SYSTEM: keep it closed and low ANTIMICROBIAL COATED CATHS (silver alloy or ATBC): may be considered: insufficient data to support recommendation PROPH ATBCS: NO! NO! PROPH WITH METHENAMINE SALTS: NO! If done, the goal is to reduce urine pH < 6; consider in women after GYN surgery who are catheterized for no more than 1 week PROPH WITH CRANBERRY PRODUCTS: NO ENHANCED MEATAL CARE: NO PROOF IT WORKS! (povidone-iodine, silver sulfadiazine, polyatbc ointment or cream, soap / water) CATHETER IRRIGATION W/ SALINE AND OR ATBCS: may be considered only in selected patients who undergo surgical procedures and short term cath to reduce CA-B. ATBCS IN THE DRAINAGE BAG: NO! NO! ROUTINE CATH CHANGE: unclear benefit for change Q 2-4 weeks of functional caths, even for patients who experience repeated early cath blockage from encrustation (!!!!) PROPH ATBC AT TIME OF CATH REMOVAL / REPLACEMENT: NO! TREATMENT SCREENING FOR AND RX OF CA-ASB AT CATH REMOVAL TO REDUCE CA-UTI: no strong evidence; consider in CA-ASB that persists 48 h after short-term indwelling cath. SCREENING FOR AND RX OF CA-ASB IN PATIENTS WITH CATHS TO REDUCE CA-UTI: NO! EXCEPTION: pregnant women and patients who undergo urologic procedures for which visible mucosal bleeding is anticipated. TREATMENT U/C and cath replacement before RX: YES for both: narrow ATBC based on Cx results; change the cath if placed for > 2 weeks => expedites resolution of symptoms and reduces risk of recurrent CA-ASB and UTI. Cx from new cath or voided urine if old cath can be D/C’d. Duration of RX: regardless of cath in place or not Seven days: for CA-UTI w/ prompt resolution of symptoms 10-14 days for those w/ delayed response Five days levofloxacin may be considered for not severely ill Three days ATBC regimen may be considered for women ≤ 65 yo (CA- UTI without upper U.T. symptoms) after the cath has been removed. Possible improvements Diagnosis Study our prevalence / incidence F/U on mortality Match with bacteremia Prevention What are our indications? Do we have them clearly written / available? Powerchart urinary catheter insertion orders/ automatic removal or reminder of removal Give feedback rates to providers / nurses Treatment RX duration / ATBC of choice Quality improvement project 5-W Infection control (use their data collection tool) Implement intervention (Published indications? Powerplan? Auto-D/C Cath?) Analyze data Publish paper and try to disseminate to the medical wards REFERENCES 1)Epidemiology of urinary tract infections: transmission and risk factors, incidence, and costs. Foxman B, Brown P. Infect Dis Clin North Am. 2003;17(2):227. 2) Juthani-Mehta M. Asymptomatic bacteriuria and urinary tract infection in older adults. Clin Geriatr Med 2007; 23:585. 3)Saint S et al. Preventing H.A. UTI in the USA: a national study. CID 2008; 46:243-50. UPTODATE IDSA Guidelines.