Urinary Tract Infections:
advertisement

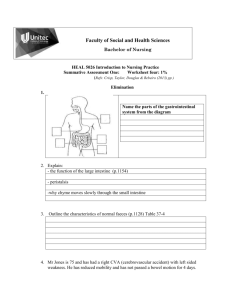
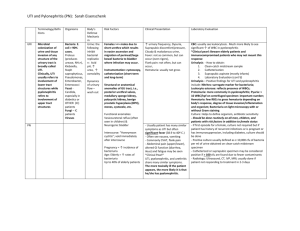
Urinary Tract Infections Meral Sönmezoğlu Division of Infectious Diseases Yeditepe University Hospital Learning objectives UTI’s Epidemiology Pathogenesis Risk Factors Types of cystitis Evaluation Therapy Urinary System Based on: Mader, S., Inquiry Into Life, McGraw-Hill Anatomy of the Kidney Based on: Mader, S., Inquiry Into Life, McGraw-Hill Nephron Based on: Mader, S., Inquiry Into Life, McGraw-Hill Urine moves from the collecting ducts through the kidney pelvis to the ureter Based on: Mader, S., Inquiry Into Life, McGraw-Hill Urine moves from the kidneys, through the ureters to the bladder and finally through the urethra Based on: Mader, S., Inquiry Into Life, McGraw-Hill Epidemiology UTI’s UTIs are the second most common cause for prescription of antibiotics Most infections are limited to the lower urinary tract 30 times more likely in young women than young men Incidence in men rises dramatically after age 50 Women may have more UTIs than men because: 1) they have a shorter urethra, allowing quicker access to the bladder 2) the urethral opening is nearer the anus 3) intercourse may result in UTIs in women Based on: Harvard Medical School Family Health Guide Relative frequency of nosocomial (hospital-acquired) infections Site % of total Urinary tract 34 Surgical wound 17 Bloodstream 14 Pneumonia 13 Other 21 Pathogenesis UTI’s Bacteria travel: Ascending route via the urethra 95% Hematogenous (kidney-> bladder) Endocarditis Tuberculosis Direct (connection bowelbladder) Bacterial factors Inoculum size Virulence Adherence E. coli adhere to urothelial cells Proteus, Providencia adhere to lumen of catheter material Virulence Host factors Infection No infection Host defense mechanisms Mechanical Interference Normal bacteria flora (meatus) Chemical Dilution and flow of urine Length of urethra Osmolality and pH of urine Prostatic fluid Anti-adherence mechanisms in bladder Urinary immunoglobulins Mucosal antibacterial activity Risk factors UTI’s (I) Alteration/introduction of bacteria Antibiotics Spermicides Vaginal atrophy (age) Sex Insertive rectal sex Inserting toys Patient education: Void after intercourse, Proper wiping, front to back once Risk factors UTI’s (II) Urinary stasis Neurologic bladder Reflux into the ureters (pregnancy) Obstruction Diabetes mellitus Congenital anatomical abnormalities Prostate hypertrophy (age) Stones, tumor Glycosuria Foreign materials Stones Stents Catheters Pathogenesis of cystitis UTI’s Uncomplicated cystitis Complicated UTI’s Risk factors When to look for causes Interpret UA, dipstick, urine cx Asymptomatic bacteriuria Catheter-related issues Prudent use of antibiotics Types of urinary tract problems Asymptomatic bacteriuria Dysuria Cystitis Complicated UTI Acute uncomplicated cystitis Recurrent cystitis Pyelonephritis UTI’s in men, pregnant women, children Prostatitis Other Catheter associated UTI Candida in urine Sterile pyuria Definitions (I) Asymptomatic bacteriuria: isolation of a specified quantitative count of bacteria in an appropriately collected urine specimen obtained from a person without symptoms or signs referable to urinary infection Acute uncomplicated UTI (cystitis): symptomatic bladder infection characterized by frequency, urgency, dysuria or suprapubic pain in a woman with a normal genitourinary tract Definitions (II) Acute nonobstructive pyelonephritis: renal infection characterized by costovertebral angle pain often with fever sometimes with bacteraemia Complicated urinary tract infection: may involve the bladder or kidneys symptomatic urinary infection in individuals with functional or structural abnormalities of the urinary tract What can the laboratory do with a sample of urine? Urinalysis Microscopy Dipstick Quantitative culture Specialized cultures (TB, fungi) Urine dipstick Leukocyte esterase: rapid screening test for detecting pyuria Patients with symptoms and negative LE should have a urine microscopic examination for pyuria Urinary nitrite Nitrite is formed when bacteria reduce the nitrate that is normally found in the urine False negatives common, but false positives are rare The whys and how's of urinary tract organism quantification Bladder urine is sterile Distal urethra is not sterile How can we differentiate: bladder bacteria (pathogens) from urethral bacteria (contaminants)? What is a positive culture? Classic definition: > 105 cfu/ml With symptoms: > 103 cfu/ml 90% chance of actual infection Etiologic agents Community acquired-UTI E. coli (25%) Enterococcus spp (16%) P. aeruginosa (11%) Candida spp. (8%) K. pneumoniae (7%) Enterobacter spp. (5%) Proteus mirabilis (5%) Community-Acquired UTI E.coli S.epi & gm - enterics Enterococcus Proteus K.pneumoniae S.saprophyticus Microscopy A true UTI is accompanied by Pyuria Lack of epithelial cells >5/ mm³ indicates contamination Only one bacterial species (monoculture) >10 leukocytes/mm³ of uncentrifuged urine unless catheter in place >105 cfu Do not culture urine unless Indicated AND Abnormal UA Dysuria Dysuria can be caused by Vaginitis -no pyuria and <102 cfu/ml) Candida Trichomonas atrophy of vaginal tissues Urethritis –pyuria and <102 cfu/ml, gradual Chlamydia Neisseria gonorrhoeae Cystitis – pyuria and >103 cfu/ml, onset abrupt Asymptomatic bacteriuria why screen? Screening of asymptomatic people for bacteriuria is only appropriate to prevent adverse events In pregnancy (Gp B strep) Prior to urologic surgery Undesirable outcomes associated with therapy: Antimicrobial resistance Adverse drug effects Costs C. difficile associated disease Asymptomatic bacteriuriaHealthy, premenopausal women Bacteriuria increases risk for symptomatic UTI Not associated adverse outcomes Treatment of asymptomatic bacteriuria neither decreases frequency of symptomatic infection nor prevents further episodes of asymptomatic bacteriuria Screening for and treatment of asymptomatic bacteriuria is not indicated Asymptomatic bacteriuria - Pregnant women 20-30 fold increased risk of pyelonephritis during pregnancy More likely to experience premature delivery and to have low birthweight infants Treatment of bacteriuria decreases above risks Screen for bacteriuria by urine culture at least once in early pregnancy and treat for 3-7 days if positive Asymptomatic bacteriuria Elderly institutionalized subjects No decrease in rate of symptomatic infection improvement in survival chronic GU symptoms with Abx therapy Screening and treatment of asymptomatic bacteriuria in elderly institutionalized residents of long-term care facilities not recommended Asymptomatic bacteriuria – Patients with indwelling catheters Antimicrobial therapy not associated with decrease in rate of symptomatic infection High incidence of recurrence, usually with more resistant organisms Asymptomatic bacteriuria or funguria should not be screened for or treated in patients with indwelling urethral catheter Acute uncomplicated UTI (cystitis) Symptoms Dysuria, frequency, urgency Initial and terminal hematuria Suprapubic discomfort Low-grade fever may occur Diagnosis Dipstick or microscopy Culture Exclude other causes STD Vaginitis Nitrite positive Positive LE/WBC (>10 WBC’s) Not routinely necessary Carefully obtained clean catch 104-5 cfu/ml 1 bacterial species only Acute uncomplicated UTI (cystitis) Bacteria E. coli in 80-90% Staph. saprophyticus in 5-15% Proteus and Klebsiella species Adult female No anatomic/functional/immunologic abnormalities Non-pregnant Acute uncomplicated UTI Therapy Resistance varies 30% resistant to amoxicillin 1-20% to nitrofurantoin 5-15% to TMP-SMX Recommend: course of TMP-SMX as first choice (3 days) Fluoroquinolone as second (3 days) Nitrofurantoin (7 days) Does not penetrate in kidney Recurrent Cystitis Relapse: same organism in <2 weeks Suggests uneradicated focus Abx resistance Non compliance Reinfection - may be same or different organism: Interval >2 weeks Hygiene/wiping Post-coital Vaginal atrophy Post-void residual (prolapse) Management: Recurrent UTI Patient-initiated therapy: multiple 3 day courses of antibiotics to be started by the patient at onset of sx Post-menopausal women: symptomatic relief with topical estrogen -helps to “normalize” protective flora Further Studies / Referral Renal US- least invasive VCUG- best study to detect vesicourethral reflux CT / MRI IVP According to Fihn, NEJM (July 17,2003), imaging studies are not necessary unless there are other sx ie. hematuria. Complicated UTI (Everyone/everything else) Child, male, pregnant female Kidney involvement, 2nd bacteraemia Abnormality Anatomy, function, immunology Urologic procedure Catheterization Unusual or resistant organisms Acute pyelonephritis Usually E. coli Obtain urine culture If hospitalized obtain blood cultures Mostly an ascending infection Disease severity Mild Life threatening urosepsis Acute pyelonephritis -Therapy Mild to moderately ill patients Severely ill patients TMP-SMX (bactrim) amox/clav, cefuroxime or fluoroquinolone Patients usually improve in 48-72 hours Treat for 1-2 weeks Ampicillin + aminoglycoside IV therapy until patient afebrile for 48-72 hours Treat for 2 weeks If fever persists and all children and men: Renal US, CT or MR ± IVP Look for perinephric abscess Exclude urinary obstruction Cystitis in males Young men (rare in men under 50) Older men Calculi Enlarged prostate (obstruction) Chronic prostatitis Organisms differ Anatomic abnormalities Anal insertive sex, toys E. coli accounts for 40-50% Proteus and Providencia species accounting for next most frequent cause Most common cause of relapsing UTI is chronic bacterial prostatitis UTI’s in males (other than pyelonephritis) Urethritis (STI’s) Gonorrhea Chlamydia Ureoplasma Prostatitis Same organisms as above For older males (in addition to above): Gram negative rods Enterococci Acute prostatitis Fever, chills Dysuria, pain Marked local tenderness Excellent penetration by most antibiotic classes-easily cured Complications Prostatic abscess Chronic prostatitis Chronic prostatitis Chronic pain Dysuria Recurrent “UTI’s” – same organism Poor antibiotic penetration-difficult to treat Biofilm Calculi Preferred agents Fluoroquinolones TMP-SMX Role of the catheter in UTI Conduit Internal lumen Migration of bacteria along external surface Foreign body Biofilm formation Protects from host defense Protects from antibiotics Incomplete emptying Complications in catheterized patients Bacteriuria is universal Providencia stuartii (24%) Proteus (15%) E. coli (14%) Pseudomonas (12%) Pyuria is common from bladder irritation Cannot diagnose UTI unless: Fever (cured often with cath change alone) Pyelonephritis Prevention of catheter-related UTI’s Avoid catheterization Avoid extrinsic contamination of system Early removal Replace catheter frequently Intermittent cath far superior Closed catheter drainage Unproven benefit Antiseptics in drainage bag Antibiotics will decrease bacteriuria and then lead to recolonization with resistant organisms Candida in the urine Most candiduria occurs in patients with indwelling catheters Risk factor is prior antibiotics Removal of the catheter results in clearance of most candiduria Oral fluconazole or amphotericin B bladder irrigation eliminate candiduria short-term no more effective than no therapy Only indications for treatment of asymptomatic candiduria Urinary tract obstruction (fungus ball) Neutropenia Renal transplant recipient Urologic procedure in next 48-72 hours Sterile pyuria 1. Antibiotic pre-treatment kills bacteria (Culture negative) 2. Organisms that don’t grow on commonly used culture media Tuberculosis Fungi Genitourinary tuberculosis From: Johnson and Feehally, Comprehensive Clinical Nephrology, 2000, Elsevier Genitourinary tuberculosis Hematogenous seeding can occur in cortex and forms granuloma Seeding in the medulla In both sites Granulomas form Caseation Erosion into collecting system Further spread to ureters, bladder, prostate… Health Education Correct technique for obtaining clean catch! Avoid bladder irritants: caffeine, carbonated beverages, aspartame, ETOH, spicy foods. Hygiene: wipe front to back. Avoid bubble baths, scented products (pads, tampons, soaps, feminine sprays). Health Education Showers instead of baths. Void at regular intervals, do not hold it all day. If sexually active, void after intercourse. Push fluids. Avoid constipation. Take all of meds!!! White toilet tissue, white cotton underwear.