File
advertisement
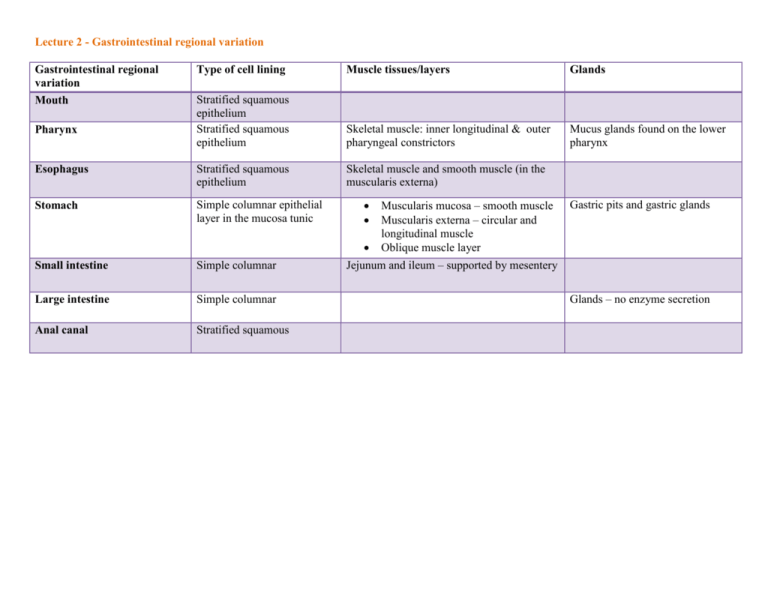
Lecture 2 - Gastrointestinal regional variation Gastrointestinal regional variation Mouth Type of cell lining Muscle tissues/layers Glands Stratified squamous epithelium Stratified squamous epithelium Skeletal muscle: inner longitudinal & outer pharyngeal constrictors Mucus glands found on the lower pharynx Esophagus Stratified squamous epithelium Skeletal muscle and smooth muscle (in the muscularis externa) Stomach Simple columnar epithelial layer in the mucosa tunic Small intestine Simple columnar Large intestine Simple columnar Anal canal Stratified squamous Pharynx Muscularis mucosa – smooth muscle Muscularis externa – circular and longitudinal muscle Oblique muscle layer Jejunum and ileum – supported by mesentery Gastric pits and gastric glands Glands – no enzyme secretion Lecture 3 – gastrointestinal regulations Stimulation Type of stimulation Neural Source Function of source Enhance function Inhibit function Interstitial cells of Cajal – pacemakers cells located on muscularis externa Stretch, acetylcholine, PNS stimulate spikes to occur on crest of slow wave AP generated Norepinephrine, SNS Extrinsic activity: conditioned stimuli Neural Sight, smell, thought of food Neurotransmitters (nts) Neural Circulating hormones: extrinsic or intrinsic Local factors: intrinsic Hormonal Neurotransmitters from CNS or ENS Endocrine Pacemakers cells deliver info form enteric neurons to smooth muscle cells generate slow wave in the stomach Involve CNS to stimulate salivary centers and vagal nuclei in the medulla Act on cells at the synapses to regulate cell activity Paracrine Paracrine cells Intrinsic activity: mediated by local enteric nervous system plexuses Sources of stimulation CNS Neuroregulation Autonomic nervous system - SNS CNS Autonomic nervous system – PNS AP release neurotransmitters Act on cells near the site of paracrine release Components and functions Preganglionic nerves: release Ach to bind w/ nicotinic receptors on postganglionic nerves Postganglionic nerves: release norepinephrine (NE) Preganglionic: comprised of vagus nerve and pelvic nerves; release Ach to activate nicotinic receptors on enteric neurons Postganglionic: release Ach which activate muscarinic receptors in gut; may also release neuropeptides as neurotransmitters ENS GI nerve supply: myenteric plexus Plexus regulates motility ENS GI nerve supply: submucosal plexus Plexus controls secretion, blood flow and absorption ENS Neurotransmitters Ach: stimulate contraction of smooth muscle, secretion of salivary gland, stomach, pancrease NE – inhibit contractions of smooth muscle, stimulate contraction of some sphincters Lecture 4 – Gastrointestinal motility Factors affecting GI motility Gastrin Function Increase frequency and velocity of gastric slow wave Stimulate antrum motility (contraction) Raise LES pressure contraction Increase emptying into duodenum Increase/decrease emptying Increase Volume of chyme in the stomach Increasing volume cause distention and stimulate mechanoreceptors enhanced motility via intrinsic nerve Increase Volume/chemical composition of chyme in the duodenum Cause neural response: enterogastric reflex inhibits gastric emptying and stimulate contraction of pyloric sphincter Hormonal response: stimulate release of enterogastrone Enterogastrones inhibits emptying pH Low pH Decrease Osmolality Isotonic osmolality of chyme Increase Particle size Large size Decrease Caloric load of content High load Decrease Lecture 5 - Secretion Part 1 Control of extrinsic salivary glands Cl-/HCO3- symporter Location Process Gain/Loss On luminal/apical membrane of acinar cell Losing Cl- and HCO3- into the lumen Na+/H+ antiporter Basolateral membrane on ductal cells CL-/HCO3- antiporter Basolateral membrane on ductal cells Transport Cl- and HCO3out into the lumen of the salivary gland Na+ is reabsorb from lumen and H+ is secreted into lumen of salivary gland Cl- gets reabsorb and HCO3- gets secreted K+/H+ antiporter Basolateral membrane of ductal cells H+ is reabsorbed and K+ is secreted into the lumen Balance H+ that was loss from the Na+/H+ antiporter Ach receptor Acinar cell Ach bind to activate 2nd messenger system to activate protein kinase to activate release of zymogen granules Function Losing H+ Gaining Na+ Balance Cl- that was lost from acinar cells; increase the loss of HCO3- HCO3- in salivary gland contribute to buffer against acid for reflux and dental caries Anticholinergic drugs: scopolamine, benztropine, ipratropium will inhibit Ach receptor and cause dry mouth Stomach mucosa epithelial cells Surface mucosal cells (all over the stomach) Secretion/components Neck mucosal cells (all over the stomach) Parietal cells (at the fundus) Mucus Parietal cells (at the fundus) HCl Parietal cells H+/K+ ATPase (protein pump protein) on luminal/apical membrane HCO3-/CL- antiporter on Basolateral membrane Parietal cells Parietal cells Mucus (mucin) and HCO3- Intrinsic factor (glycoprotein) Ach (M3 muscarinic) receptor on basolateral membrane Function of secretion/component Maintain pH 7 on surface epithelial cell; prevent gastric mucosa from stomach acid damage Form protective flexible gel against stomach acid Form complex with Vit B12 so that Vit B12 can be absorb in the ileum Produce stomach pH of 1-3 Activate pepsinogen Kill most bacteria Denature protein Destroy plant cell wall Break down animal connective tissue (CT) Inactivate salivary amylase Transport H+ to stomach lumen and bring in K+ into the cell HCO3- transported out to the blood and Cl- is brought inside Ach bind to receptor which cause an increase in IP3 increase Ca+ level increase protein kinase activity promote more proton pump (H+/K+ ATPase) activity Complications H-pyloric can producing urease to hydrolyze urea to form NH4+ and HCO3-; NH4+ can damage these surface cells gastric ulcers Vit B12 is needed for RBC production; w/out its absorption RBC cannot be produce pernicious anemia Increasing amount of H+ in lumen Cl- diffuse across cell to the lumen where it can bind w/ H+ HCl Increase in HCl production Treatment of the complication H-pyloric tx: 2 antibiotics, bismuth containing compound Ulcer: H2-receptor blocker or PPI Parietal cells Gastrin/CCK-B receptor on basolateral membrane Enterochromaffin-like (ECL) mast cells (located in the gastric mucosa at the fundus) Histamine (paracrine) Chief cells (at the fundus) Pepsinogen (precursor enzyme) Chief cells Gastric lipase Gastrin bind to receptor increase IP3 increase Ca+ increase protein kinase promote more proton pump (H+/K+ ATPase) activity Histamine will bind to H2 receptor on basolateral membrane of parietal cell increase 2nd messenger cAMP increase protein kinase increase HCl Increase in HCl production Histamine is released as a result of inflammation; histamine stimulate more acid production not good for the already damaged stomach lining gastric ulcer Tx of gastric ulcer PPI: permanent inhibition of H+/K+ ATPase activity Anticholinergic: block Ach from binding to receptor H2-receptor blocker Activated to become pepsin in the presence of acid at pH of 2. Pepsin starts protein digestion. Active at pH of 3. Activated form will digest triglycerides Pyloric enteroendocrine cells G cells (at the antrum) Secretion Gastrin (hormone) D cells (at the antrum) Somatostatin (hormone) Function of secretion Stimulate acid release by parietal cell Stimulate pepsinogen release by chief cells Stimulate stomach mucosal growth Stimulate gastric contractions that mix and stir the gastric contents Stimulate ECL release of histamine Inhibit gastric release from G cells Inhibit histamine release from ECL cells Bind to receptor on parietal cell and inhibit acid secretion Lecture 6 - Secretion Part 2 Pancreatic cells Acinar cell Secretion Enzyme Acinar cell Pancreatic amylase Acinar cell Acinar cell Ductal cells Function of secretion Store enzyme in zymogen granules until they are released via exocytosis to aid in digestion For starch digestion Site of release Site of action Duodenum Small intestine Tyypsine, chymotripsine and carboxypeptidase For protein digestion Duodenum Small intestine - duodenum Pancreatic lipase (lipolytic enzyme) For fat digestion Duodenum Small intestine - duodenum Water and electrolyte HCO3- HCO3- will neutralize excess stomach acid in the duodenum Duodenum Duodenal enteroendocrine cells Secretion Stimulus for secretion (enterogastrone) CCK Fatty chyme that is (cholecystokinin) partially digested Duodenal enteroendocrine cells Secretin Low pH of less than 4.5 Duodenal enteroendocrine cells Cells of the duodenum & jejunum GIP (gastric inhibitory peptide) Motilin Fatty acid, amino acid, glucose When fasting Function of secretion Site of action Tell the pancrease to produce more enzymes Dominant regulator of inhibiting gastric emptying Stimulate gall bladder and pancreatic functions Stimulate constriction of pyloric sphincter Tell pancrease to produce more HCO3 Stimulate liver to release more HCO3- into the bile Inhibit gastric acid secretion and emptying Stimulate release of water and HCO3- into bile Stimulate secretion of insulin Inhibit gastric emptying and gastric secretion of HCl Stimulate motility (contraction) of the stomach and small intestine to prevent bacterial overgrowth Gastrin/CCK receptor on acinar cells in the pancrease more enzyme production Bind to gallbladder contraction to release bile Bind to Oddi’s sphincter relax the sphincter to allow bile into duodenum so bile can emulsify fat Ductal cells of the pancrease Liver cells Absorptive epithelia cells transporter (on the villi of Sm. Intestine) Location Function Na+/K+ ATPase Brush border Pump Na+ out of the cell and bring in K+ using ATP to set up the gradient for Na+ wanting to come into the cell SGLT 1 (sodium glucose galactose cross) co-transporter Luminal side of brush border cells Transport these molecules against their concentration gradient into the cell by using sodium’s energy GLUT 5 (fructose) Luminal side of brush border cells Brings fructose into the cell GLUT 2 Basolateral membrane of brush border cells Helps all monosaccharide get out from the cell and into the blood