The Use of Cefoxitin for the Determination of Methicillin Resistance
advertisement

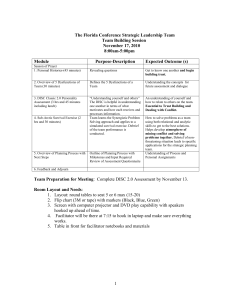
The Use of Cefoxitin for the Determination of Methicillin Resistance in Staphylococci John D. Perry Microbiology Department Freeman Hospital Newcastle upon Tyne BSAC Working Party recommendations for detection of methicillin resistance (2004): Inoculum: Semi confluent Medium: Columbia agar plus 2 % salt. Incubation conditions: 30°C Discs: Oxacillin 1 µg or methicillin 5 µg BSAC Working Party recommendations for detection of methicillin resistance (2004) Disadvantages: A separate medium (at a different temperature) is required to that used for testing other anti-staphylococcal agents. False resistance may be encountered due to hyper-production of ß-lactamase False susceptibility may be encountered with strains that are highly sensitive to salt. Felten et al: Evaluation of three techniques for detection of low-level methicillin-resistant Staphylococcus aureus (MRSA): a disk diffusion method with cefoxitin and moxalactam, the Vitek 2 system, and the MRSA-screen latex agglutination test. J Clin Microbiol. 2002 Aug;40(8):2766-71. Felten et al. examined: 69 mecA-negative S. aureus strains and 83 mecA positive S. aureus strains (MRSA) including 69 with heterogeneous resistance. Susceptibility to cefoxitin 30 µg discs was determined on Mueller-Hinton agar at 37°C using high and low inocula. Oxacillin disc testing was performed in parallel using CLSI and CASFM methodologies. Felten et al. (continued): Results: The cefoxitin 30 µg disc test showed 100 % specificity and 100 % sensitivity for detection of MRSA. Interpretive criteria were: Zone diameter < 27 mm = MRSA. Disc testing using oxacillin showed a sensitivity of 95.2 – 96.4 % depending on the inoculum used. Specificity was 100 %. Significance of the study by Felten et al. The results suggested that cefoxitin was potentially more sensitive that oxacillin for detection of methicillin resistance. Also: Reliable results were obtained at 37°C, without the addition of salt, without a specialised medium and using two different inocula. Evaluation of a cefoxitin 30 µg disc on IsoSensitest agar for detection of methicillinresistant Staphylococcus aureus. Skov et al. J Antimicrob Chemother. 2003 Aug;52(2):204-7. Skov et al. examined a ‘difficult’ collection of 457 S. aureus strains including: 190 MRSA (including several defined PFGE types and a number of ‘low level resistant’ strains). All MRSA were defined as mecA positive using PCR. Skov et al. (continued). Methods: All strains were tested using: Isosensitest agar A semi-confluent inoculum 30 µg cefoxitin disc Overnight incubation at 35-36°C. Skov et al. (continued). SRGA Method tested in parallel: All strains were tested using: Isosensitest agar plus 5% horse blood. A confluent inoculum 1 µg oxacillin disc 24 h incubation at 30°C. Skov et al. (continued). Results: Using a zone diameter of < 29 mm to define resistance, the cefoxitin disc susceptibility test showed a sensitivity of 100 % and a specificity of 99 %. The SRGA method using oxacillin (resistant < 12 mm) showed a sensitivity of 78 % and a specificity of 99 %. Zone diameters of an oxacillin 1 µg disc the SRGA method. A vertical line marks the present interpretive zone diameter for susceptibility. Black bars, mecA positive; white bars, mecA negative. Zone diameters of a cefoxitin 30 µg disc against 457 S. aureus A vertical line marks the proposed interpretive zone diameter. Black bars, mecA positive; white bars, mecA negative. Significance of the study by Skov et al. The results show that susceptibility testing with cefoxitin is much superior to the standard SRGA method using oxacillin. Also: Reliable results were obtained at 35-36°C using Isosensitest agar with a semi-confluent inoculum. These conditions are those recommended by the BSAC Working Party for routine susceptibility testing. Significance of the study by Skov et al. Disadvantages of the cefoxitin disc susceptibility test: Marginal difference in zone diameter between methicillin susceptible strains and some MRSA strains. Accurate zone measurement is required. Large zone sizes are produced by sensitive strains that could potentially interfere with other zones if multiple discs are tested on the same plate. Evaluation of cefoxitin 5 and 10 µg discs for the detection of methicillin resistance in staphylococci (Skov et al. Journal of Antimicrobial Chemotherapy 2005 55(2):157-161) Skov et al. examined a collection of 641 S. aureus strains including 261 mecA negative and 380 mecA positive. Test conditions: Isosensitest agar and Mueller-Hinton agar. 10 µg and 5 µg cefoxitin discs. Semi-confluent inoculum. Incubation at 35 – 37°C SRGA method using oxacillin also performed. Results: Interpretive zone diameters for Staphylococcus aureus for cefoxitin 5 and 10 µg discs on ISA (Oxoid) and MH (BBL) and the corresponding sensitivity and specificity Agar Disc Interpretive zone diameter (mm) Sensitivity (%) Specificity (% ISA cefoxitin 5 µg R < 14 99.5 98.1 ISA cefoxitin 10 µg R < 22 99.5 98.1 MH cefoxitin 5 µg R < 12 99.7 98.1 MH cefoxitin 10 µg R < 18 99.5 98.9 ISA oxacillin 1 µg 82.3 100 R < 12 Figure 1. Zone diameters against 641 S. aureus using a semi-confluent inoculum and overnight incubation in ambient air at 35–37°C. A vertical line marks the proposed interpretive zone diameter. Black bars, mecA-positive; grey bars, mecA-negative; (a) 5 µg cefoxitin disc on Iso-Sensitest agar; (b) 10 µg cefoxitin disc on Iso-Sensitest agar; (c) 5 µg cefoxitin disc on Mueller–Hinton agar; (d) 10 µg cefoxitin disc on Mueller–Hinton agar. n, no. of isolates with 6 mm zone. Conclusions from the study by Skov et al. Cefoxitin 10 µg and 5 µg discs were both successful for detection of MRSA. Smaller zone diameters were produced with a high proportion of MRSA giving no zone of inhibition. Two mecA-positive strains isolated from Norway could not be detected by any of the test methods (including the oxacillin test). There remains a marginal difference in zone diameter between some strains of MRSA and MSSA. Evaluation of a 10 µg cefoxitin disc for the detection of methicillin resistance in Staphylococcus aureus by BSAC methodology. Andrews et al. J Antimicrob Chemother. 2005 Sep;56(3):599-600. In a study organised by the BSAC Working Party, 200 consecutive isolates of S. aureus (duplicates from the same patient were excluded) were tested in each of 5 different laboratories: •City Hospital, Birmingham. •St. Thomas’s Hospital, London •Addenbrookes Hospital, Cambridge •Royal Infirmary, Glasgow •Freeman Hospital, Newcastle upon Tyne Andrews et al. (continued): Test conditions: Isosensitest agar (Oxoid): depth 4 mm. Semi-confluent growth. 10 µg cefoxitin disc. Incubation at 34 – 36 °C for 18 – 20 hours. All strains were also tested for the presence of the mecA gene by PCR. Andrews et al. (continued): Results: •328 strains of 1000 tested were MRSA as defined by PCR. •224 MRSA strains (68 %) showed no zone of inhibition with a 10 µg cefoxitin disc. •104 MRSA strains produced zone diameters between 7–19 mm. •A zone diameter breakpoint of 22 mm was chosen to distinguish between MRSA and MSSA. •Using this breakpoint 2 strains of MSSA (out of 672) were falsely classified as methicillin resistant. Zone diameter distribution for 1000 isolates of S. aureus. A zone diameter breakpoint of 22 mm was chosen to interpret susceptibility. Black bars, mecA negative; grey bars, mecA positive. Conclusions from the study by Andrews et al. As a result of this study (and other published work) the BSAC now recommends the use of cefoxitin as an option for the determination of methicillin resistance in S. aureus. Optimal test conditions: Isosensitest agar, Cefoxitin 10 µg discs, semi-confluent inoculum, overnight incubation at 35°C. Interpretive criteria: < 22 mm = Resistant. Coagulase-negative staphylococci (CNS) and cefoxitin. The method now recommended by the BSAC for S. aureus was employed by Skov et al. (2005) to attempt to detect methicillin resistance in 344 strains of CNS: 132 were mecA negative and 212 were mecA positive. (Skov et al. Journal of Antimicrobial Chemotherapy 2005 55(2):157-161) Skov et al. (2005): Test conditions: (a) 5 µg cefoxitin disc on Iso-Sensitest agar; (b) 10 µg cefoxitin disc on Iso-Sensitest agar; (c) 5 µg cefoxitin disc on Mueller–Hinton agar; (d) 10 µg cefoxitin disc on Mueller–Hinton agar. Skov et al. (2005): Results None of the test conditions could reliably classify CNS as either mecA-positive or mecA-negative. A scheme was proposed by the authors for reliable interpretation of most isolates. Skov et al. (2005) – continued: J. Andrews et al. (2005) unpublished 87 Coagulase-negative staphylococci tested using BSAC recommendations for S. aureus versus cefoxitin. 51 mecA positive 36 mecA negative CNS tested on ISA cefoxitin 10 ug discs incubation @ 35'C 25 Number 20 15 Mec A -ve MecA +ve 10 5 0 6 7 8 9 10 11 12 13 14 15 16 17 18 19 20 21 22 23 24 25 26 27 28 29 30 31 32 33 34 35 36 Zone diameter (mm) Conclusions: Cefoxitin disc susceptibility testing is a reliable method for determination of methicillin resistance in S. aureus. Currently the BSAC Working Party are unable to make recommendations for determination of methicillin resistance in coagulase-negative staphylococci using cefoxitin.