EPOB 3430 1-30-03 This lecture contains the last slide from 1-28-03
advertisement

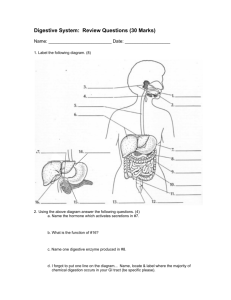
IPHY 3430 1-27-11 Control of saliva secretion Pressure and chemoreceptors in mouth--> and/or input from cerebral cortex (thoughts, smell, sight, sound)---> Salivary center in Medulla PNS Salivary glands SNS output from other centers (a. diminish blood supply, b) change composition Swallowing 1. Voluntary stage--tongue moves bolus back to back of tongue 2. Involuntary stage-- pressure receptors on tongue send signal to swallowing centers in pons and medulla--> Output of swallowing centers: 1. motor output--a) tongue moves up to hard palate to prevent food return to mouth b) uvula elevated to seal off nasal passages c.Larnyx is elevated and laryngeal muscles contract vocal folds to seal off trachea. d. Epiglottis tilted over glottis helps seal off trachea. e. After all these motor outputs occur, pharyngeal muscles contract to force bolus into esophagus. 2. Swallowing center inhibits inhalation stimulus from medulla respiratory centers Accomplishments in the mouth 1. 2. 3. 4. Increase surface area of food Moisten and lubricate food Some carbohydrate digestion Some pathogens killed Stomach 1. Store food 2. Continue carbohydrate digestion 3. Begin protein digestion 4. Moisten and mechanical breakdown 5. No absorption of food 6. Some absorption of lipid-soluble things like alcohol, aspirin, etc. In oxyntic mucosa In pyloric gland area Surface epithelial cells Gastric pit Mucosa cells Gastric gland G cells Chief cells D cells Parietal cells Enterochomaffinlike (ECL) cells Table 16-3, p. 596 Stomach secretions 1. More mucus from mucus glands 2. Parietal cell a. intrinsic factor b. HCl 3. Chief cell a. pepsinogen 4. More water Secretions and stomach contractions caused by A. Pre-meal and during eating: vagus nerve B. During eating and post meal a. Local distension, b. intrinsic nerve plexi c. Vagus (to some extent) d. G-cell (enteroendocrine cell) secretes gastrin Fig. 16-9, p. 607 Benefits of acidification of stomach contents: 1. Mechanical breakdown of food 2. Activation of pepsinogen 3. Low pH necessary for pepsin activity 4. Low pH kills many pathogens MOVEMENT OF CHYME FROM STOMACH INTO SMALL INTESTINE Factors that stimulate stomach emptying: 1. Degree of stomach distension (volume of chyme) 2. Hypotonic chyme 3. High gastrin concentration Factors in duodenum that inhibit stomach emptying (signaled to stomach by intrinsic nerve plexus and secretin and cholecystokinin) 1. High acidity of chyme 2. High fat content of chyme 3. Hypertonic chyme 4. High distension of small intestine 5. High concentration of amino acids and/or fatty acids ACCOMPLISHMENTS IN THE STOMACH 1. Some carbohydrate breakdown 2. Some protein breakdown 3. Most if not all pathogens killed 4. Chyme highly liquified SMALL INTESTINE 1. Complete enzymatic breakdown 2. Almost complete absorption of nutrients The presence of chyme on intestinal wall causes secretion of the following hormones: 1. Secretin 2. Cholecystokinin SECRETIN Target glands: 1. Stomach--inhibits emptying and secretions 2. Pancreas-causes release of aqueous NaHCO3 In small intestine NaHCO3 + HCl --> NaCl + H2CO3 --> NaCl + CO2 + H20 CHOLESYSTOKININ Target organs: a. Gall bladder--causes it to contract and release bile b. Pancreas--causes release of aqueous solution containing: 1. amylase (carbohydrate) 2. Trypsinogen (protein) 3. Chymotrypsinogen (protein) 4. Procarboxypolypeptidase (protein) 5. Lipase (fats) c. Stomach-inhibits gastric motility and secretion d. Brain--regulation of food intake WHEN PANCREATIC SECRETIONS REACH SMALL INTESTINE VIA BILE DUCT: 1. Enterokinase secreted by small intestine wall activates trypsin from trypsinogen 2. Trypsin activates chymotrypsin from chymotrypsinogen 3. Trypsin activates carboxypolypeptidase from procarboxypolypeptidase BILE Synthesized by liver, stored in gall bladder 1. 2. 3. 4. 5. 6. Water Bilirubin Cholesterol Ions (Na, K, Cl) Bile salts Lecithin