M. tuberculosis
advertisement

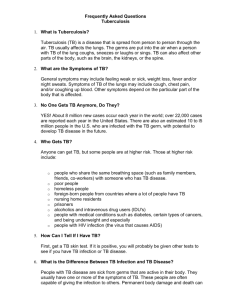
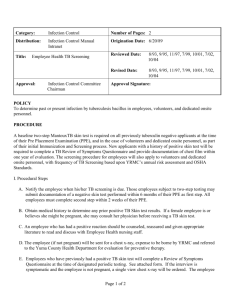
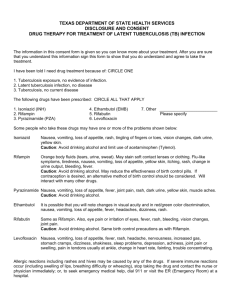
Do Now Have you heard of Tuberculosis? What is it? (If you don’t know take a guess) TUBERCULOSIS: The People’s Plague What is it? an infectious bacterial disease characterized by the growth of nodules in the tissues, especially the lungs. Commonly referred to as TB. PATHOGEN ◆ ◆ ◆ ◆ ◆ 2 – 4um in length 0.2 – 0.5um in width Facultative intracellular parasite Slow generation time (15-20 hours) Can only live in people! INNATE IMMUNE RESPONSE • When M. tuberculosis enters the body, neutrophils and macrophages provide the first line of defense • Macrophages ingest the bacilli, yet are unable to lyse or “digest” it because of M. tuberculosis’s unique waxy cellular walls (made of mycolic acid) IMMUNITY 90-95% those infected LATENT TB 5-10% of those infected ACTIVE TB • The host’s innate immune response provides the bulk of protection against TB infection • Only 1 in 10 individuals with TB will develop an active infection • Latent infections, however, are still a possibility • Likelihood of progression to an active infection from a latent infections increases with age, with positive HIV status and compromised immune systems. Latent vs. Active TB EPIDEMIOLOGY • TB disease was uncommon prior to development of major cities, where close contact and poor circulation made it easily transmitted • The CDC reports that in 2005, there were 14, 093 cases in the United States with 62% of cases amongst African Americans, Hispanics and Asians. • Globally, new cases of TB are rising in Southern and Western Africa as well as Asia. • Now highly associated with regions of high HIV positive individuals as their compromised immune systems make them more susceptible • As M. tuberculosis becomes resistant to more drugs, it is reemerging as a possibly catastrophic disease • While active disease is uncommon in most areas, 1/3 of the world population has been exposed to TB • Second most deadly infectious disease after HIV. DIAGNOSIS • • The Mantoux tuberculin skin test (TST) or the TB blood test can be used to test for M. tuberculosis infection. • Small amount of fluid containing tuberculin is injected under skin and after 48-72hrs results of indurations are analyzed • Only suggests that patient had previous exposure, not that they have an active infection Chest X-rays • • Active TB will create cavities that are visible in chest x-rays Culturing • The presence of acid-fast-bacilli on a sputum smear often indicates TB disease • Cultures are initial samples are done as final confirmation of M. tuberculosis as opposed to any other acid fast bacteria. • Incredibly slow-growing, so treatment usually begins before final confirmation from culture. SYMPTOMS • Pulmonary TB • • Paling of skin, fever, cough, difficulty breathing, night sweats, and spitting up blood Extra-pulmonary TB affects other organs such as intestines, bones, larynx and lymph nodes • • • Osteal TB - infections of the bone usually the spine resulting in deformities TB Meningitis - infection of the membrane surrounding brain and spine. Common in children Scrofula - infected lymph nodes causing visible swelling of the neck SYMPTOMS VACCINES • BCG vaccine uses attenuated bovine tuberculosis bacteria. It cannot cause disease in humans but would elicit immunity to human TB. • • • • Immunity is not permanent Ineffective with pulmonary Tb Useful in preventing disseminated disease in children Current Research • Improving BCG by experimenting on subunits from other bacteria. • • MVA85A currently in trial using VSV subunits Using live bacteria TREATMENTS • Antibiotics • • • • Streptomycin was the first antibiotic approved for treatment of TB 1949 Streptomycin was supplemented with PAS 1952 Isoniazoid found to block mycolic acid synthesis 1963 Rifampin to inhibit synthesis of bacterial RNA TREATMENT OF MULTIDRUG RESISTANT TB o When anti-biotic treatments are not fully carried out and not successfully completed drug resistant TB can develop and is becoming a serious health threat. Adherence and completion of cocktail treatments are crucial. o Many circulating strains of M. tuberculosis are resistant to Isoniazoid and Rifampin o Cocktails of second-line anti-TB drugs are often successful in the treatment of TB. Some of these include: ethambutol, rifabutin, PAS, interferon –y, and thioridazine PREVENTION o Education and DOTS campaigns o Vaccination of children o Early detection and treatment o TB drug treatment for those with confirmed latent infections oMaintenance of sanitary conditions and proper ventilation o Especially covering mouth during active infections. TB Prevention Campaigns WHO has established “DOTS” campaigns. Call for political activation to support clinical research and outreach, better diagnostic methods, standardized treatments and patient supervision and for commitment to adequate drug supply. REFERENCES • http://emedicine.medscape.com/article/226141overview#a0101 • http://textbookofbacteriology.net/tuberculosis.html • http://www.youtube.com/watch?feature=endscreen&NR= 1&v=JtyX694ubio • http://www.cdc.gov/tb/publications/slidesets/selfstudymod ules/module1/pathogenesis.htm • http://www.cdc.gov/tb/default.htm • http://www.thelancet.com/journals/lancet/article/PIIS0140 673610603935/images?imageId=gr1&sectionType=green • https://vimeo.com/13434164 • Sherman, Irwin W. Twelve Diseases That Changed Our World. Washington, DC: ASP Press, 2007 https://www.youtube.com/watch?v=I GZLkRN76Dc Do Now • Double check to make sure you have all your information for your case study. Do not go into your groups just yet. Once you are sure you have your information, take out a piece of paper, write your name and one thing you learned about TB. Once you are done, flip the paper over and wait silently.