Chemicals
advertisement

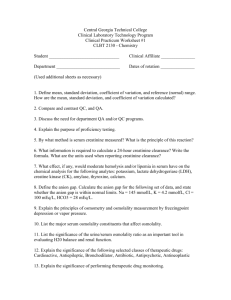
UNUVERSITY OF TABUK Faculty of Applied Medical Sciences Department of Medical Laboratory Technology LABORATORY MANUAL IN CLINICAL CHEMISTRY 1 (MLT-301) 1st semester 1434/1435 H Prepared by Dr.Walid E. Zahra; PhD Mr. Mohamed Abbas Alsubai, M.Sc., MLS Exp. No. 1 Laboratory safety Objectives 1- To use, utilize and practice all bio-safety guidelines in the biochemistry lab. 2- To realize and understand the importance of bio-safety guidelines. 3- To have the ability to explain and recognize all of hazardous labels and signs. Materials Instruments and tools: 4- Safety shower 5- Eye washer station 6- Fumes hood 7- Fire extinguisher 8- Chemicals cabinets 9- Spills kit 10- Autoclave 11- Lab coat 12- Goggles 13- 10- Glass tools/containers Disposables: 1- Latex gloves 2- Sharp containers/puncture resistant container 3- Medical wastes bags/container (yellow) 4- Needles, syringes, lancets and tubes (capped and non capped) Chemicals: 1- Acids and basis solutions 2- Several stock materials 3- Chemical Indicators 4- Solid chemicals. Background Generally in each lab there are a general lab practices for safety and safety lab guide that help all personnel to deal and contact with lab tools, equipments and practices safely in order to protect the followings: a. b. c. d. e. Workers (health care providers) Co-workers (Trainees, visitors & maid/services) Patients Environment Products/materials A. General Safety: (Wash your hand (enter/exit lab), Don’t eat, drink or smoke in the lab, wear personal protctive equipments/PPEs, mouth pipetting is PROHIBITED, emergency EXIT should be clear, wet/slipping floor is not acceptable, no visits, all benches should be received and left; cleaned, free of un-needed objects and disinfected upon starting and/finishing the work). Report any spills, leakage or/and accidents to the lab supervisor IMMEDIATELY, then record it. PPEs include: Lab coat Gloves Foot wear/medical shoes B. Chemicals Safety: (Fumes hood, chemicals cabinet, Material Safety Data Sheet/MSDS, goggles and/or masks, storage in a vertical position) Do not use or deal with any chemical that NOT labeled, unknown to you, before reading MSDS. Types of liquid chemicals: (All toxic, volatile) Flammable (Acetone, Methanol...)/away of fire source Corrosive (Strong acids and bases)/Goggles, fumes hood Carcinogenic/mutagenic (Bromo-phenol blue)/special concern Explosive/reactive (Picric acid)/separated from other chemicals Irritants (skin, eye and respiratory system), (strong acids)/goggles, fumes hood. C. Electrical safety (Be familiar with fire extinguisher, fire alarm, do not over load electrical outlets/use wet hand to handle electricity, turn off all equipments that are not in use and keep the wire hidden of benches/working area). D. Radioactive (Labelled with its sign, in its proper container, kept in a separate/specific place then collected by authorized agency). Laboratory wastes: Biological (infectious) Bio-hazardous; blood, serum, plasma, contaminated containers or curvets with one of the previous, body fluids and organic. Chemical; flammable, non-flammable, explosive and reactive. Nonmedical (Trash); non-contaminated plastics, cartons and papers. Sharp; contaminated or non contaminated (lancets, needles, broken ampoule or glasses). Radioactive; isotopes materials. Types of Fire Extinguishers A: Common materials; wood, papers & others B: Flammables liquids; gasoline & paints remover. C: Electrical fires D: Combustibles metals (industry) Carcinogenic Irritant Blood and air borne diseases: Bloodborne pathogens are type of pathogens that causing blood borne diseases (diseases arise from blood and its components and body fluids) either by direct contact, blood transfusion or illegal sexual behaviour); like: HIV, Hepatits B & Hepatitis C. Airborne pathogens are type of pathogens that causing airborne diseases (diseaes arise from microbial agents transmitted by air; by coughing, sneezing, laughing or close contact); like; Infuenza, Smallpox, Anthrax (inhalation) & Tuberculosis (TB). Exp. No 2 Tools and practices Objectives 1234- Convert results from one unit format to another using the SI system. Define concentration, simple dilution, and serial dilutions. Be able to use pipettes on proper way. Describe and use centrifuge on proper way. Materials Instruments and tools: 1- Lab coat 2- Pipettes 3- Centrifuges 4- Balances Disposables: 1234- Latex gloves Sharp containers/puncture resistant container Medical wastes bags/container (yellow) Yellow & blue tips Chemicals: 1- Glucose 2- Giemsa Stain Background UNITS OF MEASUREMENT: Prefixes used in SI units: deci centi milli micro nano pico d 0.1 = 10 -1 c 0.01 = 10 -2 m 0.001 = 10 -3 µ 0.000 001 = 10 -6 n 0.000 000 001 = 10 -9 p 0.000 000 000 001= 10 -12 Reporting of laboratory results is often expressed in terms of substance concentration mass of substance (mg/dl, g/L..) units can convert from conventional to SI and vice versa Example (1): Convert 4.5 g/dl albumin to g/L? (e.g: moles) or the g/L=4.5 g/100 ml x 1000 ml/L = 45 g/L Example: A calcium concentration is reported as 10 mg/dl. What is the concentration in mmol/L? (M.W of calcium =40) mmol/L=10 mg/100 ml x 1 mmol/40 mg x 1000 ml/1 L = 2.5 mmol/L CONCENTRATION Concentration of an analyte in solution can be expressed in many ways. Concentration expressed as percent solution, molarity, molality, or normality. There expressions of percent solutions are weight per weight (w/w), volume per volume (v/v), and most commonly weight per volume (w/v). Molarity is expressed as the number of moles per liter of solution. One mole of a substance equals its gram molecular weight. Expressed as moles per liter mol/L , mmol/L, µmol/L, nmol/L. Example: If 4g NaOH are used to make 500 ml of NaOH solution, what is the molarity (M) of the solution? (M.wt of NaOH= 40). DILUTION SIMPLE DILUTION In general it means reducing the concentration of chemicals in solution. The ratio of concentrated or stock solution to the total solution volume equals the dilution factor. The relationship of the dilution factor to concentration is an inverse one, thus the dilution factor increases as the concentration decreases. SERIAL DILUTION Defined as multiple progressive dilutions ranging from more concentrated solutions to less concentrated solution. AUTOMATIC PIPETTES Have many advantages like time saving, safety, easy to use, stability, increase precision, lack of require cleaning. If pipette less than 1 ml it’s called micropipette, if it’s more than 1 ml its called macropipet. CENTRIFUGE The purpose of a centrifuge in the clinical laboratory is to separate substances of different mass or density, separate solid matter from a liquid suspension. A centrifuge consists of a head or rotor, carriers, and shields that are attached to the vertical shaft of a motor and enclosed in a metal covering. The centrifuge always has a lid and an on/off switch. Benchtop centrifuge Fixed head rotor centrifuge Swinging bucket rotor Laboratory Report Exp. No. 2 Tools and practices Student Name: Group No.: ( Activities ) 1- Make dilution 1/5 from giemsa stain solution? 2- Use a balance to weigh 0.006 moles from glucose? (M.wt glucose 180) 3- Prepare 1% concentration of glucose solution? Data Calculations & Results Exp. No 3 Instrumentation Spectrophotometer - pH meter Objectives 1-Explain the general principles for instruments described. 2-Discuss the clinical applications for each instrument. 3-Describe the operation and component parts for each instrument. Materials Instruments and tools: 12345- Spectrophotometer. PH meter. Pipets. Lab coats. Cuvettes. Disposables: 1-Pastuer pipettes 2-Test tubes 3-Tips 4-Latex gloves. 5-Sharp containers. Chemicals: 1- Glucose solution(standards) Introduction-Spectrophotometer Spectrophotometer is the mainstay of the automated clinical chemistry laboratory, uses properties Spectrophotometer is based on two principles: (1) Substances absorb light at unique wavelengths and (2) The amount of light absorbed is proportional to the amount of substance that is present. WAVELENGTH Light transmit as waves Wavelength is a measure of the distance between repetitions of a shape feature such as peaks o Refer as λ and expressed in nm UV Visible IR Microwave Principle Radiant energy that passes through an object will be partially reflected, absorbed and transmitted. Each solution absorbs a unique pattern of wavelength. Light through solution will be some absorbed and reminder passes through (transmitted). Light I0 I Glass cell filled with concentration of solution (C) I: transmitted light I0 : incident light Spectrophotometer depends on Beer's law on their working. Beer's law describes the relationship between absorption of light by a solution and the concentratio Beer's law states that the concentration of a substance is directly proportional to the amount of ligh proportional to the logarithm of the transmitted light. By choosing a wavelength of light that is optimal for the absorbance of the substance, absorption is absorbed by that substance and no other substances. The increase or decrease of light abso concentration of the substance ( % T is inversely proportional to concentration). Calibration Curve-Spectrophotometer A calibration curve is a general method for determining the concentration of a substance in an unknown sample by comparing the unknown to a set of standard samples of known concentration. Plot between absorbance and concentration. Blank: a solution containing no analyte, typically used to zero an analytical instrument and ensure that any reagents used do not contribute to overall measurements (reference point). % T in blank= 100% no light absorbed Calibrators: solutions that contain a known amount of an analyte and are used to calibrate an assay method. Spectrophotometer Components pH Meter A pH meter is an electronic instrument used to measure the pH (acidity or alkalinity) of a liquid (though s used to measure the pH of semi-solid substances). A typical pH meter consists of a special measuring probe (a glass electrode) connected to an electronic m displays the pH reading. Laboratory Report Exp. No 3 Spectrophotometer - pH meter Student Name: Group No.: ( ) Activities 1-when we Measure the absorbance for each of 5 glucose standards tubes, the followings are the concentration of glucose in each tube. Tube 1=conc: 25 mg/dl absorbance : 0.2 Tube 2= 50 mg/dl absorbance : 0.4 Tube 3= 100 mg/dl absorbance : 0.8 Tube 4= 200 mg/dl absorbance : 0.16 Tube 5= 400 mg/dl absorbance : 0.32 Using this data draw the calibration curve, then find the absorbance of following conc. from the curve A) 75 mg/dl B) 150 mg/dl C) 250 mg/dl Data Calculations Exp. No 4 Blood Collection Objectives Describe the venipuncture procedure with necessary equipment, supplies, technique, and precautions. Materials Instruments and tools: 1- Centrifuge 2- Torniquet 3- Racks Disposables: 1234567- gloves adhesive tape sterile alcohol pads cotton veinpuncture needles(different gauge) gauze pads lancet Venipuncture Procedure 1- apply tourniquet, patient should close hand. 2-select venipuncture site 3-cleanse site 4-inspect needle 5-anchor vein-pull skin taut with thumbs ,grasp arm with 4 fingers 6-align needle(bevel up)with vein and insert at 15̊ angle 7-Grasp holder tightly with opposite hand, anchor fingers against arm 8-push tube onto needle, fill 9-release tourniquet ,patient should open hand 10-gently remove tube 11-place gauze ,remove needle 12-apply pressure Exp. No 5 Estimation of Glucose Level in Serum Objectives 1-Describe the principle and methodology used in the analysis of glucose. 2-Describe the clinical significance of abnormal levels of glucose. Materials Instruments and tools: 1-Spectrophotometer 2-Pipets 3-Centrifuge 4-Torniquet 5-racks 6-timer 7-water bath Disposables: 1-cuvettes 2-needles 3-pastuer pipettes 6-cotton 7-test tubes 8-tips 9-adhesive tape Chemicals: Comercial prepared kit. Background Glucose is formed from carbohydrate digestion and conversion of glycogen to glucose by the liver. The two hormones that directly regulate blood glucose are glucagon and insulin. Glucagon accelerates glycogen breakdown in the liver and causes the blood glucose level to rise. Insulin increases cell membrane permeability to glucose, transport glucose into cells (for metabolisim), stimulates glycogen formation, and reduces blood glucose levels. Driving insulin into the cells requires insulin and insulin receptors. For example, after a meal, the pancreas releases insulin for glucose metabolisim, provided there are enough insulin receptors. Insulin binds to these receptors on the surface of target cells such as are found in fat and muscle. This opens the channels so that glucose can pass into cells, where it can be converted to energy. As cellular glucose metabolism occurs, blood glucose levels fall. Principle By enzymatic method called glucose oxidase method. Glucose in the sample originates by means of coupled reactions, a colored complex that can be measured by spectrophotometer. Glucose+1/2 O2+H20 glucose oxidase gluconate+H2O2 2H2O2+ 4-Aminoantipyrine+Phenol peroxidase Quinoneimine+4H2O Patient Preparation Patient should be fasting 10-12 hrs. Or as random sample without fasting. Or as postprandial(after 2 hrs meal) Samples Serum or plasma. Procedure According to kit instructions. Normal Values Fasting: 70-105 mg/dl. Diagnostic Significance Hyerglycemia: 1-Diabetes mellitus. Hyoglycemia: 1-Insulin overdose. 2-Starvation. 3-Pancreatic islet cell carcinoma Interfering Factors 1-Hemolysis. 2-Lipemia. 3-Icteric samples. Exp. No 6 Urea Determination in Serum Objectives 1-Describe the principle and methodology used in the analysis of urea. 2-Describe the clinical significance of abnormal levels of urea. 3-Be aware of interfering factors that affect on this test. 4-Perform this test properly. Materials Instruments and tools: 1-Spectrophotometer 2-Pipets 3-Centrifuge 4-Torniquet 5-Racks Disposables: 1-Plain tubes 2-Needles 3-alcohol pad 4-Pastuer pipets 5-Cotton 6-Test tubes 7-Tips 8-Adhesive tape Chemicals: Comercial prepared kit. Background Urea is an organic compound with the chemical formula (NH2)2CO. The molecule has two amine (-NH2) groups joined by a carbonyl (C=O) functional group. Urea is a major by-product of protein metabolism, urea is synthesised in the liver from ammonia as a result of deamination of amino acids. Urea is found dissolved in blood and is excreted by the kidney as a component of urine. In addition, a small amount of urea is excreted (along with sodium chloride and water) in sweat. Urea concentration in the blood can vary with diet,hepatic function,and numerous disease states. Principle Urea in the sample originates, by means of the coupled reactions described below, a coloured complex that can be measured spectrophotometry. Urea + H2O urease NH4+ + Salicylate + NaClO 2NH4+ + CO2 nitroprusside Indophenol Samples Serum or plasma. Stable for 7 days at 2-8 C Procedure According to kit instructions. Normal Values Serum: 0.15 – 0.45 g/L. 2.5-7.5 mmol/L Urine : 20-35 g/24 hours 338-583 mmol/24 hours Diagnostic Significance Increased in: 1-Accelerated ProteinCcatabolism (illness, fever). 2- Acute and chronic renal failure. Decreased in: 1-Liver failure. 2-Malnutrition. Interfering Factors Hemolysis. Exp. No 7 Uric Acid Determination in Serum Objectives 1-Describe the principle and methodology used in the analysis of uric acid. 2-Describe the clinical significance of abnormal levels of uric acid. Materials Instruments and tools: 1234567- Spectrophotometer Pipets Centrifuge Torniquet Racks Timer water bath Disposables: 1234567- Cuvettes. Needles. Pastuer pipets. Cotton. Test tubes. Tips. Adhesive tape Chemicals: Comercial prepared kit. Background Uric acid is formed from the breakdown of nucleonic acids and is an end product of purine metabolisim.A lack of the enzyme uricase allows this poorly soluble substance to accumulate in body fluids. Two thirds of the uric acid reduced daily is excreted by the kidneys, whereas the remaining once third exits by the stool. The basis for this test is that an over production of uric acid occurs when there is excessive cell breakdown and catabolism of nucleonic acid(as in gout),excessive production and destruction of cells(as in leukemia),or an inability to excrete the substance produced(as in renal failure). Principle By colorimetric method, uric acid is converted by uricase to allantion and hydrogen peroxide which under the catalytic influence of peroxidase ,oxidizes 3,5 dichloro-2-hydroxybenzensulfonic acid and 4-aminoantipyrine to form a red violet quinoneimine compound. Uric acid+O2+2H2O uricase Allantoin+CO2+H2O2 2H2O2+3,5 DHBS+4-AP Peroxidase quinoneimine +4H2O Patient Preparation 1-Nonfasting sample is acceptable for uric acid estimation,but fasting is prefered. 2-Prefer to avoid eating meat before 3 days of the test. Samples Serum or Plasma or urine Procedure According to kit instructions. Normal Values Serum: Males: 3.4-7.0 mg/dl – (202-416 micro mol/l) Females:2.4-5.7 mg/dl (142-339 micro mol/l) Diagnostic Significance Hyperuricemia: 1- Renal diseases. 2-Gout. 3-starvation. 4-leukemia Interfering factors 1-Purine-rich diet. 2- Hemolysis. Exp. No 8 Total Protein Determination in Serum Objectives 1-Describe the principle and methodology used in the determination of total protein. 2- Discuss the factors that influence on the measurement of total protein. 3- Describe the clinical significance of measurement total protein. 4- List the types of samples use to measure total protein. Materials Instruments and tools: 1-Spectrophotometer 2-Pipets 3-Centrifuge 4-Torniquet 5-Racks 6-Timer Disposables: 1-Cuvettes 2-Plain tubes 3-Needles 4-alcohol pad 5-Pastuer pipets 6-Cotton 7-Test tubes 8-Tips 9-Adhesive tape Chemicals: 1-Comercial prepared kit Background Most of the plasma proteins are synthesized by the liver. The major exception to this is the immunoglobulins which are produced by plasma cells found in the spleen, lymph nodes and bone marrow. The two general causes of alterations of serum total protein are change in the volume of plasma water and a change in the concentration of one or more of the serum proteins. Principle Colorimetric determination of total protein in serum based on the principle of the Biuret reaction. Protein in the sample reacts with copper (ii) ion in alkaline medium forming a colored complex that can be measured by spectrophotometer. Samples Serum, heparinized plasma, urine. Stable for 8 days at 2-8 C° Procedure According to kit instructions. Normal Values 6 – 8 g/dL Diagnostic Significance Hyperproteinemia: 1- Dehydration. 2- Vomiting,diarrhea. 3- Multiple myeloma. Hypoproteinemia: 1- Nephrotic syndrome (Kidney diseases). 2- Malnutrition. Interfering Factors 1- Hemolysis . 2- Lipemia. 3- Icteric (bilirubin>20 mg/dl) Exp. No 9 Albumin Determination in Serum Objectives 1-Describe the principle and methodology used in the determination of albumin. 2- Discuss the factors that influence on the measurement of albumin. 3- Describe the clinical significance of measurement albumin. 4- List the types of samples use to measure albumin. Materials Instruments and tools: 1-Spectrophotometer 2-Pipets 3-Centrifuge 4-Torniquet 5-Racks 6-Timer Disposables: 1234567- Cuvettes Test tubes Needles Pastuer pipets Cotton Tips Adhesive tape Chemicals: Comercial prepared kit. Background Albumin is the most abundant protein in human plasma. It has three main functions: it contributes towards maintaining the colloid pressure of plasma, it acts as non-specific transport vehicle for many nonpolar compounds and it is a source of endogenous amino acids. Principle Colorimetric determination of serum albumin which react with bromocresol green in acid medium forming a colored complex that can be measured by spectrophotometry . Samples Serum or plasma. Stable for 3 days at 2-8 C° Procedure According to kit instructions. Normal Values Adult: 3.8-4.4 g/dL.(38-44 g/L) Neonate: 3.8-4.2 g/dL (38-42 g/L) Diagnostic Significance Hyperalbuminemia: Dehydration. Hypoalbuminemia: 1- Malnutrition. 2- Renal diseases. 3- Liver diseases Interfering Factors 1- Hemolysis. 2- Lipemia. 3- Icteric (bilirubin>20 mg/dl) Exp. No 10 Cholesterol Determination in Serum Objectives 1-Describe the principle and methodology used in the analysis of cholesterol. 2-Describe the clinical significance of abnormal levels of cholesterol. 3-Be aware of interfering factors that affect on this test. 4-Perform this test properly. Materials Instruments and tools: 1-Spectrophotometer 2-Pipets 3-Centrifuge 4-Torniquet 5-Racks 6-Timer Disposables: 1-Cuvettes 2-Plain tubes 3-Needles 4-alcohol pad 5-Pastuer pipets 6-Cotton 7-Test tubes 8-Tips 9-Adhesive tape Chemicals: Comercial prepared kit. Background Cholesterol is unsaturated steroid alcohol (sterol) found in animal fats and oils. It is widely distributed throughout the body, especially in the blood, brain, liver, kidneys, and nerve fiber myelin sheaths, and it is an essential component of cell membrane development and production of bile acids, adrenal steroids, and sex hormones. Dietary cholesterol is partially absorbed and it is also synthesized by the liver. Principle Free and esterified cholesterol in the sample originates, by means of the coupled reactions described below, a colored complex that can be measured by spectrophotometry. Cholesterol ester + H2O chol.esterase cholesterol + fatty acid Cholesterol + ½ O2 + H2O chol.oxidase cholesterol + H2O2 2H2O2 + 4-Aminoantipyrine + Phenol peroxidase Samples Serum or plasma. (Cholesterol is stable for 7 days at 2-8 C.) Quinoneimine +4 H2O Procedure According to kit instructions. Normal Values Normal : Up to 200 mg/dl. Diagnostic Significance Elevated cholesterol levels are found in: 1-Atheroscelerosis 2-Coronary artery diseases. 3-Obesity. Interfering Factors 1-Hemolysis. 2- Medications. 3-Lipemic samples. 4-Icteric samples. Exp. No 11 Triglyceride Determination in Serum Objectives 1-Describe the principle and methodology used in the analysis of Triglyceride. 2-Describe the clinical significance of abnormal levels of Triglyceride. Materials Instruments and tools: 1-Spectrophotometer 2-Pipets 3-Centrifuge 4-Torniquet 5-racks 6-timer 7-water bath Disposables: 1-cuvettes 2-needles 3-pastuer pipets 4-cotton 5-test tubes 6-tips 7-adhesive tape Chemicals: Comercial prepared kit. Background Triglycerides are a type of fat in the bloodstream and fat tissue. Triglycerides are created both naturally by our livers, and consumed through the foods we eat. They are formed in the intestinal mucosa by the esterification of glycerol and free fatty acids. The fat which is already stored in our body is made up triglycerides, and consuming foods which are high in these, can lead to even more of it being stored, posing several health risks. Principle By colorimetric method.Triglyceride in the sample originates , by means of the coupled reactions described below,a coloured complex formed and measured by spectrophotometer. Triglyceride+ H2O lipase glycerol+fatty acids glycerol+ATP glycerol-3-P+O2 glycerol kinase glycerol-3-p +A G-3-P-oxidase Dihydroxyacetone-P + H2O2 2H2O2+4-Aminoantipyrine+ 4-Chlorophenol peroxidise Quinoneimine+4H2O Patient Preparation Fasting for at least 12 hours. Samples Serum or plasm. Procedure According to kit instructions. Normal Values Normal: Up to 150 mg/dl. Diagnostic Significance Increased in: 1-Liver diseases. 2-Myocardial infarction. 3-Hyperlipidemia. 4-Atherosclerosis. Interfering factors 1- Hemolysis: decrease result. 2- Drugs. Exp. No 12 Bilirubin Determination in Serum Objectives 1-Describe the principle and methodology used in the analysis of total and direct bilirubin. 2-Describe the clinical significance of abnormal levels of bilirubin total and direct. Materials Instruments and tools: 1-Spectrophotometer 2-Pipets 3-Centrifuge 4-Torniquet 5-Racks 6-Timer Disposables: 1-Cuvettes 2-Needles 3-Pastuer pipets 4-Cotton 5-Test tubes 6-Tips 7-Adhesive tape Chemicals: Comercial prepared kit. Background Bilirubin results from the breakdown of haemoglobin in red blood cells and is a byproduct of hemolysis. It is produced by the reticuloendothelial system. Removed from the body by the liver, which excretes it into the bile, it gives the bile its major pigmentation. Usually , a small amount of bilirubin is found in the serum. A rise in serum bilirubin levels occurs when there is an excessive destruction of red blood cells or when the liver is unable to excrete the normal amounts of bilirubin produced. There are two forms of bilirubin in the body: indirect or unconjugated bilirubin(water insoluble) , which is protein bound, and direct or conjugated bilirubin ,which circulates freely in the blood until it reaches the liver, where it is conjugated with glucuronic acid by enzyme uridyldiphosphate glucuronyl transferase(UDPG-T) and then excreted into the bile. An increase in protein-bound bilirubin(unconjugated bilirubin) is more frequently associated with increased destruction of red blood cells(hemolysis),an increase in free-flowing bilirubin is more likely seen in dysfunction or blockage of the liver. A routine examination measures only the total bilirubin. A normal level of total bilirubin rules out any significant impairment of the excretory function of the liver or excessive hemolysis of red cells. Only when total bilirubin levels are elevated will there be a call for differentiation of the bilirubin levels by conjugated and unconjugated types. Principle Serum is added to a solution of sodium acetate and caffeine-sodium benzoate, then added to diazotized sulfanilic acid to form purple azobilirubin. Alkaline tartarate solution added to convert the purple azobilirubin to blue azobilirubin. Direct bilirubin is determined in the absence of caffeine. Sodium acetate buffers the PH of the diazotization reaction. Caffeine sodium benzoate accelerates the coupling of bilirubin with diazotised sulfanilic acid. Samples Serum. Bilirubin in serum is stable for 2 days at 2-8 C°, protect from light. Samples with high bilirubin level called icteric samples . Procedure According to kit instructions. Normal Values Adult : Up to 1.0 mg/dl (total) Up to 0.2 mg/dl (direct) Diagnostic Significance Elevated level of total bilirubin (hyperbilirubinemia) is found in: 1-Hepatocellular jaundice. 2-Hemolytic jaundice. 3-Obstructive jaundice. 4-Physiological jaundice. Interfering Factors 1- Hemolysis. 2- Lipemia. 3- A 1-hour exposure of the specimen to sunlight or high intensity artificial light at room temperature will decrease the bilirubin content.