When Kids Are Sweet as Sugar
advertisement

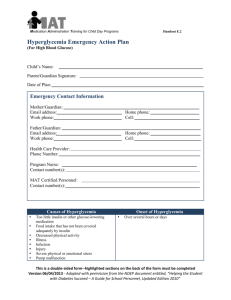
When Kids Are Sweet as Sugar and Sick as *&#! Teri Campbell RN, BSN, CEN, CFRN University of Chicago Aeromedical Network Aerocare DKA • Complex metabolic state • Emergency vs. life-threatening • Hospitalizations • Cerebral edema Objectives • Participants will define DKA • Participants will identify precipitating factors • Participants will discuss common presentation • Participants will review pre-hospital vs. hospital stabilization goals • Participants will discuss treatment options • Participants will review potential complications Definition Triad • Hyperglycemia • Ketonemia • Acidemia That’s a lot of “emias”… Definition • Blood glucose: > 250 mg/dl • PH: < 7.3 • Serum Bicarbonate: < 15 mEq/L • Urinary ketone: > = 3+ • Serum Ketone: positive at 1:2 dilutions • Serum osmolality: Variable All the stats… • Incidence / frequency • Race • Mortality Precipitating factors • New diagnosis • Infections • Non-compliance • Endocrine changes • Caregiver lack of compliance • Pump failure What a story… History • Polydipsia, Polyuria • Fatigue • Malaise •N/V • Weight loss • Fever History Abdominal pain Pathology Decreased Insulin Increase of “stress hormones” • catecholamines • glucagon • growth hormone • cortisol Pathology Lots and lots of sugar to no avail… • Proteolysis • Ketones • Lipolysis • Lactic acids Presentation Soooo… How do they LOOK? • mental status changes • tachycardia • kussmaul • B/P • delayed cap refill • possibly febrile Hyperglycemia • High serum glucose • Big sponge Dehydration and thirst • Intra-cellular dehydration • Extra-cellular fluid expansion • Hyponatremia • Polyuria • H20 losses exceed NaCl losses • Decrease urine blood flow • Glucose retention Acidosis 2 main culprits Ketones : Proteolysis Lactic acid: Lipolysis Tissue hypoperfusion Hyperosmolality • Directly related to hyperglycemia • Increased serum osmols • Increased cerebral osmols Electrolyte disturbances • NA: low, normal or high • Increased K+ • Decreased K+ Treat hypokalemia first or…ZAP! Fluids → K+ → Insulin Labs • Glucose • K+ • ABG’s • Electrolytes: CL, HCo3, BUN, Cr, Phos Labs • CBC • blood / urine culture • UA • serum osmolality • EKG: hyperK+ = peaked T waves SHOCK hyperkalemia? _______ Pre-hospital • A: mental status changes • B: O2, BVM, Sellicks • C: Isotonic fluids • 20 cc/kg X ONE… • What size IV? Pre-hospital • D: Altered mentation? • History? Long transport? It’s time we face reality, my friends Global goals • Restore perfusion • Give insulin • Correct electrolyte disturbances • Avoid complications Where are we going? And why am I in this Hand basket? Fluid therapy • 1st 1-2 hours of therapy • Isotonic 20cc/kg • Shock • 0.9 NS vs. 0.45 NS • 1.5 – 2.0 X maintenance • BSA: 1200cc/M2/day Fluid therapy • • • • 4-2-1 Rule 1st 10 kg : 40 cc 2nd 10 kg : 20 cc 1cc for every kg over (20kg) 1st 10 kg: 40cc 2nd 10 kg: 20 cc all the other kg (1cc/kg): 17 cc 77 cc/hr 37 kg child: Potassium supplement • Profound hypoK+: oral vs. IV • Treat before insulin • K+ > 5.5: No K+ to IVFs • KCL vs K phosphate Slowwwww lab? Insulin • Bolus controversy • timing controversy • prime the tubing • 0.1 units/kg/hr • 0.05 units/kg/hr • clear ketones • Regular insulin 1:1 Bicarbonate • Rarely indicated • Evidence? • PH < 7.0 • Adverse hemodynamic effects • Hypokalemia, hyperNA, alkalemia • Never give IV push Glucose • Blood sugar @ 250 mg/dL • D5, D10 • Ketones, prevent hypoglycemia • serum glucose: 100-150 mg/dL 150-250 mg/dL • Fall: 50-70 mg/dL / first hour Serum Osmolality • Normal range • > 320 risk for cerebral edema • > 320 correct volume over 36 hours • > 340 correct volume over 48 hours Complications Cerebral edema • More common kids / adol. • Incidence: 0.3-1.0% • Mortality: 70% • Risk factors • Presentation Pathology • Hyperglycemia = high serum osmols • High serum osmols = high brain osmols • Rapid correction: volume or sugar • Gradient: intracerebral & serum osmols • Free H20 into brain Treatment Initial CT Mannitol Hypertonic saline ARDS • Rare • Potentially fatal • Lots of crystalloids • Normal cardiac function Key points • Often misdiagnosed • Replace cellular and intravascular losses • Insulin to allow glucose utilization • Possible correction of electrolytes • Prevent complication In conclusion… Keep it slow….. It took them weeks to get here… It will take days to fix them…. When Kids Are Sweet as Sugar and Sick as *&#! Teri Campbell RN, BSN, CEN, CFRN University of Chicago Aeromedical Network Aerocare tlcsoup@aol.com