Functions of the kidney
advertisement

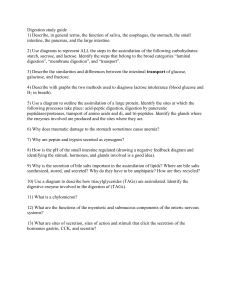
Definitions Digestion: Breakdown of ingested nutrients into forms which can be absorbed Absorption: Transport of small molecules from the GI tract into the blood Motility: Patterns of GI contraction and relaxation; tone of sphincters Secretion: Control of secretion of digestive enzymes & regulatory hormones 1 Gastrointestinal functions fig 15-2 Digestion: mouth, stomach, small intestine Absorption: small intestine Secretion: mouth, stomach, small intestine Motility: entire GI tract 2 GI functions: mouth, esophagus, stomach, pancreas fig 15-3a 3 GI functions: biliary system, small intestine, large intestine fig 15-3b 4 Fluid exchanges Oral intake: 1200 ml/day Secretions: 7000 ml/day Absorption: 8100 ml/day Feces: 100 ml/day Significance: potential for fluid loss if absorption compromised fig 15-5 5 Microanatomy of GI tract Mucosa: absorptive epithelium, endocrine/exocrine cells, muscularis mucosa Submucosa: blood/lymph vessels, submucosal nerve plexus Muscularis externa: circular muscle, myenteric nerve plexus, longitudinal muscle Serosa, mesentery fig 15-6 6 Intestinal structure: villi fig 15-7 Surface area: “tennis court”, villi, microvilli (next) Life cycle: ~5 day life cycle, generated at base of villi, shed from top 7 The intestinal cell fig 15-8 Surface enzymes: released into intestine as cells released Microvilli = “brush border” 8 Carbohydrate digestion & absorption Source: ~ half of daily caloric intake ~ 70% as starch (potatoes, pasta, rice, bread), ~ 30% as sucrose, lactose cellulose: glucose links not digestible, forms “bulk” of diet Starch: 14, 16 links hydrolyzed by salivary & pancreatic amylase maltose, maltotriose Intestinal disaccharidases: maltase: hydrolyses maltose, maltotriose glucose sucrase: hydrolyses sucrose glucose + fructose lactase: hydrolyses lactose glucose + galactose Absorption: from small intestine into blood capillaries Glucose, galactose by Na+ linked cotransport at luminal border Fructose by facilitated diffusion at luminal border Glucose, galactose, fructose by facilitated diffusion at basolateral surface 9 Protein digestion & absorption Source: ~ 20% of daily caloric intake Digestion: gastric *pepsin (endopeptidase, acid pH optimum) pancreatic *trypsin & *chymotrypsin (endopeptidase, alkaline pH optimum) pancreatic carboxypeptidase (exopeptidase) intestinal aminopeptidase (exopeptidase) Absorption: small intestine, into blood capillaries aminoacids by Na+ linked cotransport, di- & tri-peptides by H+ linked cotransport at luminal border peptides hydrolyzed in intestinal cell aminoacids by facilitated diffusion at basolateral membrane * secreted as inactive precursor (next slide) 10 Pepsin, trypsin, chymotrypsin activation pepsin trypsin, chymotrypsin fig 15-21 fig 15-26 11 Lipid digestion & absorption Source: Triglyceride, ~30% of daily caloric intake Digestion: pancreatic lipase (triglyceride 2-monoglyceride + 2 fatty acids) lipases act at fat water interfaces & depend on fat surface area Emulsification: mechanical disruption (chewing, motility of stomach & small intestine amphipathic emulsifiers (bile salts, bile phospholipid) 12 Anatomy of bile & pancreatic ducts Bile: produced in liver, stored in gall bladder Composition: bile salts, phospholipids, cholesterol, bicarbonate, bile pigments (heme metabolism), drug metabolites & trace metals fig 15-4 13 Bile salt actions fig 15-9 fig 15-10 Bile: produced in liver, stored in gall bladder Emulsification in duodenum & upper intestine 14 Triglyceride digestion Colipase: from pancreas, binds lipase to emulsion droplet Micelles: 4-7 nm diameter store of fatty acids & monoglycerides for transport into epithelial cells fig 15-11 15 Triglyceride absorption Resynthesis: 2 FA + MG TG on smooth endoplasmic reticulum Chylomicrons: 80-90% triglyceride + phospholipid + cholesterol, coated with amphipathic proteins released by exocytosis into lacteal metabolized by fat & liver fig 15-12 16 Vitamins, water absorption Water: passively absorbed down osmotic gradient GI wall permeable, therefore GI contents isosmotic mostly from small intestine Vitamins: lipid soluble (vit A, D, E, K) with lipids (micelles, diffusion, chylomicrons) water soluble (vit B, vit C) diffusion, mediated transport vit B12 with intrinsic factor (from stomach parietal cells), endocytosis 17 Regulation of secretion: general Luminal stimuli: 1. distension of wall (volume stimulates mechanoreceptors) 2. osmolality of chyme (osmoreceptors) 3. acidity of chyme (chemoreceptors) 4. chyme concentration of digestive products: monosaccharides, fatty acids, peptides, aminoacids (chemoreceptors) 18 Neural regulation Long reflexes: mostly parasympathetic Short reflexes: enteric nervous system, myenteric & submucosal plexuses, conduct impulses up & down GI tract fig 15-13 19 Hormonal regulation (simplification of table 15-4) Gastrin Cholecystokinin Secretin GIP Structure peptide peptide peptide peptide Source G cells in stomach small intestine epithelium small intestine epithelium small intestine epithelium Release stimulus Parasymp NS, FA’s, AA’s in small stomach AA’s, intestine; peptides osmolality ( pH inhibits) pH in small intestine glucose, AA’s in small intestine Actions stomach enzymes, H+, motility secretion of bile & pancreatic HCO3- insulin secretion secretion of bile, pancreatic enzymes, relaxes sphincter of Oddi GIP = glucose insulinotropic peptide (gastric inhibitory peptide) Cholecystokinin & secretin potentiate each others’ actions 20 Saliva Composition: fluid, mucus, amylase Functions: moistening food, preventing tooth decay (lysozyme, IgA), starting starch digestion Regulation of release: parasympathetic NS (responding to sight, smell, thought of food) sympathetic NS (transient); ( saliva flow, blood flow) acidic fruit juices, mechanical contact 21 Gastric secretion fig 15-17 fig 15-16 Structure: fundus, body, antrum; lower esophageal & pyloric sphincters Goblet cells mucus, Parietal cells HCl & intrinsic factor, Chief cells pepsinogen, G cells gastrin 22 HCl secretion by parietal cells fig 15-18 As HCl is secreted, HCO3- is returned to the GI blood (“alkaline tide”) Function of HCl: not digestive, kills potential parasites: bacteria etc. 23 Regulation of HCl secretion fig 15-20 HCl secretion increased by: parasympathetic NS stimulation (cephalic phase) gastrin (direct & via histamine from mast cells) (gastric phase) HCl secretion inhibited by somatostatin 24 Phases of gastric secretion of pepsinogen & HCl Cephalic phase: stimulus: sight, smell, thought of food, chewing mechanism: parasympathetic NS secretion & motility Gastric phase: stimulus: aminoacids, peptides in stomach, distension, pH as food enters mechanism: short/long loop reflexes, gastrin secretion & motility Intestinal phase: stimulus: intestinal distension, pH, osmolality, digestive products mechanism: short/long loop reflexes, secretin, CCK, GIP 25 Pancreatic secretion Enzymes (a reminder): trypsin, chymotrypsin, (elastase), carboxypeptidase amylase, lipase, (phospholipases, nucleases) Bicarbonate fig 15-25 26 Regulation of pancreatic secretion Stimulus: fatty acids, glucose, osmolality, distension in small intestine Mediator: cholecystokinin Response: relaxation of sphincter of Oddi, contraction of gall bladder secretion of pancreatic enzymes, potentiation of secretin actions Stimulus: pH in small intestine Mediator: secretin Response: secretion of bicarbonate in pancreatic juice & bile Stimulus: glucose in small intestine Mediator: glucose insulinotropic peptide (GIP) Response: secretion of insulin, inhibition of gastric secretion 27 Regulation of pancreatic secretion fig 15-28 fig 15-27 28 Bile Source: produced in liver, stored & concentrated in the gall bladder Composition: bile salts, phospholipids, cholesterol (emulsify fats) bicarbonate (neutralizes HCl) bile pigments (heme metabolism), drug metabolites & trace metals Regulation of secretion: intestinal fatty acids cholecystokinin gall bladder contraction Enterohepatic circulation: next screen 29 Regulation of bile secretion fig 15-31 30 Bile enterohepatic circulation Bile salts circulate 2-3x per meal fig 15-30 31 Gastrointestinal motility omitted Omit objectives 16-20 32 Liver functions 1. exocrine function: bile salts, bicarbonate 2. plasma proteins: albumin, binding proteins, angiotensinogen 3. metabolism: gluconeogenesis, urea, ketoacids, lipoproteins 4. cholesterol synthesis, secretion in bile 5. excretion: bile pigments, trace metals, drug metabolites 33