Immunity to Intracellular Bacteria Innate and Adaptive Immunity to
advertisement

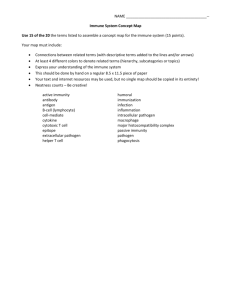
Chapter 16 Immunity to Microbes Important General Features of Immunity to Microbes Defense against microbes is mediated by the effector mechanisms of innate and adaptive immunity The immune system responds in specialized and distinct ways to different types of microbes to most effectively combat these infectious agents Survival and pathogenicity of microbes in a host are critically influenced by the ability of the microbes to evade or resist the effector mechanisms of immunity Many microbes establish latent, or persistent, infections in which the immune response controls but does not eliminate the microbe and the microbe survives without propagating the infection Tissue injury and disease may be caused by the host response IMMUNITY TO EXTRACELLULAR BACTERIA Immunity to Extracellular Bacteria Innate Immunity to Extracellular Bacteria Principal mechanisms of innate immunity to extracellular bacteria are complement activation, phagocytosis, and the inflammatory response Toll-like receptors (TLRs) of phagocytes participate in the activation of the phagocytes as a result of encounter with microbes Cytokines also induce the systemic manifestations of infection, including fever and the synthesis of acute-phase proteins Adaptive Immune System to Extracellular Bacteria Injurious Effects of Immune Responses Principal injurious consequences of host responses to extracellular bacteria are inflammation and septic shock Septic shock is a severe pathologic consequence of disseminated infection by gram-negative and some gram-positive bacteria TNF is the principal cytokine mediator of septic shock, but IFN-γ and lL12 may also contribute Bacterial Super -Antigen Staph. Aureus (SEA-E), TSST, Mycoplasma (Exotoxins), Streptococci (Endotoxins) Entrotoxin bind to the Vβ region of TCR and MHC class II Polyclonal activation of T cells by bacterial superantigens Immunity to Intracellular Bacteria Downloaded from: StudentConsult (on 7 October 2006 08:19 AM) © 2005 Elsevier Innate and Adaptive Immunity to Intracellular Bacteria Cooperation of CD4+ and CD8+ cells in Defense Against Intracellular Microbes Downloaded from: StudentConsult (on 7 October 2006 08:19 AM) © 2005 Elsevier T Cells and Cytokines Role in Infection Outcome Downloaded from: StudentConsult (on 7 October 2006 08:19 AM) © 2005 Elsevier Immunity to Tb Mycobacteria are slow-growing, aerobic , facultative intracellular bacilli whose cell walls contain high concentrations of lipids BCG ( bacillus Calmette-Guerin) used as a vaccine against Tb CD4+ T cells, IFNγ, TNF DTH & Granuloma & Caseous necrosis PPD (purified protein derivative) Mechanisms of Immune Evasion by Bacteria Immunity to Fungi Fingi infection called mycoses are important causes of morbidity and mortality in humans Compromised immunity is the most important predisposing factor (opportunistic infection) The principal mediators of Innate Immunity are neutrophils and macrophages (neutropenia) Phagocytes and dendritic cells sense fungal organisms by TLRs and lectin-like receptors called dectins Neutrophils presumably liberate fungicidal substances, such as reactive oxygen species and lysosomal enzymes, and phagocytose fungi for intracellular killing Cell-mediated immunity is the major mechanism of adaptive immunity against fungal infections Histoplasma capsulatum, C. neoformans facultative intracellular parasite Many extracellular fungi elicit strong TH17 responses Individuals with defective TH17 responses are susceptible to chronic mucocutaneous Candida infections and Pneumocystis jiroveci Immunity to Viruses Viruses are obligatory intracellular microorganism Cytopathic effect of viruses Innate immunity to viruses: Antiviral state by IFN type I NK cell-mediated killing Adaptive immunity to viruses: Antibodies CTL & cross priming Innate and Adaptive Immune Responses to Viruses Downloaded from: StudentConsult (on 7 October 2006 08:19 AM) © 2005 Elsevier Innate and Adaptive Immune Responses to Viruses Downloaded from: StudentConsult (on 7 October 2006 08:19 AM) © 2005 Elsevier Mechanisms of Immune Evasion by Viruses Immunity to parasites Parasitic infection such as protozoa, helminths, and ectoparasites (ticks and mites) Innate immunity to parasites: to protozoa and helminths is phagocytosis but may resist activate the alternative pathway of complement Adaptive immunity to parasites: to protozoa is macrophage activation by Th1 cell-derived cytokines to helminths is Th2 cells and IgE and activation of eosinophils then secrete MBP that is severe toxin for helminths Tissue injury after Adaptive immune responses (as fibrosis) Immune Responses to Disease-Causing Parasites Mechanisms of Immune Evasion by Parasites STRATEGIES FOR VACCINE DEVELOPMENT The birth of immunology as a science dates from Edward Jenner's successful vaccination against smallpox in 1796 The success of active immunization in eradicating infectious disease is dependent on numerous factors: Vaccines are effective if the infectious agent does not establish latency, if it does not undergo much or any antigenic variation, and if it does not interfere with the host immune response limited to human hosts, and do not have animal reservoirs Vaccines Adjuvants and Immunomodulators Most adjuvants elicit innate immune responses, with increased expression of costimulators and production of cytokines such as IL-12 that stimulate T cell growth and differentiation Heat-killed bacteria are powerful adjuvants that are commonly used in experimental animals with severe local inflammation Several are in clinical practice, including aluminum hydroxide gel (which appears to promote B cell responses) and lipid formulations that are ingested by phagocytes IL-12 incorporated in vaccines promotes strong CMI plasmid DNA has intrinsic adjuvant-like activities, and it is possible to incorporate costimulators (e.g., B7 molecules) or cytokines Passive Immunization Passive immunity is short-lived because the host does not respond to the immunization and protection lasts only as long as the injected antibody persists In the clinical situation, passive immunization is most commonly used for rapid treatment of potentially fatal diseases caused by toxins, such as tetanus, and for protection from rabies and hepatitis Passive immunization does not induce memory, so an immunized individual is not protected against subsequent exposure to the toxin or microbe