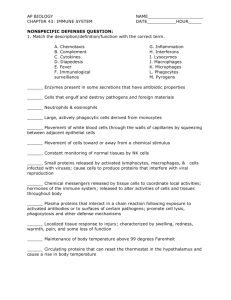
innate (non-specific) immunity
advertisement

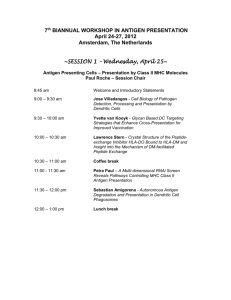
Normal Immune System Function Karim Rafaat Organs of the Immune System Central lymphoid organs Central (primary) lymphoid organs are the sites for generation and early maturation of lymphocytes T cells mature in the thymus (T for thymus) B cells mature in the bone marrow B for bursa of Fabricius (a lymphoid organ in birds) [After Hieronymus Fabricius (1537-1619), Italian anatomist] Lymphoid organs contain lymphocytes and non-lymphoid cells such as macrophages and dendritic cells (and epithelial cells) Lymphoid organs are important for the generation and maturation of lymphocytes, the initiation of immune responses and the perpetuation of immune responses Peripheral lymphoid organs 1. trap antigens 2. are the sites for initiation of most immune response 3. provide signals for recirculation of lymphocytes 4. Antigen delivery to regions of increased *other stuff (not traffic peripheral lymphoid organs) Flow of lymph Gut associated lymphoid tissue (GALT)(tonsils, adenoids, Peyer’s patches, appendix) •Immature B and T cells mature in the central lymphoid organs •Then, they circulate in the blood and through the peripheral lymphoid organs. As long as they have not encountered the specific antigen that binds their antigen receptors (BCR or TCR), the circulating lymphocytes are mature naïve lymphocytes When they encounter antigen (bind antigen in their antigen receptor), they 1. Stick in the lymph nodes (or other peripheral lymphoid organ)(they stop circulating, i.e., altered trafficking) 2. Proliferate (divide) 3. Differentiate Innate and Specific immunity; Cells of the Immune System Cells of the Immune System Myeloid cells lymphoid cells Granulocytic Monocytic T-cells B-cells Neutrophils Basophils Eosinophils Macrophages Langerhans & Kupffer cells Dendritic cells? Helper Cytotoxic Suppressor Plasma cells Dendritic cells? Components of the Immune System Nonspecific Humoral complement, interferon, TNF etc. Cellular macrophages, neutrophils Specific Humoral antibodies Cellular T cells; other effectors cells Characteristics of Innate and Adaptive Immunity Innate Immunity Adaptive Immunity Antigen independent Antigen dependent No time lag A lag period Not antigen specific Antigen specific No Immunologic memory Development of memory Components of Innate and Adaptive Immunity Innate Immunity Adaptive Immunity physical barriers skin, gut Villi, lung cilia,etc soluble factors many protein and non-protein secretions cells phagocytes, NK cell eosinophils, K cells non e Immunoglobulins (antibody) T and B lymphocytes Effector mechanisms in Innate Immunity Site Skin GI tract Lung Component Functions squamous cells sweat desquamation flushing, fatty acids columnar cells Peristalsis, low pH bile salts, fatty acids tracheal cilia mucociliary elevator surfactants Effector mechanisms in Innate Immunity Site Component Functions Nasopharynx and eye mucus, saliva, tears flushing, lysozyme Blood and Lymphiod organs Phagocytes phagocytosis and intracellular killing K, NK & LAK cells direct and antibody dependent cytolysis Effector mechanisms in Innate Immunity Site Serum and other serous fluids Component Functions lactoferrin, transferrin iron deprivation interferons, TNF- antiviral proteins phagocyte activation lysozyme Fibronectin & complement peptidoglycan hydrolysis opsonization, enhanced phagocytosis, inflammation Phagocytes are the Most Important Cells George Bernard Shaw wrote: “There is at bottom only one genuine treatment for all diseases,…to stimulate Influenced by the work of phagocytes.theDrugs are a Eli Metchnikoff, delusion. …(when) the phagocytes are stimulated; they devour the disease…” Phagocytes: Macrophages phagocytosis, intracellular and extra-cellular killing, tissue repair, antigen presentation for specific immune response characteristic nucleus and CD14 membrane marker. Phagocyte Response to Infection The SOS Signals –N-formyl methionine –Clotting system peptides –Complement products Phagocyte response –Vascular adherence –Diapedesis –Chemotaxis –Activation –Phagocytosis and killing Initiation of Phagocytosis Attachment via ScavengerR IgG FcR CR Toll-like R Respiratory Burst Oxygen Dependent Myeloperoxidase Independent Reactions Glucose +NADP+ G-6-P-dehydrogenase NADPH + O2 Cytochrome b558 Pentose-P + NADPH + NADP + O2 - - 2O2 + 2H+ Superoxide dismutase - 2O2 + H2O2 H2O2 + 1O2 .OH + OH- + 1O2 Mediators of Oxygen Independent Killing in the Phago-lysosome Effector Molecule Function Cationic proteins (cathepsin) Damage to microbial membranes Lysozyme Hydrolyses mucopeptides in the cell wall Lactoferrin Deprives pathogens of iron Hydrolytic enzymes (proteases) Digests killed organisms Non-specific Killer Cells NK and LAK cells ADCC (K) cell Activated macrophages Eosinophils They all kill foreign and altered self targets Natural Killer (NK) cells also known as large granular lymphocytes (LGL) kill infected and malignant cells are identified by the presence of CD56 & CD16 and absence of CD3 activated by IL2 and IFN-γ to become LAK cells Lymphokine Activated Killer (LAK) cell kills kills transformed malignant and malignant cells cells Innate Immunity • The complement system Complement: history Discovered in 1894 by Bordet It represents lytic activity of fresh serum Complement functions Host benefit: opsonization to enhance phagocytosis phagocyte attraction and activation lysis of bacteria and infected cells regulation of antibody responses clearance of immune complexes clearance of apoptic cells Host detriment: Inflammation, anaphylaxis Proteins of the complement system (nomenclature) C1(qrs), C2, C3, C4, C5, C6, C7, C8, C9 factors B, D, H and I, properdin (P) mannose binding lectin (MBL), MBL associated serine proteases (MASP-1 MASP-2) C1 inhibitor (C1-INH, serpin), C4-binding protein (C4-BP), decay accelerating factor (DAF), C1 receptor (CR1), protein-S (vitronectin) Pathways of complement activation CLASSICAL PATHWAY antibody dependent LECTIN PATHWAY ALTERNATIVE PATHWAY antibody independent Activation of C3 and generation of C5 convertase activation of C5 LYTIC ATTACK PATHWAY Components of the Classical Pathway C3 C1 complex C4 Classical Pathway Generation of C3-convertase Classical Pathway Generation of C3-convertase C4b2a is C3 convertase C4b Classical Pathway Generation of C5-convertase C4b2a3b is C5 convertase; it leads into the Membrane Attack Pathway C4b C3b Components of mannose-binding lectin pathway MBL MASP1 Mannose-binding lectin pathway C4b2a is C3 convertase; it will lead to the generation of C5 convertase MASP1 MBL Components of the alternative pathway C3 Spontaneous C3 activation Generation of C3 convertase C3 i b C3b C3iBb complex has a very short half life C3-activation the amplification loop If spontaneously-generated C3b is not degraded C3b b C3 b C3-activation the amplification loop C3 b C3b b C3b C3-activation the amplification loop C3 b b C3b C3b C3b C3-activation the amplification loop C3b C3b C3b C3b C3-activation the amplification loop C3b C3b C3b Control of spontaneous C3 activation via DAF DAF prevents C3b the binding of factor B to C3b CR1 Autologous cell membrane Control of spontaneous C3 activation via CR1 C3b CR1 Autologous cell membrane C3b iC3b CR1 C3b stabilization and C5 activation C3b finds an activator (protector) membrane This is stable C5 convertase of the alternative pathway C3b b C3 b C3b regulation on self and activator surfaces C3b C5-convertase of the two pathways C5-convertase of the Classical and lectin Pathways C4b C3b C5-convertase of the Alternative Pathway C3b C3b Lytic pathway Generation of C5 convertase leads to the activation of the Lytic pathway Components of the lytic pathway C7 C6 C 9 Lytic pathway C5-activation b C4b C3b Lytic pathway assembly of the lytic complex C6 C7 b Lytic pathway: insertion of lytic complex into cell membrane C6 C7 CC C C C9 9 9 9C 9C C C9 9 9 9 b Biological effects of C5a Opsonization and phagocytosis Biological properties of C-activation products Product C2b (prokinin) C3a (anaphylatoxin) Biological Effects edema mast cell degranulation; enhanced vascular permeability; anaphylaxis Regulation C1-INH carboxypeptidase- B (C3-INA) Biological properties of C-activation products Product Biological Effects Regulation C3b (opsonin) opsonization; phagocyte activation factors H & I C4a (anaphylatoxin) as C3, but less potent (C3-INA) C4b (opsonin) opsonization; phagocytosis C4-BP, factor I Biological properties of C-activation products Product Biological Effects Regulation C5a (chemotactic factor) anaphylactic as C3, but much more potent; attracts & activates PMN causes neutrophil aggregation, stimulation of oxidative metabolism and leukotriene release carboxypeptidase-C (C3-INA) C5b67 chemotaxis, attaches to other membranes protein-S Antigens Factors Influencing Immunogenicity Contribution of the Immunogen • Foreignness • Size • Chemical Composition – – – – Primary Structure Secondary Structure Tertiary Structure Quarternary Structure Sequence determinants Conformational determinants Factors Influencing Immunogenicity Contribution of the Immunogen • Foreigness • Size • Chemical Composition • Physical Form • Degradability – Ag processing by Ag Presenting Cells (APC) Factors Influencing Immunogenicity Contribution of the Biological System • Genetics – Species – Individual • Responders vs Non-responders • Age Factors Influencing Immunogenicity Method of Administration • Dose • Route – Subcutaneous > Intravenous > Intragastric • Adjuvant – Substances that enhance an immune response to an Ag Chemical Nature of Immunogens • Proteins • Polysaccharides • Nucleic Acids • Lipids – Some glycolipids and phosopholipids can be immunogenic for T cells and illicit a cell mediated immune response Types of Antigens T-independent • Polysaccharides • Properties – Polymeric structure – Polyclonal B cell activation – Resistance to degradation • Examples – Pneumococcal polysaccharide, lipopolysaccharide – Flagella Types of Antigens T-dependent • Proteins • Structure • Examples – Microbial proteins – Non-self or Altered-self proteins Antigenic Determinants Recognized by B cells and Ab • Composition – Proteins, polysaccharides, nucleic acids • Size – 4-8 residues Antigenic Determinants Recognized by T cells • Composition – Proteins (some lipids) – Sequence determinants • Processed • MHC presentation (lipid presentation by MHC-like CD1) • Size – 8 -15 residues • Number – Limited to those that can bind to MHC Biological Foreign bit receptor Consequence of Interaction Microbial cell wall Complement Opsonization; components Complement activation MannoseMannose-binding Opsonization; containing protein Complement carbohydrates activation Polyanions Scavenger receptors Phagocytosis Lipoproteins of Gram + bacteria Yeast cell wall components TLR-2 (Toll-like receptor 2) Macrophage activation; Secretion of inflammatory cytokines Foreign bit Double stranded RNA receptor TLR-3 LPS TLR-4 (lipopolysaccharid e of Gram – bacteria Flagellin (bacterial TLR-5 flagella) Biological Consequence of Interaction Production of interferon (antiviral) Macrophage activation; Secretion of inflammatory cytokines Macrophage activation; Secretion of inflammatory cytokines Immunoglobulins: Structure and Function Immunoglobulins:Structure and Function • Definition: Glycoprotein molecules that are produced by plasma cells in response to an immunogen and which function as antibodies General Functions of Immunoglobulins • Ag binding – Can result in protection • Effector functions (Usually require Ag binding) – Fixation of complement – Binding to various cells Immunoglobulin Structure • Heavy & Light Disulfide bond Chains • Disulfide bonds – Inter-chain – Intra-chain Carbohydrate CL VL CH2 CH1 VH Hinge Region CH3 Immunoglobulin Structure Disulfide bond • Variable & Carbohydrate Constant Regions – VL & CL – VH & CH • Hinge Region CL VL CH2 CH1 VH Hinge Region CH3 Immunoglobulin Fragments: Structure/Function Relationships Ag Binding Complement Binding Site Binding to Fc Receptors Placental Transfer IgG • Structure – Monomer (7S) IgG1, IgG2 and IgG4 IgG3 IgG • Properties – Major serum Ig – Major Ig in extravascular spaces – Placental transfer – Does not require Ag binding – Fixes complement Binds to Fc receptors Phagocytes - opsonization • K cells - ADCC IgM • Structure J Chain – Pentamer (19S) – Extra domain (CH4) – J chain C 4 IgM • Properties – 3rd highest serum Ig – First Ig made by fetus and B cells – Fixes complement Fixation of C1 by IgG and IgM Abs No activation Activation IgM • Properties – 3rd highest serum Ig – First Ig made by fetus and B cells – Fixes complement – Agglutinating Ig – Binds to Fc receptors – B cell surface Ig Tail Piece B Cell Antigen Receptor (BcR) Ig- Ig- Ig- Ig- IgA • Structure – Serum - monomer – Secretions (sIgA) • Dimer (11S) • J chain • Secretory component Secretory Piece J Chain IgA • Properties – 2nd highest serum Ig – Major secretory Ig (Mucosal or Local Immunity) • Tears, saliva, gastric and pulmonary secretions – Does not fix complement (unless aggregated) – Binds to Fc receptors on some cells IgD • Structure – Monomer – Tail piece Tail Piece IgD • Properties – 4th highest serum Ig – B cell surface Ig – Does not bind complement IgE • Structure – Monomer – Extra domain (CH4) C 4 IgE • Properties – Least common serum Ig • Binds to basophils and mast cells (Does not require Ag binding) – Allergic reactions – Parasitic infections (Helminths) • Binds to Fc receptor on eosinophils – Does not fix complement Nature of Ag/Ab Reactions • Lock and Key Concept http://www.med.sc.edu:85/chime2/lyso-abfr.htm • Non-covalent Bonds – Hydrogen bonds – Electrostatic bonds – Van der Waal forces – Hydrophobic bonds • Multiple Bonds • Reversible Source: Li, Y., Li, H., Smith-Gill, S. J., Mariuzza, R. A., Biochemistry 39, 6296, 2000 Ab formation Hallmarks of the Immune Response • Self/Non-self Discrimination • Memory • Specificity Kinetics of the Ab Response T-dependent Ag; 1o Response LAG LOG PLATEAU DECLINE Ab Titer • Lag phase • Log phase • Plateau phase • Decline phase Ag Days After Immunization Kinetics of the Ab Response • Lag phase • Log phase • Plateau phase • Decline phase Ab Titer T-dependent Ag; 2o Response 1o Ag 2o Ag * Specificity Days After Immunization Qualitative Ab Changes during o o 1 and 2 Responses • Class variation Total Ab IgG Ab IgM Ab – 2o - IgG, IgA or IgE Ab Titer – 1o - IgM 1o Ag 2o Ag Days After Im munization Cellular Events in 1o Response to T-dependent Ags • Lag – Clonal selection • Log – IgM – Class switching • Stationary • Decline • Memory Cell Pool 1o Ag IgM IgG Memory Cells Cellular Events in 2o Response to T-dependent Ags • Lag phase – Virgin cells – Memory cells Virgin B cell • Log phase – Pool size – IgG, IgA or IgE • Stationary • Decline – Sustained production IgM IgG Memory Pool Memory Cells IgG Memory Cells Cell-Cell Interactions, T-Independent Antigens, CD5 B Cells, Cytokines T Cell-B Cell Interactions (hapten-carrier effect) • Th cells recognize carrier, B cells recognize hapten • Th and B cells cooperate by interacting • Interactions are class II self-MHC restricted Uniqueness of B Cells • Express both immunoglobulin (Ig) and class II MHC on cell surface • Capable of producing antibody of same specificity as that of its surface Ig AND • Capable of functioning as an antigen presenting cell Mechanism of HaptenCarrier • Hapten recognized by Ig receptor on B cell • Hapten-carrier endocytosed • Carrier processed and presented on class II MHC to Th cell • Activated Th cell produces cytokines • Cytokines enable B cell to be activated to produce anti-hapten antibodies Antigen CD40 B MHC II cell Cytokine Immunoglobulin receptor receptor B B cell cell cell B7 CD28 2. B7 expressed 4. Cytokine binds to cytokine receptor, CD40 ligand binds to CD40 B 5. B cell activated 6. B cells proliferate, differentiate, secrete Ig TCR cell cell 1. Antigen presentation to Th cell B T helper B cell 3. Th cell is activated and expresses CD40 ligand, Cytokines secreted CD40 ligand T helper cell Cytokine Th cell Class II MHC APC B Th cell cell B cell takes up and presents antigen Th cells are primed by antigenpresenting cell Th cell Th cell B cell B-T cell cooperation B cells receive signals from T cells B B cell cell B cells divide B B B B cell cell cell cell Antibody forming cell Antibody forming cell Antibody forming cell B memory cell B Cells In Secondary Responses • Memory cells created during primary response • Have high-affinity Ig receptors • Can therefore take up antigens at much lower concentrations than other antigen presenting cells that lack Ig antigen receptors Cytokines Non-antibody proteins acting as mediators between cells, termed: • Monokines – mononuclear phagocytes • Lymphokines – activated T cells, especially helper T cells • Interleukins – abbreviated IL with a number Properties of Cytokines 1. Produced by cells involved in both natural and specific immunity 2. Mediate and regulate immune responses 3. Secretion brief and limited - not stored pre-formed - synthesis initiated by gene transcription - mRNA short-lived - cytokines produced as needed Properties of Cytokines (continued) 4. Can be produced by many cell types and act on many cell types (pleiotropic) 5. Can have similar actions (redundant) Properties of Cytokines (continued) 6. Can influence synthesis of other cytokines - produce cascades - enhance or suppress production of other cytokines - exert positive or negative regulatory mechanisms for immune responses 7. Influence action of other cytokines - can be antagonistic, additive, synergistic Properties of Cytokines (continued) 8. Bind to receptors with high affinity 9. Cells responding to cytokine can be: - same cell (autocrine) - nearby cell (paracrine) - distant cell by circulation (endocrine) 10.Cellular responses to cytokines are slow, require new mRNA and protein synthesis Mediators and Regulators of Natural Immunity • Tumor Necrosis Factor-alpha (TNF-α) • Interleukin-1 (IL-1) • Chemokines (Chemotactic cytokines) • Type I Interferons (IFN-α and IFN-β) • Interleukin-12 (IL-12) • Interleukin-10 (IL-10) Tumor Necrosis Factor (TNFα) • Produced by activated macrophages • Most important mediator of acute inflammation in response to microbes, especially Gram-negative bacteria (LPS) • Mediates recruitment of neutrophils and macrophages to site of inflammation • Acts on hypothalamus to produce fever • Promotes production of acute phase proteins Interleukin-1 (IL-1) • Produced by activated macrophages • Effects similar to those of TNF-α Chemokines • Produced by many different leukocytes and tissue cells • Large family of >50 substances • Recruit leukocytes to sites of infection • Play a role in lymphocyte trafficking Type I Interferons (IFN-α and β) • IFN-α a family of many proteins produced by macrophages, IFN-β a single protein produced by many cells • Both IFNs inhibit viral replication • Both increase expression of class I MHC • Both activate NK cells Interleukin-12 (IL-12) • Produced by activated macrophages and dendritic cells • Stimulates production of IFN-γ • Induces differentiation of Th cells to become Th1 cells • Enhances cytolytic functions of cytotoxic T cells and NK cells Interleukin-10 (IL-10) • Produced by activated macrophages, Th2 cells • An inhibitory cytokine • Inhibits cytokine production by activated macrophages • Inhibits expression of class II MHC and costimulatory molecules on macrophages Mediators and Regulators of Specific Immunity • Interleukin-2 (IL-2) • Interleukin-4 (IL-4) • Interleukin-5 (IL-5) • Interleukin-10 (IL-10) • Interferon-gamma (IFN-γ) Interleukin-2 (IL-2) • Produced by Th>>Tc • Main growth factor for T cells T cell B cell Monocyte Activation IL-2 secretion NK Stimulation of division T cell Stimulation of division and IFN gamma release (and other Increase in NK mediators) Cell activity Interleukin-4 (IL-4) • Produced by Th2 cells • Stimulates Ig class switching to IgE isotype • Stimulates development of Th2 cells from naïve Th cells • Promotes growth of differentiated Th2 cells Interleukin-5 (IL-5) • Produced by Th2 cells • Promotes growth and differentiation of eosinophils • Activates mature eosinophils • IL-4 and IL-5 can work together Helminths opsonized with IgE can be killed by activated eosinophils Interleukin-10 (IL-10) • Produced by activated macrophages, Th2 cells • Inhibits production of IFN-γ by Th1 cells needed to activate macrophages Interferon-gamma (IFN-γ) • Produced by Th cells >> Tc and NK cells • Numerous functions in both natural and specific immunity Th1 cell > Tc cell NK Granulocyte Endothelial cell Activation Activation IFN gamma secretion Macrophage NK Activation Many cell types Weak anti-viral activity, Stops cell division, Stops hematopoiesis T cell T cell activation B cell Increase in NK cell activity Many cell types Differentiation, Induction of class I Stops cell division and class II MHC Major Histocompatibility Complex and T Cell Receptor Differential expression of MHC antigens Class-I expressed on all nucleated cells in man, and also on erythrocytes in mice. Class-II expressed primarily on antigen presenting cells (dendritic cells, macrophages and B cells, etc.) Structure of Class I MHC α1 NH2 NH2 Alloantigenic sites α2 β2 NH2 COOH CHO α3 Disulfide bridge Papain cleavage Plasma membrane OH P Cytoplasm COOH Structure of Class II MHC NH2 NH2 CHO α1 β1 CHO α2 β2 CHO Plasma membrane Cytoplasm COOH COOH Aspects of MHC 1. MHC molecules are membrane- bound. Recognition by T cells requires cell-cell contact. 2. Peptide from cytosol associates with class I MHC and is recognized by Tc cells. Peptide from vesicles associates with class II MHC and is recognized by Th cells. Aspects of MHC (continued) 3. Although there is a high degree of polymorphism for a species, an individual has maximum of six different class I MHC products and only slightly more class II MHC products. A peptide must associate with a given MHC of that individual, otherwise no immune response can occur. That is one level of control. Aspects of MHC (continued) 4. Mature T cells must have a T cell receptor that recognizes the peptide associated with MHC. This is the second level of control. 5. Each MHC molecule has only one binding site. The different peptides a given MHC molecule can bind all bind to the same site, but only one at a time. Structure of T Cell Receptor Alpha chain Beta chain CHO CHO CHO CHO Variable region “V” Constant region “C” Hinge “H” Disulfide bridge + + + Transmembrane region Cytoplasmic tail Structure of T Cell Receptor (continued) • Hypervariable regions in V contribute to diversity of TCR • TCR recognizes portions of MHC molecule and peptide bound in the groove • Small population of T cells has a TCR comprised of γ and δ chains – γδ TCR specificity differs from αβ TCR Antigen Processing and Presentation What Does The B Cell Immunoglobulin (Ig) Receptor Recognize? 1. Proteins (conformational determinants, denatured or proteolyzed determinants) 2. Nucleic acids 3. Polysaccharides 4. Some lipids 5. Small chemicals (haptens) What Does the αβ T Cell Receptor (TCR) Recognize? 1. Only fragments of proteins (peptides) associated with MHC molecules on surface of cells • Helper T cells (Th) recognize peptide associated with MHC class II molecules • Cytotoxic T cells (Tc) recognize peptide associated with MHC class I molecules Antigen Processing and Presentation • Fragmentation of protein into peptides • Association of peptide with an MHC molecule • Transport to cell surface for expression • Different cellular pathways for association of peptide with MHC class I and class II molecules Class I MHC Pathway Peptide is presented by MHC-I to CD8 cytotoxic T cell Peptide passes with MHC from Golgi body to surface Plasma membrane Viral protein is made on cytoplasmic ribosomes Globular viral protein - intact Peptide associates with MHC-I complex rER Proteasome degrades protein to peptides Peptide transporter protein moves peptide into ER Golgi body Peptide with MHC goes to Golgi body MHC class I alpha and beta proteins are made on the rER Class II MHC Pathway Peptide MHC-II complex is presented to CD4 helper T cell Endosome fuses with plasma membrane Immunodominant peptide binds to class II MHC Golgi body Globular protein CD4 helper T cell Endosome Fusion of endosome and exocytic vesicle Endocytosis Lysosome Exocytic vesicle fuses with endosome releasing Ii from αβ dimer Protein is processed to peptides in endosome or lysosome Class II MHC α Synthesis 3 chains: α,β and Ii β Ii Endoplasmic reticulum Points Concerning Antigen Processing and Presentation 1. Location of pathogen • viruses in cytosol, MHC class I pathway, Tc response • extracellular bacteria, MHC class II pathway, Th2 response, Ab formation • intracellular bacteria, MHC class II pathway, Th1 response Points Concerning Antigen Processing and Presentation 2. Peptides derived from both self and non-self proteins can associate with MHC class I and class II molecules. 3. Chemical nature of MHC groove determines which peptides it will bind. Self MHC Restriction • T cells recognize foreign antigen associated with self MHC • No value for individual to have T cells that recognize foreign antigen associated with foreign MHC • Self MHC restriction occurs in thymus Process of Self MHC Restriction in Thymus • T cells with TCR recognizing self MHC molecules are retained – “positive selection” • Retained T cells with TCR recognizing self peptide associated with self MHC are eliminated – “negative selection” • Self MHC-restricted T cells are released Functions of Th Cells, Th1 and Th2 Cells, Macrophages and Tc Cells. Immunoregulation Critical Role of Th Cells in Specific Immunity • Select effector mechanisms • Induce proliferation in appropriate effectors • Enhance functional activities of effectors Ag Ag APC Antigen-presenting cell Ag Th B cell cell Cytokines Tc cell Granulocyte Macrophage Cytokines NK NK cell Functions of Th1 and Th2 Cells Th1 Th2 cell cell Inhibits production IL-10 IFNγ IL-4 IL-5 Activates Activates Macrophage Mast cell B cell Eosinophil Antibodies (including IgE) Central Role of Macrophages in Natural and Specific Immunity • Involved in initial defense and antigen presentation Invading agent Macrophage and have effector functions Antigen presentation Macrophage Activated macrophage Macrophage Th cell Cytokines Lymphokines Cytokines Anti-microbial functions Anti-tumor functions Detailed Functions of Macrophages Inflammation – Fever, Production of: IL-6, TNF-alpha, IL-1 – act as pyrogen Immunity Selection of lymphocytes to be activated: IL-12 results in Th1 activation IL-4 results in Th2 activation Activation of lymphocytes: Production of IL-1 Processing and presentation of antigen Reorganization of tissues, Secretion of a variety of factors: Degradative enzymes (elastase, hyaluronidase, collagenase) Fibroblast stimulation factors Stimulation of angiogenesis Damage to tissues Hydrolases, Hydrogen peroxide production Complement C3a TNF alpha production Antimicrobial action O2–dependent production of: hydrogen peroxide, superoxide, hydroxyl radical, hypochlorous acid O2-independent production of: acid hydrolases, cationic proteins, lysozyme Anti-tumor activity produced by: Toxic factors Hydrogen peroxide Complement C3a Proteases, Arginase Nitric oxide TNF alpha Cytolytic T (Tc) Cells • Tc exiting the thymus are pre-Tc cells, i.e. have TCR that can recognize antigen, but are not mature and cannot kill until “armed” • To become armed requires two signals: 1. Recognition by TCR of specific antigen associated with class I MHC, and 2. Exposure to cytokines (IL-2 and IFN-γ) Mechanism of Arming Tc Cells Class I MHC 1. Cell expressing class I MHC presents antigen ( ) to a pre-Tc cell 3. Th cell makes cytokines Pre-Tc cell IFN IL-2 2. Antigen-presenting cell presents antigen in association with class II MHC to Th cell T helper cell Class II MHC APC 4. Pre-Tc cell differentiates to functional Tc cell Tc cell 5. Tc recognizes antigen on class I MHC-expressing target cell 6. Target cell is killed Features of Tc Killing • Antigen-specific • Requires cell-cell contact • Each Tc capable of killing many target cells Steps in Tc Killing Tc cell Tc cell Tc cell Target cell Target cell Target cell Target cell 1. Tc recognizes antigen on target cell 2. A lethal hit is delivered by the Tc using agents such as perforin or granzyme B 3. The Tc detaches from the target cell 4. Target cell dies by apoptosis Regulation of Immune Responses • Magnitude determined by balance between the extent of lymphocyte activation and tolerance induced by an antigen • Nature determined by specificities and functional classes of lymphocytes activated • Regulatory mechanisms may act at the recognition, activation, or effector phases of an immune response