new trends in laser application in dermatology
advertisement

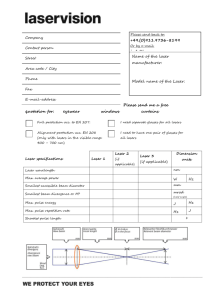
NEW TRENDS IN LASER APPLICATION IN DERMATOLOGY PRESENTED BY: Dr Shaza Mohammed Yousif MD.Dermatology 1 What is a laser? Outlines: •Laser basic •Applications of lasers dermatology and beauty therapy and new trends. •Low level laser therapy •Laser hazards Common Components of all Lasers Active Medium may be Solid crystals such as ruby or Nd:YAG, Liquid dyes, Gases like CO2 or Helium/Neon Semiconductors such as GaAs. Active mediums Contain atoms whose electrons may be excited to a metastable energy level by an energy source. 5 Excitation Mechanism Excitation mechanisms pump energy into the active medium by one or more of three basic methods; optical electrical chemical. High Reflectance Mirror A mirror which reflects essentially 100% of the laser light. Partially Transmissive Mirror A mirror which reflects less than 100% of the laser light and transmits the remainder. Fundamentals of Laser Operation 8 Lasing Action Diagram Energy Introduction Excited State Metastable State Spontaneous Energy Emission Ground State Energy is applied to a medium raising electrons to an unstable energy level. 9 These atoms spontaneously decay to a relatively long-lived, lower energy, metastable state. Lasing Action Diagram Energy Introduction Excited State Metastable State Spontaneous Energy Emission Stimulated Emission of Radiation Ground State A population inversion is achieved when the majority of atoms have reached this metastable state. 10 Lasing action occurs when an electron spontaneously returns to its ground state and produces a photon. If the energy from this photon is of the precise wavelength, it will stimulate the production of another photon of the same wavelength and resulting in a cascading effect. Optical pumping Only those perpendicular to the mirrors will be reflected back to the active medium, They travel together with incoming photons in the same direction, this is the directionality of the laser. Optical pumping The highly reflective mirror and partially reflective mirror continue the reaction by directing photons back through the medium along the long axis of the laser. The partially reflective mirror allows the transmission of a small amount of coherent radiation that we observe as the “beam”. Laser radiation will continue as long as energy is applied to the lasing Laser Output Pulsed Output (P) Energy (Watts) Energy (Joules) Continuous Output (CW) Time watt (W) - Unit of power or radiant flux (1 watt = 1 joule per second). Time Joule (J) - A unit of energy Energy (Q) The capacity for doing work. Energy content is commonly used to characterize the output from pulsed lasers and is generally expressed in Joules (J). 13 Irradiance (E) - Power per unit area, expressed in watts per square centimeter. continuous wave (CW) lasers versus pulsed lasers CW lasers has a constant power output during whole operation time. • pulsed lasers emits light in strong bursts periodically with no light between pulses• Laser Properties The light emitted from a laser is: Monochromatic, that is, it is of one color/wavelength. . Directional, that is, laser light is emitted as a relatively narrow beam in a specific direction. Coherent, which means that the wavelengths of the laser light are in phase in space and time. 15 Laser Tissues Interaction Mechanisms of laser interaction with human tissues : When a laser beam projected to tissue Five phenomena Reflection, Transmission, Scattering, Re-emission, Absorption. • • Laser light interacts with tissue and transfers energy of photons to tissue Because absorption occurs. What is a coagulation? A slow heating of muscle and other tissues is like a cooking of meat in everyday life. The heating induced the proteins, enzyme destabilization . This is also called coagulation. Like egg whites coagulate when cooked, red meat turns gray because coagulation during cooking. A Laser heating of tissues Above 50 oC but below 100oC induces disordering of proteins and other bio-molecules, this process is called photocoagulation. Applications of photocoagulation Destroy tumors Hemostatic laser surgery - bloodless incision, excision due to its ability to stop bleeding during surgery. With very high power densities, instead of cooking, lasers will quickly heat the tissues to above 100o C , water within the tissues boils and evaporates. Since 70% of the body tissue is water, the boiling change the tissue into a gas. Photo-vaporization Photo- vaporization results in complete removal of the tissue, making possible for Hemostatic incision,or excision. Complete removal of thin layer of tissue Skin rejuvenation, resurfacing Intensity requirement Resulting processes Intensity (W/cm2) High (>100) Low (<10) Photovaporization General heating Moderate (10 – 100) Photocoag ulation Photochemical ablation When using high power lasers of ultraviolet wavelength, some chemical bonds can be broken without causing local heating; this process is called photo-chemical ablation. The photo-chemical ablation results in clean-cut incision. The thermal component is relatively small and the zone of thermal interaction is limited in the incision wall. Selective absorption of laser light by human tissues Selective absorption Selective absorption occurs when a given color of light is strongly absorbed by one type of tissue, while transmitted by another. Lasers’ pure color is responsible for selective absorption. The main absorbing components of tissues are Oxyhemoglobin (in blood) the blood’s oxygen carrying protein absorption of UV and blue and green light, Melanin (a pigment in skin, hair, moles, etc): absorption in visible and near IR light (400nm – 1000nm), Water (in tissues) transparent to visible light but strong absorption of UV light below 300nm and IR over 1300nm The wavelength peaks of the laser light, pulse durations and how the target skin tissue absorbs this, determine the clinical applications of the laser types. Applications of lasers Laser in dermatology Lasers in dermatology The first lasers used to treat skin conditions occurred over 40 years ago .In the last 20 years major advances in laser technology has revolutionized their use in the treatment of many skin conditions and congenital defects. Ethincs skin laser procedures in darker skinned patients are challenging but can be successfully achieved if certain treatment guidelines are followed.. Pre- and post laser cooling can be helpful to minimize side effects and improve patients' comfort. This is especially true with laser hair removal. Photorejuvenation can be successfully achieved with low risk when appropriate settings are used. Fractional technology has increased treatment options for rhytides and atrophic scars. The 532 nm laser has proved to be risky in skin of color. On the other hand, the 1064 nm laser may offer greater safety when treating ethnic skin still risky in type VI skin. What skin conditions can be treated with lasers? Vascular lesions Vascular skin lesions contain oxygenated haemoglobin, which strongly absorbs visible light at 418, 542 and 577 nm, whereas Lasers have been used successfully to treat a variety of vascular lesions including superficial vascular malformations (port-wine stains), facial telangiectases, haemangiomas, pyogenic granulomas, Kaposi sarcoma and poikiloderma of Civatte. Lasers that have been used to treat these conditions include argon, APTD, KTP, krypton, copper vapour, copper bromide, pulsed dye lasers and Nd:YAG. Argon (CW) causes a high degree of non-specific thermal injury and scarring and is now largely replaced by yellow-light quasi-CW and pulsed laser therapies. The pulsed dye laser is considered the laser of choice for most vascular lesions because of its superior clinical efficacy and low risk profile. It has a large spot size (5 to 10mm) allowing large lesions to be treated quickly. Side effects include postoperative bruising (purpura) that may last 1-2 weeks and transient pigmentary changes. Crusting, textural changes and scarring are rarely seen. Laser removal of port-wine stain Yellow laser is absorbed by the presence of hemoglobin in blood vessels. Skin resurfacing Removal of acne scars skin wrinkles hypertrophic lesions Of lichen planus xanthelasma Seborrheic keratosis psoriasis patches C02 laser is the treatment of choice for treatment of actinic cheilitis. Facial wrinkles, scars, and sun-damaged skin Facial laser resurfacing uses high-energy, pulsed and scanned lasers. Pulsed CO2 and erbium:YAG lasers have been successful in reducing and removing facial wrinkles, acne scars and sun-damaged skin. High-energy, pulsed, and scanned CO2 laser is generally considered the gold standard against which all other facial rejuvenation systems are compared. Typically a 50% improvement is found in patients receiving CO2 laser treatment. Side effects of treatment include post-operative tenderness, redness, swelling and scarring. The redness and tenderness last several weeks, while new skin grows over the area where the damaged skin has been removed by the laser treatments (ablative laser systems). Secondary skin infection including reactivation of herpes is also a potential problem until healing occurs. Extreme caution is needed when treating darker skinned individuals as permanent loss or variable pigmentation may occur longterm. Erbium:YAG produces similar results and side effects to CO2. Despite their side effect profile and long recovery time these ablative laser systems, when used properly, can produce excellent results. Laser skin rejuvenation Recently non-ablative lasers have been used for dermal modeling; 'non-ablative' refers to heating up the dermal collagen while avoiding damage to the surface skin cells (epidermis) by cooling it. Multiple treatments are required to smooth the skin. Near-infrared 1064-nm neodymium Irradiation provides long-lasting stimulation of elastin, and thus increase elastin in the dermis, and achieve skin rejuvenation. Long-term stimulation of elastin is beneficial for improving dilated pores, skin texture, and wrinkles. Keloids and hypertrophic scars Keloids and hypertrophic scars are difficult to eradicate and traditional treatments are not always successful. Vaporising lasers (CO2 and erbium:YAG) have been useful as an alternative to conventional surgery. More recently PDL has been used to improve hypertrophic scars and keloids. This may require multiple treatment sessions or the simultaneous use of intralesional injections to gain good results. The PDL has been reported to reduce the redness as well as improving texture and pliability of the scar. Benign dermal tumors: Neurofibromas myxoid cysts granuloma faciale. Actinic keratosis squamous cell carcinoma. Other uses The CO2 laser can be used to remove a variety of skin lesions including seborrhoeic keratoses and skin cancers by vaporization or in cutting mode. However, conventional surgery or electrosurgery can also be used and is generally less expensive. Violet-blue metal halide light (407-420 nm) has been used to treat acne, because it has a toxic effect on the acne bacteria, Proprionibacterium acnes. The Excimer laser uses noble gas and halogen to produce ultraviolet radiation (308 nm) that will clear psoriasis plaques. However the small spot size and the tendency to cause blistering makes treatment time-consuming and difficult to perform. Warts treatment: of different sizes can be easily and effectively vaporized by C02 laser. It is recommended to use a magnifying lens during vaporization of warts. Warts typically bubble on evaporation . Precautions should be taken during vaporization of warts by using a special laser mask to filter wart particles during vaporization in order not to inhale the particles, which may cause infection to the surgeon. The surface of the wart is better shaved before laser vaporization to remove the dry hyperkeratotic surface, which requires much high energy because of its lower water content. Peri ungual warts can be vaporized and if the lesion is extending beneath and around the nail , the overlying nail can be evaporated to avoid nail avulsion. Pigmented lesions and tattoos Pigmented skin lesions contain melanin, which has a broad range of absorption in the : visible infrared wavebands. Melanin-specific, high energy, QS laser systems can successfully lighten or eradicate a variety of pigmented lesions. Pigmented lesions that are treatable include freckles and birthmarks including some congenital melanocytic naevi, blue naevi, naevi of Ota/Ito and Becker naevi. The short pulse laser systems effectively treat the lesions by confining their energy to the melanosomes, which are the tiny granules containing melanin inside the pigment cells. The results of laser treatment depend on the depth of the melanin and the colour of the lesion and is to some degree unpredictable. Superficially located pigment is best treated with shorter wavelength lasers whilst removal of deeper pigment requires longer wavelength lasers that penetrate to greater tissue depths. Caution is needed when treating darker-skinned people as permanent hypopigmentation and depigmentation may occur. Successfully treated lesions may recur. Prior to any laser treatment of pigmented lesions, any lesion with atypical features should be biopsied to rule out malignancy. The treatment of congenital melanocytic naevi is a controversial issue. The long-term effect of using lasers on promoting melanoma is not known but the treatment is thought to be low risk. The QS laser systems can selectively destroy tattoo pigment without causing much damage to the surrounding skin. The altered pigment is then removed from the skin by scavenging white blood cells, tissue macrophages. The choice of laser depends on the colour, depth and chemical nature of the tattoo ink. Two to ten treatments are often necessary. Yellow, orange and green colours are the most difficult to remove. Black: QS ruby, alexandrite or Nd:YAG Blue and green: QS ruby, alexandrite Yellow, orange, red: QS Nd:YAG or PDL As with other laser treatments, pigmentary and textural changes including scars may occur. Tattoo can be removed with variety of laser depending on the presence of inks in the tattoo. Laser removal of tattoo Other types of lasers such as Q-switched lasers are more efficient in removing tattoos without skin scarring Hair removal Lasers can be used to remove excessive and cosmetically disabling hair due to hypertrichosis or hirsutism. Laser treatments remove dark hair quickly and it may take 3 to 6 months before regrowth is evident. Several treatment cycles are required with the spacing between treatments dependent on the body area being treated. Laser treatments are less painful and much quicker than electrolysis. Complications are rare but superficial burns, pigmentary changes and even scarring may occur. Increased growth of fine dark hair in untreated areas close to the treated ones has been reported. Both increased and reduced localised sweating have been reported after treatment. Suitable devices include long-pulsed ruby and alexandrite lasers, diode (810nm), millisecond Nd:YAG and non-laser intense pulsed light. Laser hair removal Laser hair removal Epilation Temporary dark marks Permanent white marks Angiofibroma of lips Nevus of Ota (treated by Q-Switched Ruby laser) common acquired melanocytic nevi are largely benign, Pigment-specific lasers were initially used in the Q-switched mode, which was based on the thermal relaxation time of the melanocyte (size 7 µm; 1 µsec), which is not the primary target in melanocytic nevus. The cluster of nevus cells (100 µm) probably lends itself to treatment with a millisecond laser rather than a nanosecond laser. Thus, normal mode pigment-specific lasers and pulsed ablative lasers (CO2/erbium [Er]:yttrium aluminum garnet [YAG]) are more suited to treat acquired melanocytic nevi. The complexities of treating this disorder can be overcome by following a structured approach by using lasers that achieve the appropriate depth to treat the three subtypes of nevi: junctional, compound, and dermal. Thus, Junctional nevi respond to q-switched/normal mode pigment lasers, Compound and dermal nevi, pulsed ablative laser (CO2/ er:yag) may be needed. although melanoma is decidedly uncommon in most acquired melanocytic nevi, even though histological markers may be seen on evaluation. Keywords: lasers, surgery, nevus, melanoma Clinical classification of common acquired melanocytic nevi Macular junctional melanocytic nevi showing increased skin markings. Raised pigmented papular lesion pathognomic of a compound melanocytic nevi. Figure 4 The three stages of melanocytic nevi, with loss of pigment and eventual resolution of lesion which mirrors the “Abtropfung” theory. Reported case of fractional ablative carbon dioxide (CO2) laser treatment for of HHD. No recurrence was observed 5 months after laser therapy in right inframammary and axillary regions. Sympto- matic recurrence was noted after treatment of inguinal areas. Still traditional laser ablation remains the treatment of choice for prolonged remission of recalcitrant plaques in HHD. Nail Diseases Characteristics of laser systems used to treat onychomycosis are as follows: Wavelength: Lasers are single-wavelength light sources. There needs to be sufficient tissue penetration to adequately treat nail fungus. The near-infrared spectrum tends to be used because this is the part of the spectrum that has maximum tissue penetrance in the dermis and epidermis and the nail plate is similar to the epidermis. To date, most laser systems for treating onychomycosis have been Neodymium yttrium aluminum garnet (Nd:YAG) lasers that are typically operated at 1064nm; 940-1320nm and 1440nm wavelengths are also options. Pulse duration: Pulses need to be short to avoid damage to the tissue surrounding the target area. For example, short-pulse systems have microsecond pulse durations and Qswitched lasers have nanosecond pulse durations. Repetition rate (frequency of laser pulses, Hz): Selective photothermolysis requires that there be time between pulses to allow for dispersal of heat energy. Spot size: This refers to the diameter of the laser beam. For treating Laser Vagina Tightening patent-pending Er:YAG laser therapy for incisionless, non-invasive photothermal tightening of the vaginal canal is an efficient, easy-to-perform, and safe procedure. The indication is vaginal relaxation syndrome, which is the loss of the optimum structural form of the vagina. This condition is generally associated with overstretching of the vaginal canal during childbirth as well as with natural aging. How does It work? Wave length 2940 nm Er:YAG non-ablative laser with proprietary “Smoothmode” technology thermally affects the vaginal tissue, stimulating collagen remodeling and the synthesis of new collagen fibers in the vaginal mucosa tissue and collagen-rich endopelvic fascia. The final result of collagen neogenesis and remodeling is tightening of the vaginal canal. Clinical results show a tightened vaginal canal, greater sexual satisfaction and significant improvement in a patient’s quality of life. Usually two sessions are recommended. No special pre-op preparation or postop precautions are necessary. Patients can immediately return to their normal Laser lipolysis Laser lipolysis is a therapeutic modality that is currently used to treat localized fat and promote cutaneous retraction Applying laser directly to adipose tissue causes fat liquefaction, blood vessel coagulation and collagen denaturation. The thermal damage induces neocollagenesis and skin contraction Cut leishmaniasis LLLT is a complementary form of treatment Where it acts ? 88 10/31/2012 Where it acts ? (Continues` Laser Tissue Interactions: Photochemical Interaction The laser energy is absorbed by metabolically active pigments of the mitochondria in various cutaneous and subcutaneous layers: Here involved are the two enzymes of the oxidation chain, Cytochrome a/a3 and Flavoprotein with absorption maxims of wavelengths applied. It is supposed that the changes in the stereochemical conformation induced by an electro magnetic field leads to an increase in activity and improves the concentration of ATP by up to 200%. In addition, an increase in oxygen and glucose metabolism is observed. The main effect is an optimized function of the Na-K pump at the cell membrane, an increased protein synthesis (prostaglandin, enzyme) and a significantly higher rate of mitosis. Cellular Activities Increased cell metabolism (Increased cell function) Increased collagen synthesis (Increased healing of soft tissues) Increased osteoblast production (Increased healing of bone) Increased circulation Increased formation of new capillaries (tiny blood vessels) by release of growth factors Increased T-cell production (Increased immune function) Increased production of neurotransmitters such as endorphins, serotonin, ACTH etc. (Increased nerve function) Increased chronic pain threshold through decreased C-fiber activity (Decreased pain). Physiological Effects of Laser Accelerated tissue healing and repair by 40% Increased tensile strength in tissue repair Increase callous and bone formation Reduced or eliminated pain Decreased edema and inflammation Improved immune response Stimulates nerve function Promotes Cellular Oxygenation/Detoxification. Subsides inflammation by: Stabilization of cellular membrane ATP production and synthesis Vasodilatation is stimulated via Histamine, Nitric Oxide (NO) and Serotonin. Acceleration of leukocytic activity. Increased Prostaglandin synthesis, Reduction in Interleukin 1(IL-1). Enhanced lymphocyte response. Increased angiogenesis. Temperature modulation. Enhanced superoxide dismutase(SOD) levels. Decreased C-reactive protein and neopterin levels. Reduces pain by: Increase in b-Endorphins. Blocked depolarization of C-fiber afferent nerves. Increased nitric oxide production. Increased nerve cell action potential. Axonal sprouting and nerve cell regeneration. Decreased Bradykinin levels. Increased release of acetylcholine. Ion channel normalization. Reduces healing time by: Enhanced leukocyte infiltration. Increased macrophage activity. Increased neovascularization. Increased fibroblast proliferation. Keratinocyte proliferation. Early epithelialization. Growth factor increases. Enhanced cell proliferation and differentiation. Greater healed wound tensile strength. Laser Hazards 96 Types of Laser Hazards Eye : Acute exposure of the eye to lasers of certain wavelengths and power can cause corneal or retinal burns (or both). Chronic exposure to excessive levels may cause corneal or lenticular opacities (cataracts) or retinal injury. Skin : Acute exposure to high levels of optical radiation may cause skin burns carcinogenesis may occur for ultraviolet wavelengths (290-320 nm). Chemical : Some lasers require hazardous or toxic substances to operate (i.e., chemical dye, Excimer lasers). 97 Electrical : Most lasers utilize high voltages that can be lethal. Fire : The solvents used in dye lasers are flammable. High voltage pulse or flash lamps may cause ignition. Flammable materials may be ignited by direct beams or specular reflections from high power continuous wave (CW) infrared lasers. Laser hazards and protections The retina The directionality of a laser beam permits the ray to be focused to an extremely small spot on the retina. A collimated laser will be concentrated by a factor of 100,000 when passing from cornea to retina. Visible or near IR lasers (400 nm to 1400nm) are particularly dangerous to the retina and always requires eyeprotection when working with these kind of lasers. Hazards to the eye The cornea and lens Cornea is accessible to danger of UV and most of IR lasers, UV-A, UV-B (between 295nm and 320 nm) and IR-A (between 1 to 2 mm) are dangerous for lens, 308-nm (UV-B) excimer XeCl laser is particular dangerous because of it can simultaneously damage the lens, the cornea and the retina. Lasers and Eyes What are the effects of laser energy on the eye? Laser light in the visible to near infrared spectrum "retinal hazard region". (i.e., 400 - 1400 nm) can cause damage to the Retina resulting in scotoma (blind spot in the fovea). Laser light in the ultraviolet (290 - 400 nm) or far infrared (1400 10,600 nm) spectrum can cause damage to the Cornea and/or to the Lens. Photoacoustic retinal damage may be associated with an audible "pop" at the time of exposure. Visual disorientation due to retinal damage may not be apparent to the operator until considerable thermal damage has occurred. 101 Laser Class The following criteria are used to classify lasers: Wavelength. If the laser is designed to emit multiple wavelengths the classification is based on the most hazardous wavelength. For continuous wave (CW) or repetitively pulsed lasers the average power output (Watts) and limiting exposure time inherent in the design are considered. For pulsed lasers the total energy per pulse (Joule), pulse duration, pulse repetition frequency and emergent beam radiant exposure are considered. 102 CONTROL MEASURES Eye protection Eyewear (goggles) is the most common laser protective measure, especially for open laser beams. It should be good design with all around shielding and adequate visible light transmission. Engineering Controls Interlocks Enclosed beam Administrative Controls Identification of the eyewear : All laser protective eyewear shall be clearly labelled with information adequate to ensure the proper choice of eyewear with particular lasers. Standard Operating Procedures (SOPs) Training Personnel Protective Equipment (PPE) Eye protection 103 Common Laser Signs and Labels 104