common infections of childhood
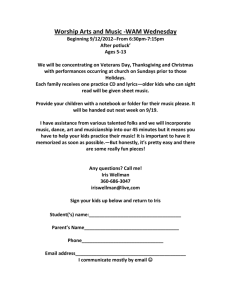
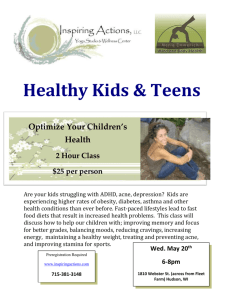
advertisement

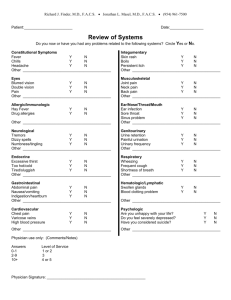
Jen Avegno, MD LSU – New Orleans Emergency Medicine 2006 National Hospital Ambulatory Medical Care Survey showed: most common ED diagnosis for kids <1 = upper respiratory infection kids 2-12 = otitis media/ear disorders In all, fever is the most common chief complaint of kids presenting to the ED (about 20-30% all peds visits) this lecture is about NOT Review pediatric fever guidelines Discuss some common infections in childhood See LOTS of pictures of cute kids! Mom brings in a 3-week-old baby girl with a fever for 4 hours. The child was a normal vaginal delivery with no complications and has been feeding and growing well at home. This morning, she began to “spit up” her bottle and had several loose stools. She has been somewhat sleepy but does respond to her parents. Physical exam reveals a child in no distress with a rectal temperature of 100.8 and a normal exam for age. what is the risk of serious bacterial illness (SBI) in kids less than 3 months with fever? SBI = UTI, bacteremia, meningitis, osteo, pneumonia, gastroenteritis, cellulitis, septic arthritis risk is about 6-10% in these kids, with those younger than 1 month having the highest chance of SBI kids under 3 months may present looking like “viral syndrome” but still have SBI … in one study, kids less than 60 days with temp>38: 22% had RSV 7% with RSV also had concomitant SBI immature immune system exposure to pathogens during delivery (esp. GBS) cannot mount immune response to prevent localized infection from disseminating fever = “a pyrogen-mediated rise in body temperature above normal range” what is a NORMAL temp? the magical 98.6 was set as “normal” by a German guy in the 19th century using a 22cm long mercury glass thermometer … we now think that his instruments may have been OFF by 1.5-2 degrees!! normal temps can vary by age in kids from 99.5 (neonates) to 98 (older kids) temps are influenced by age, sex, race, time of day, activity level, ambient temp, site of measurement, type of device NO REAL EVIDENCE to support the hardand-fast cutoff of 100.4 (38°C) – evidence suggests that oral temps 37.237.8 may be considered febrile depending on situation BEST SITE to measure temperature … the hypothalamic artery. (yeah, right) take-home point: fever is an ARBITRARY number – base your workup on overall clinical impression, not a particular cutoff oh, yeah, the “mom hands” … don’t blow them off! 60% of parents use their hands instead of a thermometer to assess fever is this method accurate? studies show: 74-90% sensitive 76-86% specific 85-94% NPV the exact number or method doesn’t matter … BELIEVING the parents is! AGE BACTERIAL VIRAL OTHER 0-28 days Group B Strep Listeria E. Coli C. trachomatis N. gonorrhoeae Herpes simplex Varicella Enterovirus RSV Flu Bundling environment 1-3 months H. flu S. pneumo N. meningiditis E. coli Varicella Enterovirus RSV flu Bundling environment length of illness localized symptoms? pertinent PMH, birth hx of both mom & baby sick contacts vaccination status any meds/ABx VITAL SIGNS (yes, ALL of them!!) ABCs – respiratory/airway distress? signs of shock? tachycardia? for infants less than 1 year, HR should increase 10 beats for every 1°C TAKE THOSE CLOTHES OFF!! just remember … in non-immunocompetent kids (neonates) … fever may be the ONLY presenting sign of SBI – do not be reassured by a “normal” exam!! again, ABCs … consider intubation for respiratory distress, hypoxia, altered MS fluid resuscitation: 20 ml/kg IV/IO fluids to total of 60-100 ml/kg (if hypovolemia persists) cultures prior to Abx, if possible sterilization of CSF can occur as quickly as 15 min – 2 hrs after receiving Abx, so watch results! BROAD SPECTRUM TREATMENT: Ampicillin + (Gentamycin or Cefotaxime) – avoid Rocephin in kids <28 days Vanc? Acyclovir? PHILADELPHIA ROCHESTER BOSTON AGE 29-60 d <60 d 28-89 d TEMP >38.1 >37.9 >37.9 EXAM well, no focus well, no focus well, no focus LAB VALUES (lowrisk) WBC <15 Band<0.2 UA < 10 wbc CSF < 8 wbc neg CXR WBC 5-15 band <1500 UA <10 wbc WBC <20 HIGH-RISK dispo admit, IV Abx admit, IV Abx admit, IV Abx LOW-RISK dispo home, no Abx home, no Abx home, empiric Abx How good is it?? sens/spec PPV/NPV 98%/42% 14%/99.7% 92%/50% 12%/98.9% NPV 94.6% ** these rules miss very few kids with SBI ** UA <10 wbc CSF <10 wbc neg CXR cancer toxic shock autoimmune and/or congenital disorders (cardiac, pulmonary) Dad comes to the ED with little Maria, age 2, and reports that she has had a fever for the last 2 days (up to 103.4 at home). The parents have tried Tylenol and Motrin to no avail. Maria has not eaten much but is still drinking water and juice. She had a “runny nose” a few days ago, but is not sneezing, coughing, or vomiting. In the ED, Maria has a temperature of 102.8. She looks droopy, but interacts well with her parents. fever is the most common complaint in this age group!! unlike neonates, of young children who present with viral illness (RSV, croup, bronchiolitis etc) and fever (>39), less than 0.5% will also be bacteremic concern here is for OCCULT BACTEREMIA before HiB and Prevnar, the rate of occult bacteremia in the non-focal febrile child was 5% currently … it is less than 1% with other pathogens more prevalent N. meningiditis urinary pathogens WHY do we treat a fever? feel better/decrease anxiety lower morbidity/mortality prevent febrile seizures HOW do we treat a fever? ambient temp control light clothing/bedding fluids sponge bath warm feet/potatoes or onions in socks (REALLY!) antipyretics Acetaminophen 15 mg/kg every 4-6 hours Ibuprofen 10 mg/kg every 6 hours alternate?? evidence shows some minor benefits in reducing fever faster and lasting longer BUT … potential for dosage/scheduling errors; synergistic renal toxicity; difficult to understand and comply detailed information/handout at appropriate reading level on administration of antipyretics should be given to caregivers!! AGE BACTERIAL VIRAL OTHER 3-36 months S. pneumo N. meningiditis E. coli Varicella Enterovirus RSV Flu Mono Roseola Adenovirus Norwalk Coxsackie Leukemia Lumphoma Neuroblastoma Wilms’ tumor length of illness localized symptoms? headache – neck pain – sore throat – pulling @ ears – cough (describe!!) – wheeze – vomiting – RASH – mental status use of antipyretics (**defervesence after use does NOT exclude bacteremia!) sick contacts po intake/output vaccination status any meds/ABx VITAL SIGNS (yes, ALL of them!!) ABCs – respiratory/airway distress? signs of shock? tachycardia? capillary refill is an easy and reliable indicator of perfusion TAKE THOSE CLOTHES OFF!! thorough search for focal findings most guidelines argue for getting the WBC first, then CXR if WBC > 20k … but who does this? study showed that rate of pneumococcal bacteremia increased to 0.5% with WBC 10-15k; 3.5% with WBC 15-20k; 18% with WBC>20k ANC >10k (include all immature forms) increases risk of bacteremia by 10-fold over those with ANC<10k the post-immunization world has resulted in much lower rates of bacteremia for this age group: where bacteremia rates in febrile kids >1.5%, the most cost-effective strategy is a WBC, blood CX, and empiric Abx (Rocephin) when rates <0.5%, clinical judgment alone for treatment & management is most useful to select out high-risk groups kids 3-6 mo are still relatively nonimmunocompetent … recommendations are for all kids in this age group with temp >39 to have WBC & BCx; treat all WBC > 15k with empiric ABx CANCER autoimmune disease: JRA, Kawasaki’s brain tumors Mom brings in a 15-month old girl who woke up last night screaming and with fever to 101.2. She has not eaten much today but is drinking liquids with normal urine output. All of her immunizations are up to date and she is otherwise healthy. On exam, you note a mildly ill appearing, non-toxic child who responds well to mom. The left TM is red and bulging with loss of landmarks. Most commonly diagnosed disease in kids <15 By age 3 – estimated that more than 80% of kids have had one episode; 40% have had >3 Risk factors: Male Smoking Day care Family history Anatomic abnormalities Winter Bottle feeding ACUTE: s/s of acute infxn WITH effusion OME: effusion WITHOUT s/s of acute infxn aka “acute suppurative” or “prurulent” OM aka “serous,” “mucoid,” “secretory,” “nonsuppurative” CHRONIC: chronic ear discharge from perforated membrane RECURRENT: >3 episodes in 6 mo or >4 episodes in 1 year It’s all about the tube – functions of the eustachian tube: Ventilates middle ear for pressure equilibration Drains middle ear Protects ear from NP secretions Only open when yawning/chewing/swallowing CHILD When the eustachian tube becomes obstructed … Middle ear ventilation Negative middle ear cavity pressure causes fluid to move into middle ear (transudate)and combine with NP secretions & bacteria •S. Pneumoniae •H. flu –higher % in OME •M. catarrhalis •S. aureus •S. pyogenes •gram-negative bacteria •VIRUSES: “Pulling at ears” Cough Vomiting & diarrhea Decreased po intake Fever – may be present in only ¼ of cases, with less than 10% having temp >40 URI sx pars flaccida malleus pars tensa umbo eustachian tube opening light reflex What does the TM look like? bulging erythematous hemorrhagic normal Middle ear effusions other indicators of AOM: lack of TM mobility *** (MOST RELIABLE SIGN) cloudy, retracted, dull TM 1/3 of cases may NOT have symptoms! AAP/AAFP guidelines state that the following should be present to dx AOM: 1. 2. 3. Recent, usually abrupt onset of s/s Presence of middle ear effusion (bulging, limited TM mobility, air-fluid level, otorrhea) S/s of middle ear inflammation (erythema or otalgia) AAP guidelines on management of AOM in kids: Dx by hx of acute onset + signs of effusion + signs of middle ear inflammation Assess for pain – if present, treat Limited role for observation in select patients > 2 years (must have “a ready means of communication with clinician”) If treat with ABx – start with amox 80-90 mg/kg/day If treatment failure by 48-72 hours – reconsider dx or change ABx Temp <39.1 or severe otalgia or BOTH Initial Tx Clinical failure after 48-72 hrs with initial tx NO Amox 80-90 mg/kg/day PCN all: cefdinir, cefuroxime, cefpodoxime, azith, clarith Augmentin 90 mg/kg/day (of amox) PCN all: Rocephin (3 day tx), clinda YES Augmentin 90 mg/kg/day (of amox) PCN all: Rocephin (1-time or 3 day tx) Rocephin (3 days) PCN all: clinda + tympanocentesis Important points: “treatment failure” = lack of clinical improvement and/or persistent signs of AOM Bactrim & macrolides often considered 2nd line, but resistance rates approach 30-40% Courses are generally 10 days in patients < 2 yrs , perf TM, and recurrent OM, recommended in patients <6 years NO INDICATION for antihistamines, decongestants, steroids, or tubes in single episode AOM Auralgan may be useful for pain relief Tx of OME (either alone or following episode of OM) is controversial – ABx? Antihistamines? Tubes for patients with OME for 4-6 months, failed tmt, and hearing loss otitis externa mastoiditis Parents bring an 8 year old boy to the ED with fever of 102.3, and complaints of headache and abdominal pain. He was otherwise healthy until this morning, and his shots are all up to date. The patient is febrile and tachycardic to 120 with normal blood pressure. He is ill-appearing but nontoxic, speaks normally, and is not drooling. His oropharynx is red with bilateral white exudates and tender, palpable cervical lymphadenopathy. dx of tonsillitis/acute pharyngitis is made more than 7 million times/year MCC is viral in kids MCC bacterial pharyngitis is GABHS (15-30%) kids 5-15 y/o predominantly Group C & G Strep are likely much more common than typically thought & may be missed by routine testing about 1 in 4 kids with acute sore throat has serologically confirmed GABHS MC in winter when respiratory viruses predominate BACTERIAL: Strep Group A Groups C & G mixed anaerobic (“Vincent’s angina”) N. gonorrhoeae C. diphtheriae Arcanobacterium haemolyticum; Yersinia; tularemia atypicals VIRAL: rhino, corona, adeno, paraflu, flu, CMV; HSV 1 & 2 – oral gingivostomatitis Coxsackie – aka herpangina – fever & painful, white-gray papulovesicular lesions/ulcers in posterior OP EBV - **mono** severe pharyngitis with GENERALIZED LAD (posterior cervical), hepatosplenomegaly, periorbital edema, palatal petechiae Amoxil rash!! HIV** may be most common presenting sx! herpangina diphtheria HSV stomatitis weird looking throats Vincent’s angina sick contacts – common in both bacterial & viral causes how to differentiate viral vs. bacterial sore throat? BACTERIAL (GABHS) VIRAL Sudden onset More gradual + fever +/- fever headache conjunctivitis N/V/abd pain diarrhea Tender anterior LAD Cough, hoarseness, coryza Patchy discrete exudates myalgias Scarlatiniform rash single throat swab & culture is 90-95% sensitive; rapid kits are 90-99% Modified Centor criteria for dx of GABHS in kids: tonsillar exudates tender anterior cervical LAD or lymphadenitis absence of cough SCORE RISK OF MGT GABHS hx of fever 0 1-2.5% No testing or Abx age < 15 add 1 point 1 5-10% 2 11-17% 3 28-35% Culture; Abx for + results 4-5 51-53% Tx without test most common viral causes are self-limited and resolve with supportive tx GABHS is generally self-limited and resolves without tx … but … why do we treat with Abx? symptom relief; decrease spread; shorten duration of illness (16 hrs) prevent complications (1 in 1000) suppurative – bacteremia, endocarditis, mastoiditis, meningitis, OM, PTA, RPA, pneumonia nonsuppurative – PSGN, RF Abx options: Pen V K po or Pen G IM Amox PCN allergy – Keflex, Azithromycin (resistance rates near 10% thanks to us!) supportive measures – antipyretics, warm salt water gargles, cool soothing fluids, etc. mono retropharyngeal abscess peritonsillar abscess (older adolescents) epiglottitis (more common in adults now) scarlet fever – caused by pyrogenic exotoxinproducing form of GABHS in non-immune individuals outbreaks are cyclical rash 24-48 hours after onset of symptoms (may be longer) kids will be kids and get SICK fortunately, most of the time they are not TOO SICK (let us all say a prayer of thanks to the guy(s) who invented vaccines) when you hear hoofbeats … it’s OK to consider a zebra, as long as the herd of horses doesn’t trample you while you’re thinking …