Pesticide Exposure

The Health of
Farmworkers-Pt. 2
Marc Schenker M.D., M.P.H.
• Dept. Public Health Sciences, University of California at Davis
• Director, Western Center for Agricultural Health and
Safety
Part II
****
Acute Injuries and Fatalities of Farmworkers
Outline
• The hazardous passage
• Occupational fatalities among agricultural workers
– Animal
– Machine/tractor
– Transportation
• Fatalities of children
• Pesticides
Causes of Death Among Latin
Immigrants Crossing US Border
• During the crossing
– Exposure
– Drowning
– Accidents
– Murder
• After the crossing
– Disease
– Injury (occupational)
U.S.-Mexico Border: The Season of
Death
“The deaths trickle in over the cooler months. A couple here from a rollover. Four dead there during a cold snap. They begin in earnest once the temperature spikes over
100 degrees sometime in May.”
PBS Frontline, June 27, 2006
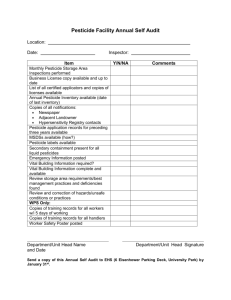
Occupational Fatalities in
Agriculture
SOURCE: U.S. Bureau of Labor Statistics, U.S. Department of Labor, 2007
Occupational fatality rates by age group for farming, 1992-2004*
* Excludes New York City. Rates calculated by NIOSH and may differ from BLS.
Agriculture Fatality Rate vs.
Private Sector, US, 1992 - 2002
Children : The Forgotten
Farmworkers
“Farmers and Labor
Contractors say they allow children to perform field work because the grower needs to get the crop in, parents need the money or children would learn the value of working.”
Fresno Bee, 12/14/92
José (22) and Angelica Alatorre and son
Guillermo. Jose died while working in a manure pit at Aguiar-Faria & Sons Dairy, Gustine, CA.
February 22, 2001
Pesticide Toxicology
• Many toxin categories
• Affect various organs
• Varied health effects
Diagram illustrating various pesticide-related health effects.
Definition of Pesticide
“Any substance or mixture of substances intended for preventing, destroying, repelling, or mitigating any insects, rodents, nematodes, fungi, or weeds, or any other forms of life declared to be pests; any substance or mixture of substances intended for use as a plant regulator, defoliant, or desiccant.”
-Federal Insecticide, Fungicide, and Rodenticide Act (US
EPA, 1947)
US Pesticide Use
• 4.5 billion pounds chemicals per year
– 890 active ingredients,
30,000 formulations
– Uses
• 75% agricultural
• 25% home, garden, structural
Agricultural Pesticide Use
• High volume:
– Hand labor (Western states)
• Vineyards
• Orchard, row vegetables, nursery
• Low volume:
– Mechanized (Midwest states)
• Livestock insecticide dipping
• Grain agriculture
Pesticide Exposure:
Occupational Settings
• Multiple industries
– Agriculture
– Emergency response
– Maintenance
– Transportation
• Variety of workers
– Applicators, fieldworkers
– Firefighters
– Medical personnel
– Flight attendants
NEETF 2002
Pesticide Exposure:
Environmental-Occupational Interface
• Drift
– Off-target physical movement of pesticide through air
• Take-home
– Contaminated clothing
– Pesticide containers brought home
Pesticide Exposure:
Environmental Settings
• Use in schools
• Lawn, garden use
• Household cleaning
• Home pesticide use
• Residues in food
Pesticide Exposure:
Accidental Ingestion
• Improper storage or mislabeling of containers
• Prescription pesticides resembling oral medications
Pesticide Exposure:
Suicide/Homicide
• Unknown substance
• Secondary exposure
San Francisco Chronicle Monday, Ja nuary 17, 2000
Coroner Identifies Man Who Swa llowed Pesticide
Unintentional Pesticide Illness, USA
Toxic Exposure Surveillance System 1993-1996
100000
10000
1000
100
10
1
D isi nf ec ta nt s
Fu m ig an ts
Fu ng ic id es
H er bi ci de s
In se ct ici de
R s od en tic id es
Minor
Moderate
Major
Fatal
Illness severity
Pesticide Illness
Rates Vary by Occupation
Organophosphate pesticide poisoning rates by agricultural sector
California, 1982--1990
Source: HS-1688, Cal EPA
Pesticide Illness Around the World
Annual rates of intentional and unintentional pesticide-related fatalities and hospitalizations in several countries
100 0
800
600
400
200
0
Costa
Rica
Sri
Lan ka
Sweden
U.K.
U.S.A.
Hospi tali za tion s
Fatalities
US EPA Toxicity Classification
(Systemic toxicity, eye irritation, skin irritation)
• Class I: “Danger”
– Fatal if ingested; corneal opacity; corrosive to skin
• Class II: “Warning”
– May be fatal if ingested; reversible corneal opacity; severe skin irritation
• Class III: “Caution”
– Harmful if ingested; no corneal opacity; moderate skin irritation
• Class IV: “Caution”
– May be harmful if ingested; no eye irritation; mild/no skin irritation
Common Components of
Pesticide Formulations
• Technical grade chemical (active ingredient)
• Adjuvants/synergists
• “Inert” ingredients
– e.g., formaldehyde, sulfuric acid, benzene, toluene, other organic solvents
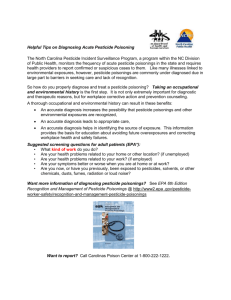
Diagnosis of Pesticide Illness
• Exposure history most important
– Occupational and environmental history
– Duration, dose, route of potential exposure
• Symptom review
• Physical exam & lab findings
• Health effects may be due to any component of pesticide formulations
Commonly-used Acronyms for
Cholinesterase Inhibition Syndromes
• S alivation
• L acrimation
• U rination
• D iarrhea
• D iarrhea
• U rination
• M iosis
• B ronchorrhea
• E mesis
• L acrimation
• S alivation
41
Cholinesterase Inhibitors
Clinical Presentations Vary
• Some signs & symptoms may be absent
– Bronchorrhea more likely with high-dose exposures (ingestion)
• Common presentations
– Nausea, vomiting
– Miosis
– Sweating, urinary frequency
– Non-specific constitutional symptoms
42
Aspects of History that Suggest
Pesticide Illness
• Multiple cases
– Similar symptoms, exposure history
• History of chemical application
– Home or office
• Accidental ingestion, esp. children
• Suicide, homicide attempts
Pesticide Illness
Nonspecific Symptoms & Signs
• Rash
• Flu-like symptoms
– Dizziness, malaise, respiratory tract irritation
• Gastrointestinal symptoms
• Seizures
• Odor-related effects
– Not toxicological effects of active ingredient
Pesticide Illness May Mimic
Common Medical Conditions
• Mild
:
– Upper respiratory tract infection/influenza
– Food-borne illness
– Asthma
– Plant-induced irritant or allergic dermatitis
• Severe
:
– Cerebrovascular accident
– Psychiatric dysfunction
– Heat stroke
How to Identify Pesticides
• Application records
• Label
• Material Safety Data Sheet
• www.msdsonline.com
• http://www.ilpi.com/msds/index.html
Sources of Pesticide Information
• Internet
– EXTOXNET: http://ace.orst.edu/info/extoxnet/
– California Department of Pesticide Regulation: http://www.cdpr.ca.gov/docs/label/labelque.htm
– Pesticide Action Network: http://www/pesticideinfo.org/index.html
• Textbooks
– US EPA. Recognition and Management of Pesticide Poisonings. 1999; 5 th ed. http://www.epa.gov/pesticides/safety/healthcare
– R Krieger (ed). Handbook of Pesticide Toxicology. 2001; 2 nd ed.
• Poison Control Centers: 1-800-222-1222
• National Pesticide Information Center (NPIC):
1-800-858-7378 or npic@ace.orst.edu
Treatment of Pesticide Illness
Decontamination
• Shower, shampoo
– Scrub under fingernails
• Contain contaminated clothing, body fluids
– Save for residue analysis
• Protect treating staff
– Body fluid precautions
– Personal protective equipment if appropriate
Pesticide Illness
Medical Treatment
• Symptomatic treatment
– Respiratory distress
• Maintain airway, breathing, circulation
• Oxygen, bronchodilators if indicated
– Ingestion
• Gastric lavage, charcoal if indicated
• Specific antidotes where applicable
Poison Control Centers
• Toxicity
• Decontamination
• Management
• Reporting
Case
Applicator with Gastrointestinal Illness
• 27 year-old pesticide applicator with dizziness, headache, body ache, nausea and vomiting. Sprayed Carzol yesterday.
• Exam: Weak (not flaccid), oriented; orthostatic hypotension; exam otherwise normal.
• Cholinesterase normal compared to laboratory reference range
Applicator with Gastrointestinal Illness
Discussion
• Differential etiology of gastroenteritis
• Pesticide-related
• Food-borne
• Viral
• Test results confirm clinical suspicions
– Normal results do not rule out exposure
– Treatment based on symptoms
Case
Farmworker with Multiple
Symptoms
• 66 year-old male with eye irritation, abdominal pain, nausea, vomiting, headache, dizziness, frequent urination, muscle shaking. Symptoms began after weeding a cotton field for 4 hours.
• Occasional palpitations but no other symptoms over the past 6 months
• 33 other crew members complain of similar symptoms
53
Farmworker with Multiple Symptoms
Exposure History
• 4:00 am: Aerial application of
– Carbofuran (N-methyl carbamate)
– Abamectin (macrolytic lactone)
– Mepiquat chloride (growth regulator)
• 6:00 am: Workers entered field
• 10:00 am: Symptoms
54
Farmworker with Multiple Symptoms
Physical Exam
• Nausea & abdominal pain
• Conjunctival injection
• Irregularly irregular pulse; rate
106-155,
• Lungs clear, no murmurs; neurological exam normal
This warning sign was posted after the workers entered the field and became ill.
55
Pyrethroid Insecticides
• Use increasing
• Examples of use
– Structural & agricultural
– Pet flea control
– Pediculicide
• Vector control
– West Nile virus
– Aircraft “disinsection ”
56
Source: CDC
Pyrethroids: Health Effects
Skin
Paresthesia, dermatitis
Respiratory
Rhinitis
Systemic
Dizziness, headache
Fasciculations, seizures,
Hormonal disruption in vitro
57
Pyrethrin & Pyrethroid Illness:
Treatment
• Decontamination
• Vitamin E cream
• Symptomatic therapy
• Remove from further exposure if needed
58
Case
Woman Exposed to Flea Bomb
• 35 year-old non-pregnant female with skin burning, itching and chest tightness after putting on clothes from closet.
• Physical exam
– Arms and face bright red
– Vital signs normal
– Lungs clear
59
Woman Exposed to Flea Bomb
Ingredients
• Label
– 0.435% permethrin
– 0.05% pyrethrins
– 0.4% piperonyl butoxide
– 99.115% inert ingredients
• Recommended no entry for 4 hours after fogging
60
Fumigants
• Halogenated hydrocarbons
– Methyl bromide
– Ethylene dibromide, DBCP
• Inorganic compounds
– Sulfuryl fluoride
• Pro-fumigants
– Metam sodium
• Metal phosphides
– Aluminum, Zinc, Magnesium
61
Fumigants
Methyl Bromide
• High vapor pressure
• Heavier than air
• Odorless
– Chloropicrin added
• Toxic mechanism
– Tissue methylation
Br
H
C
H
H
62
Pesticide Availability in Mexico
Pesticide Illness: Summary
• Occupational, environmental history
• Clinical suspicion
• Tests supplement clinical diagnosis
• Treatment symptomatic, few exceptions