On the CUSP: Stop BSI - Health Research & Educational Trust
advertisement

On the CUSP: Stop CAUTI
Content Call #5 :
Prevention of CAUTI: The View from the Bedside
Cohort 2
May 3, 2011: 1 ET/12 CT/11 MT/10 PT
Russ Olmsted, MPH, CIC
Director, Infection Prevention & Control Services
Saint Joseph Mercy Health System, Ann Arbor, MI
1
CAUTI Content Call Schedule
CUSP/CAUTI Content Call #1 – CUSP
Moderator – Sam Watson; Speaker – Sean Berenholtz
03/07/11
2 ET/1 CT/12 MT/11 PT
Attendee: (866) 256-9295
CUSP/CAUTI Content Call #2 - The Science of Safety
Moderator – Sam Watson; Speaker – Sean Berenholtz
03/22/11
2 ET/1 CT/12 MT/11 PT
Attendee: (866) 256-9295
CUSP/CAUTI Content Call #3 - Care and Removal Intervention
Moderator – Sam Watson; Speaker – Mohamad Fakih
04/05/11
2 ET/1 CT/12 MT/11 PT
Attendee: (866) 256-9295
CUSP/CAUTI Content Call #4 - Data Collection
Moderator – Sam Watson; Speaker – Sam Watson
04/19/11
2 ET/1 CT/12 MT/11 PT
Attendee: (866) 256-9295
CUSP/CAUTI Content Call #5 - The View from the Bedside
Moderator – Sam Watson; Speaker – Russ Olmsted
05/03/11
2 ET/1 CT/12 MT/11 PT
Attendee: (866) 256-9295
CUSP/CAUTI Content Call #6 - Implementation in a Community Hospital
Moderator – Sam Watson; Speaker – Mary Jo Skiba
05/17/11
2 ET/1 CT/12 MT/11 PT
Attendee: (866) 256-9295
2
60 Min.
60 Min.
60 Min.
60 Min.
60 Min.
60 Min.
Overview of Today’s Call
• Overview of External Factors Impacting Prevention of
CAUTI
• How are we doing with CAUTI Prevention Intervention?
A National Survey
• From the Bedside: One Infection Preventionist’s
Experience with CAUTI Prevention Collaborative
3
Project Goals
• Reduce CAUTI rates in participating units by 25%
– Appropriate placement
– Appropriate continuance
– Appropriate utilization
• Improve patient safety culture on participating
units
4
Pathogenesis of CA-UTI
• Source: colonic or perineal flora
or hands of personnel
• Microbes enter the bladder via
extraluminal {around the
external surface} (proportion =
2/3) or intraluminal {inside the
catheter} (1/3)
• Daily risk of bacteriuria with
catheterization is 3% to 10%; by
day 30 = 100%
– Maki DG EID 2001
5
Facts & Figures on CAUTI According to
Rodney…”these just don’t get any respect!”
• Increased morbidity, mortality (attributable mortality
= 2.3%), hospital cost, and length of stay
• 15% - 25% of hospitalized patients may receive
short-term indwelling urinary catheters
• 17% to 69% of CAUTI may be preventable with
recommended infection prevention measures
– Up to 380,000 infections and 9000 deaths related
to CAUTI per year could be prevented
• Gould CV, et al. Guideline for prevention of CAUTIs, 2009
6
Snapshot of Relative Distribution of
Health Care-Associated Infections (HAIs) in U.S.
hospitals, 2002
263,810
274,098
-967
-21
-28,725
244,385
TOTAL
HRN
WBN
Non-newborn ICU
= SSI
Other
22%
133,368
BSI
11%
SSI
20%
PNEU
11%
129,519
HRN = high risk newborns
WBN -= well-baby nurseries
ICU = intensive care unit
SSI = surgical site infections
BSI – bloodstream infections
UTI = urinary infections
Klevens, et al. Pub Health Rep 2007;122:160-6
PNEU = pneumonia
7
UTI
36%
424,060
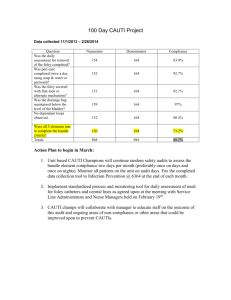
Action Plan to Prevent HAIs, June 2009
http://www.hhs.gov/ophs/initiatives/hai/draft-hai-plan-01062009.pdf
Tier 1: See Targets/Metrics
Tier 2: Ambulatory Surgery Clinics, Dialysis Centers,
Influenza vaccine for Healthcare Personnel
American Recovery and
Reinvestment Act (ARRA), 2009.
Public Law 111-5
8
Health & Human Services HAI Prevention Plan
5 yr. Targets; Progress Report, 09/23-24/10
TOPIC
METRIC & TARGET
Progress Report
Central line-assoc. bloodstream
infection (CLABSI)
CLABSI Std Infection Ratio (SIR);
18% drop in 2009 – on target!
CLABSI Insert. Bundle
Proportion of insertions using
bundle; 100% adherence
Sample of Hospitals = 92% - on
target
C. difficile Infection (CDI)
Rate/1000 discharges; 30%
reduction
8.9 in 2009; 9.4 in 2010 – not
likely to meet target
Catheter-assoc. UTI (CAUTI)
CAUTI rate ; 25% reduction
Estimate in ’08 = 5% reduction
but new def. in ’09 - unsure
MRSA
Rate invasive MRSA/100k pop.;
50% reduction
22.72 in 2009 = 13.4% drop
compared to ’07-’08 – on target
SSI
SIR; 25% reduction
5% fewer SSIs in 2009 – on
target
SSI
Proportion SCIP measures; 95%
adherence
> 92% in 2009 – on target
50% reduction
9
National Patient Safety Goals (NPSG),
Hospital, 2010
• NPSG.07.01.01: Hand Hygiene
• NPSG.07.03.01: Prevent HAIs caused by multidrugresistant organisms (MDROs)
• NPSG.07.04.01: CLABSI prevention
• NPSG.07.05.01: SSI prevention
===============================
New Goals for 2011; CAUTI & VAP – in press
10
• Proposed NPSG.07.07.01: Implement evidence-based
practices to prevent indwelling catheter-associated urinary
tract infections (CAUTI)
– Insertion:
• Limiting use and duration to situations necessary for patient care
• Use aseptic techniques
– Maintenance:
• Secure
• Maintain closed system
– Measure and monitor catheter-associated urinary tract infection
prevention processes and outcomes
Field Review Comments Were Due: January 27, 2011
Final version and elements are in press
11
UTIs Also Represent Significant Reservoir of
MDROs
12
New Respect for UTIs?
Emerging Reservoir of MDROs*
New Delhi metallo-beta-lactamase (NDM-1):
Transmissible genetic element Enterobacteriaceae [Klebsiella, E. coli, etc.]
Inactivates beta lactam antibiotics [penicillin, cephalosporins, carbapenem
First identified in 2008 in India – now found in US, Canada, Israel, Turkey,
China, Australia, France, Japan, Kenya, Singapore, Taiwan, Sweden, & the UK
Epidemiology of Cases in the U.S.:
3 different patients residing in 3 different states in the U.S.; prior history of
Health care in India
All were causing urinary tract infection
N Engl J Med 2010 December 16, 2010
* Multidrug-resistant organisms
13
CAUTI Prevention
AHRQ Report (2001); APIC (2008); SHEA/IDSA (2008); CDC/HICPAC (2009)
• Appropriate urinary catheter use
– Insert only for appropriate reasons
– Remove when no longer needed (reminders/stop orders)
• Avoid catheter use
– Portable bladder ultrasound
• Consider use of alternatives
– Condom catheters, intermittent catheterization
14
CAUTI Prevention (cont.)
• Use of proper insertion technique
– Aseptic technique in acute care settings
• Proper urinary catheter maintenance
• If the CAUTI rate is not decreasing after implementing
other prevention strategies, consider using
antimicrobial catheters
15
Which method of hand hygiene is best
for personnel caring for urinary
catheters?
Poor
Better
Best
Alcohol-based
Antimicrobial
handrub
soap
Catheter bacterial contamination study: hand hygiene
followed by contact with urinary catheter; findings:
Soap + water failed to prevent transfer to cath.
in 11/12 (92%) instances
Alcohol-based handrub: 2/12 (17%) (p < 0.001)
Plain Soap
Source: Ehrenkranz NJ ICHE 1991;12:654-62
16
Ann Arbor VA Health Services Research &
Development (HSRD) & U of M Patient Safety
Enhancement Program [PSEP]
• Mixed Methods Research Project: Drs. Sarah Krein &
Sanjay Saint – Principal Investigators
– Practice Survey
– Qualitative Interviews
– Site Visits
• Collaboration with MI Keystone Center for Patient
Safety & Quality
• Survey Distributed March 2009:
– Note of thanks to Infection Preventionists who completed survey and have
participated in interviews & ongoing site visits
– Results in press
17
Methods
•National survey of infection preventionists
•Stratified random sample of U.S. hospitals
–Non-federal general medical/surgical hospitals with 50 or
more hospital beds and intensive care unit beds
–Randomly selected 300 with 50-250 beds and 300 with >
250 beds
–Oversample of hospitals in Michigan
•Initial survey in March 2005 and repeated in March 2009
•Response rate of ~ 70% (national) / ~ 80% (MI)
18
Hospital Characteristics
2005
(national)*
2009
(national)*
2009
(MI)
229
(219 - 239)
226
(215 - 237)
238
(187 – 289)
57%
75%
76%
1.3
(1.2 – 1.4)
1.5
(1.4 – 1.7)
1.7
(1.2 – 2.1)
Lead IP certified in infection
control
57%
59%
58%
Participate in a collaborative
effort to reduce HAI
42%
68%
99%
Number of hospital beds
mean (95% CI)
Have hospitalists
Number of full-time equivalent
infection preventionists (IP)
mean (95% CI)
*Weighted estimates
19
Report almost always or always using to
prevent CAUTI
National Sample
20
Efficacy of Enhancing Catheter Awareness;
Meddings J, et al. Clin Infect Dis 2010;51:550-60
Rate of CAUTI
can be reduced
by half with use
of catheter
reminder or
stop order.
Process vs.
Outcome
21
CAUTI Prevention Initiative: A Simple
Approach
• Physician Reminder System Implemented, 473 bed
community, teaching hospital
– Appropriate use of urinary catheters at 3 months (57% vs
73%; p=0.007) and 6 months (57% vs 86%; P <0.001).
– Significant reduction in rate of CA-UTI after 3 months (7.02 vs
2.08; P <0.001) and 6 months (7.02 vs 2.72; p <0.001)
Bruminhent J, et al. Am J Infect Control
2010;38:689-93.
22
Report almost always or
always using to prevent CAUTI
23
System for monitoring
duration and/or discontinuation of urinary catheters
100%
100
90%
80%
70%
%
60%
50%
40%
30%
20%
10%
0
0%
19
14
34
74
28
facility wide
unit specific
none
73
59
39
2005
2005MI
MI
2005
Nation
2005
2009MI
MI
2009
National
24
2009
2009 Nation
National
Managing Expectations: Catheter-Associated
Urinary Tract Infection and the Medicare
Rule Changes [Saint S, et al. Ann Intern Med 2009;877-84]
• Recommendations for Providers:
– Develop or adopt existing protocols that emphasize
appropriate use, care and maintenance of urethral
catheters
– Develop systems that promote removal of
catheters once no longer needed
– Clinician education: use, interpretation, and
response to urinalysis & urine cultures
– Avoid use of urinalysis or culture to detect “present on
admission” (POA)
25
Use of infection prevention practices
2009: Minding the Gap
CLABSI
%
VAP
100
90
80
70
60
50
40
30
20
10
0
26
CAUTI
Nurse-Led Multidisciplinary Rounds on
Reducing Unnecessary Catheter Utilization
Proportion of urinary
catheters indicated =
54.8%
Nurse-led intervention
was associated with
discontinuation
of 45% of those catheters
that did not meet
Indications.
Fakih M, et al. Infect Control
Hosp Epidemiol 2008;29:815-9
27
Focus on Processes of Care
Acknowledgement: Images courtesy of St. Alphonsus
Regional Medical Center, Boise, IA
28
Process vs Outcome Metrics Related to
CAUTI Prevention
• Progressive Care &
Observation Units, 60 beds
• Urinary catheter use
decreased by 42% and the
incidence of CAUTIs
decreased by 57%.
29
At the Bedside: CAUTI Prevention
Collaborative, St. Joseph Mercy Hospital, Ann Arbor
30
CAUTI Prevention
Team Members
• Katy Hoffman, Nurse Manager, 3 East – Chair & Chief
Executive Champion
• Alvira Galbraith, Nurse Manager, Older Adult Unit
• Pilot Units [3E, 9E] Staff: RNs, MDs, Pt Care Assistants
• Pam Ceo, Nurse Practitioner - Urology
• Pam Willoughby, Education Coordinator, 3 East
• Linda Bloom, Manager, SJM-Saline Comm. Hosp, Med-Surg
• Gail Siedlaczak & Russ Olmsted, Infection Prevention &
Control
• Lakshmi Halasyamani, MD – VP, Quality, Patient Safety &
Systems Improvement
31
At the Bedside - Baseline data, SJMH
One Day Point Prevalence Study:
All inpatient units, 4/20/2009
• Total Patients: 340
• Total With Indwelling Urinary Catheters (IUC) = 101
• Prevalence = 29.7%
Keystone Bladder Bundle: Two Pilot Units
• 76.2% of IUC’s had a physician order
• 67.9% met HICPAC indications
32
CAUTI Prevention At the Bedside,
SJMH
1. Ensure the catheter is indicated.
•
•
•
Revision of Hospital Policy
Improve consistency of Provider orders
Education:
•
•
•
•
•
•
CDC indications and non-indications for Indwelling Urinary Catheters
Poster Presentations
Online education module for personnel
Patient/Family Handouts
Collaboration with the Emergency Dept. to decrease
insertion of unnecessary IUC’s
Consider alternatives to IUC’s (condom catheters, scheduled
toileting, etc.)
33
CAUTI Prevention At the Bedside, (cont)
2. Insert and Maintain IUC using proper
technique
•
•
•
•
Adherence with Revised IUC Policy
Utilization of Stat-lock or other securing
devices (Dale elastic leg strap, tape)
Location of tubing and dependent drainage
bag
Improve documentation of Insertion, including
date/time
34
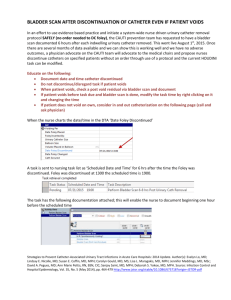
Supporting Improvement through
the Electronic Health Record
Urinary Cath. alert to RN (with task and order)
35
CAUTI Prevention At the Bedside,
SJMH,cont.
3. Remove catheters when no longer
appropriate
•
•
•
Daily screening tool
Nurse driven process for discontinuation
Portable Bladder Ultrasound Scanning
36
Results of Bladder Bundle: Before & After EHR
Implementation, SJMH-AA, 2009
New EHR System
CAUTI Quarterly Data
100
90
80
70
60
50
40
30
20
10
0
April
June
September
Prevalence
December
Percentage of IUC's with Physician Order
Percentage of IUC's Clinically Appropriate
37
Summary CAUTI Data, SJMH
90
80
70
Prevalence
60
%
50
Indications-Meet CDC
criteria
Orders
40
30
20
10
0
09-Nov
10-Feb
38
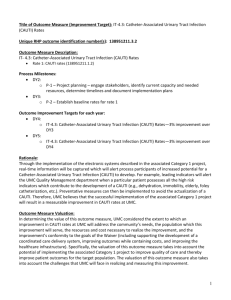
Distribution for Indication for Urinary Catheterization,
SJMH-AA, November 2009, Med-Surg Unit A
10%
5%
Urinary Retention-10%
U.O. Critically Ill-5%
Immobilization-45%
No Orders-40%
40%
45%
39
Distribution for Indication for Urinary Catheterization,
SJMH-AA, February 2010, Med-Surg Unit A
18%
12%
Urinary Retention-55%
U.O. Critically Ill-15%
Immobilization-12%
No Orders-18%
55%
15%
40
Surveillance for CAUTI, NHSN
• Urinary tract infections (UTI) are defined:
– Symptomatic urinary tract infection (SUTI) or
Asymptomatic Bacteremic UTI (ABUTI)
• CAUTIs = catheter-associated (i.e. patient had
an indwelling urinary catheter at the time of
or within 48 hours before onset of the UTI)
– NOTE: There is no minimum period of time that the
catheter must be in place in order for the UTI to be
considered catheter-associated
http://www.cdc.gov/nhsn/pdfs/pscManual/7pscCAUTIcurrent.pdf
41
Surveillance for CAUTI, NHSN
Application
• Not CAUTI:
• CAUTI:
– Day 1: Patient has an
indwelling urinary catheter in
place on an inpatient unit B.
– Day 2: Catheter is
discontinued
– Day 6:
– Day 1: Patient admitted
through the ED where a
urinary catheter is inserted
and admitted to Unit A. Day 3
of hospitalization:
• Catheter remains in place
• Fever (>38°C),
• Urine culture = ≥105
colony-forming units
(CFU)/ml of E. coli
• fever (>38°C), urgency, &
frequency
• Urine culture = ≥105 CFU/ml
Proteus mirabilis
– Patient has a SUTI BUT is not
a CAUTI because the time
since discontinuation of the
catheter is > 48 hours
– Meets NHSN criteria for
symptomatic urinary tract
infection (SUTI) + has
catheter
42
CAUTI Surveillance Flow Chart
43
CAUTI Surveillance Flow Chart
44
ABUTI Flow Chart
45
Calculation of CAUTI Rate
• Numerator: # CAUTIs for May 2011, Unit A
• Denominator: Tot. number of catheter days for Unit
A in May 2011
• RATE: The CAUTI rate per 1000 urinary catheter days
is calculated by dividing the number of CAUTIs by
the number of catheter days and multiplying the result
by 1000
– Example: 1 CAUTI, Unit A, 05/11______
250 urin.cath.days,Unit A, 05/11 X 1,000 = 4.0
46
NHSN Summary Data Report
Edwards JR, et al. Am J Infect Control 2009;37:783-805.
47
Perspectives on Role of the Infection
Preventionist on CAUTI Prevention Teams
• Nurse, and ideally, Physician Champion(s) in the
Clinical Care Area Are Critical Element of Success
– We were fortunate to have engagement of clinical leadership of our
CAUTI Prevention Team
• Infection Preventionist – key stakeholder and subject matter
expertise, but not necessarily Team Leader or Unit-based
Champion.
– [Note: this was the model from Keystone ICU involving prevention of
VAP & CLABSI]
• A member of Infection Prevention & Control Services at SJMH
does collect ongoing, periodic, unit-based data on processes
of care involving IUCs.
• Ongoing monitoring to sustain gains is important; aka keeping
your eye on the ball [Meaningful Use of Surveillance]
48
Core Prevention Strategies:
(All Category IB)
Catheter Use
• Insert catheters only for appropriate indications
• Leave catheters in place only as long as needed
Insertion
Maintenance
• Ensure that only properly
Hand Hygiene
trained persons insert and
maintain catheters
• Insert catheters using
aseptic technique and
sterile equipment (acute
care setting)
Quality Improvement Programs
• Following aseptic
insertion, maintain
a closed drainage
system
• Maintain
unobstructed urine
flow
http://www.cdc.gov/hicpac/cauti/001_cauti.html
49
A Model For
Implementation Science
Saint S, et al ICHE 2010
50
Parting Thoughts
• Prevention of CAUTI is supported by several external
organizations and initiatives
• National surveys continue to identify significant gaps
between CAUTI prevention evidence in the literature
and care of the patient at the bedside
• Use the 4 “Es”: engage, educate, execute, & evaluate
for your CAUTI prevention teams
• The IP is a key member of this team but does not
necessarily have to lead – clinical champions can
provide this leadership
• Use a variety of measures with emphasis on processes
aimed at urinary catheter stewardship
51
Your Feedback is Important
http://www.surveymonkey.com/s/FN9BJKB
52
Questions
• Content – Russ Olmsted, SJMHS
– Olmstedr@trinity-health.org
• Participation– Your State Lead
53