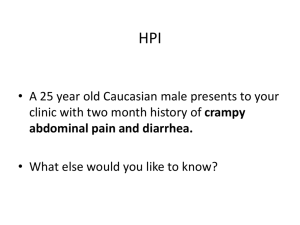
ID 1
advertisement

The Pathology of Intestines I Developmental anomalies Atresia (bowel): complete failure of development of the intestinal lumen (imperforate anus) Stenosis (bowel): narrowing of the intestinal lumen Duplication (small intestine): well-formed saccular-tubular cystic spaces (may or may not communicate with the lumen). Omphalocele (small intestine): a membranous sac; herniation. Malrotation (bowel): malposition of the large intestinal components (caecum in the left upper quadrant). Meckel diverticulum: (small intestine) Common; in ileum; Failure of involution of the omphalomesenteric (vitelline) duct which connects the lumen of the developing gut to the yolk sac ; Persistent blind-ended tubular protrusion (5-6 cm long); Contains all three layers of the normal bowel wall: mucosa, submucosa, and muscularis propria; Asymptomatic Pernicious anemia-like syndromes (bacteria B12 depletion); Acute appendicitis-like syndrome (heterotopic rests of gastric mucosa Peptic ulcerationbleeding). Hirschsprung’s Disease (Congenital Megacolon) Pathogenesis: The enteric neuronal plexus develops from neural crest cells which must migrate into the bowel wall during development mostly in a cephalad-to-caudad direction. Congenital megacolon, or Hirschsprung’s disease, results when the migration of neural crest cells arrests at some point before reaching the anus. Hence a segment remains that lacks both Meissner’s submucosal and Auerbach’s myenteric plexuses. Loss of enteric neuronal coordination leads to (1) functional obstruction (2) colonic dilatation proximal to the affected segment. Occurs in approximately 1 out of 5000 to 8000 live births M/F : 4/1 Hirschsprung’s disease is characterized by the absence of ganglion cells, ganglia, in the muscle wall and submucosa of the affected segment. The rectum is always affected, (most cases involve the rectum and sigmoid only), Proximal to the aganglionic segment, the colon undergoes progressive dilatation and hypertrophy. With time, the colon may become massively distended, sometimes achieving a diameter of 15 to 20 cm (megacolon) The colonic wall becomes markedly thinned and may rupture, usually near the caecum. Mucosal inflammation or shallow stercoral ulcers produced by impacted feces may appear. Enterocolitis. Acquired megacolon (1) Chagas’ disease (in which the trypanosomes directly invade the bowel wall to destroy the enteric plexuses); (2) obstruction of the bowel as by a neoplasm or inflammatory stricture; (3) toxic megacolon complicating ulcerative colitis or Crohn’s disease (4) a functional psychosomatic disorder. Vascular disorders Ischemic Bowel Disease Arterial thrombosis Arterial embolism Venous thrombosis Nonocclusive ischemia Miscellaneous: radiation injury, volvulus, stricture, and internal or external herniation. Angiodysplasia Hemorrhoids Ischemic Bowel Disease Restricted to the small or large intestine or may affect both, Acute occlusion of one of the three major supply trunks of the intestines (celiac and superior and inferior mesenteric arteries) infarction. Lesions within the end-arteries, which penetrate the gut wall, produce small, focal ischemic lesions. The severity of injury ranges from (1) transmural infarction of the gut, involving all visceral layers (acute occlusion of a major artery); (2) mural infarction of the mucosa and submucosa; (3) mucosal infarction (erosions), if the lesion extends no deeper than the muscularis mucosa. Arterial embolism: cardiac vegetations, angiographic procedures, aortic thromboembolism. Arterial thrombosis: severe atherosclerosis (a.mesenterica), systemic vasculitis (polyarteritis nodosa), dissecting aneurysm, angiographic procedures, aortic reconstructive surgery, surgical accidents, hypercoagulable states, oral contraceptives. Venous thrombosis: hypercoagulable states, oral contraceptives, antithrombin III deficiency, intraperitoneal sepsis, the postoperative state, invasive neoplasms (particularly hepatocellular carcinoma), cirrhosis, abdominal trauma. Nonocclusive ischemia: Miscellaneous: -Radiation -Volvulus -Stricture -herniation cardiac failure, shock, dehydration, vasoconstrictive drugs (digitalis, vasopressin, cocaine, heroin). Morphology Transmural Infarction: Sudden and total occlusion of mesenteric arterial blood intestinal infarction. Arterial or venous occlusionhemorrhagic infarct, ischemic injury mucosal necrosis 18-24 h fibrinous exudate over the serosa Margins of the infarct: in arterial occlusions : distinct (demarcation) in venous occlusions : less distinct Microscopy: edema, interstitial hemorrhage, necrosis (24 h)gangreneperforationperitonitis !!! Mural & Mucosal Infarction: In any level of the gut from the stomach to anus lesions may be multifocal-scattered or continuous-widely distributed (depends on the level of the arterial narrowing), does not affect the entire thickness (may not be visible from the serosal surface), on opening the bowel, there is hemorrhagic, edematous thickening of the mucosa. Superficial ulcerations with edema, hemorrhage, fibrinous inflammation (psedomembrane due to superinfection). Chronic Ischemia: Chronic vascular insufficiency mucosal inflammation and ulceration Submucosal chronic inflammation and fibrosis stricture. Segmental and patchy. Angiodysplasia Tortuous dilatations of submucosal and mucosal blood vessels most often in the cecum or right colon after the sixth decade of life intestinal bleeding: chronic and intermittent (anemia) acute and massive. Hemorrhoids Variceal dilatations of the anal and perianal venous plexuses Persitently elevated venous pressure within the hemorrhoidal plexus Predispositions: chronic constipation, pregnancy. Thin-walled, dilated vessels Complications: Bleeding, prolapsing. Diarrheal diseases Diarrhea is an increase in stool: Mass Frequency Fludity Disentery is a kind of diarrhea with: Low-volume Pain Hemorrhage Diarrhea 1. Secretory diarrhea 2. Osmotic diarrhea 3. Exudative diarrhea 4. Malabsorption 5. Deranged motility 1. Secretory diarrhea Intestinal fluid secretion (catarrh) Serous Causes: Infection (bacteria, virus) Neoplastic (secretion of peptides and serotonin) Excessice laxative use 2. Osmotic diarrhea Excessive osmotic forces Causes: Lactulose therapy (hepatic encephalopathy, constipation) Gut lavage Antacids (magnesium salts) 3. Exudative diarrhea Purulent/bloody stool Causes: Infections escherichia, campylobacter, shigella, salmonella, Entamoeba histolytica, Idiopathic inflammatory bowel disease 4. Malabsorption Voluminous, bulky stool Causes: Defective intraluminal digestion Defective mucosal cell absorption Reduced small intestinal surface area Lymphatic obstruction Infection (Giardia) 5. Deranged motility Decreased intestinal retention time Surgical reduction of gut length Neural dysfunction (irritable bowel syndrome) Hyperthyroidism Decreased motility Surgery Bacterial overgrowth in the small intestine Infectious enterocolitis Intestinal diseases of microbial origin Diarrhea and sometimes ulceroinflammatory changes Most common offenders rotavirus Norwalk virus Enterotoxigenic Escherichia coli Offenders vary with the age, nutrition, immune status of the host, environment (living conditions, public health measures), Special predispositions: hospitalization, wartime dislocation, foreign travel. Viral Gastroenterocolitis The small intestinal mucosa usually exhibits shortened villi infiltration of the lamina propria by lymphocytes vacuolization and loss of the microvillus brush border in surface epithelial cells crypts appear hypertrophied viral particles within surface epithelial cells by electron microscopy and in stool. Bacterial Gastroenterocolitis Numerous bacteria and several pathogenic mechanisms: Ingestion of preformed toxin, present in contaminated food (major offenders are Staphylococcus aureus, Vibrios, and Clostridium perfringens) Infection by toxigenic organisms (which proliferate within the gut lumen and elaborate an enterotoxin) Infection by enteroinvasive organisms (which proliferate, invade, and destroy mucosal epithelial cells) Most bacterial infections exhibit a general nonspecific pattern: damage of the surface epithelium decreased epithelial cell maturation an increased mitotic rate (“regenerative change”) hyperemia and edema of the lamina propria variable neutrophilic infiltration into the lamina propria and epithelial layer. Salmonella (multiple species, including S. typhimurium and S. paratyphi): primarily ileum and colon blunted villi, vascular congestion, Peyer’s patch involvement with swelling, congestion, ulceration (linear ulcers) Typhoid fever : may result in chronic infection of biliary tree, joints, bones, meninges. Shigella primarily distal colon acute mucosal inflammation and erosion purulent exudate Campylobacter small intestine, appendix, colon villus blunting multiple superficial ulcers mucosal inflammation purulent exudate Yersinia enterocolitica and Y. pseudotuberculosis: V. cholerae: ileum, appendix, and colon mucosal hemorrhage and ulceration bowel wall thickening Peyer’s patch and mesenteric lymph node hypertrophy with necrotizing granulomas systemic spread (with peritonitis, pharyngitis, pericarditis 3-Ps) essentially intact small intestinal mucosa, with mucus-depleted crypts C. perfringens: similar to V. cholerae but with some epithelial damage; some strains produce a severe necrotizing enterocolitis with perforation. Necrotizing Enterocolitis Neonates (premature or of low birth weight) acute, necrotizing inflammation. A combination of ischemic injury, colonization by pathogenic organisms, excess protein substrate in the intestinal lumen, functional immaturity of the neonatal gut. The disease may present as a mild gastrointestinal disturbance or as a fulminant illness with intestinal gangrene, perforation, sepsis, shock. Terminal ileum and ascending colon, although in severe cases, the entire small and large bowel may be involved. In early phases, the mucosa exhibits As the disease progresses, the full thickness of the bowel wall becomes edema, hemorrhage, necrosis hemorrhagic, inflamed, gangrenous frank intraluminal hemorrhage mural gas formation Reparative changes epithelial regeneration granulation tissue formation fibrosis. Antibiotic-Associated Colitis (Pseudomembranous Colitis) C. difficile (a normal gut commensal) acute colitis plaque-like adhesion of fibrinopurulent-necrotic debris and mucus to damaged colonic mucosa following a course of broad-spectrum antibiotic therapy also may occur following any severe mucosal injury, ischemic colitis, volvulus, necrotizing infections (staphylococci, shigella, candida, necrotizing enterocolitis) Malabsorption Syndromes Malabsorption is characterized by suboptimal absorption of fats, fat-soluble and other vitamins, proteins, carbohydrates, electrolytes and minerals, and water. The consequences of malabsorption affect many organ systems. Etiology Mal-digestion: Exocrine pancreatic disease Lack of bile salts Disaccharidase (lactase, etc.) deficiency Problems with the small bowel mucosa: Sprue Crohn's disease Whipple's disease Acute infections Parasites (Giardia) Allergic gastroenteritis Amyloidosis Lymphomas Radiation sickness / B12 / folate deficiency Super-fast transit time: Laxatives Cholera Vasoactive intestinal polypeptide-producing tumors Mechanical problems: Blocked lymphatics (cancer, TB) After re-routing surgery (gastrectomy, bypass) Clinicopathology Alimentary tract: Skin: Hematopoietic system: diarrhea abdominal pain weight loss vitamin deficiencies anemia (iron, pyridoxine, folate, or vitamin B12 deficiency) bleeding (vitamin K deficiency) Nervous system: peripheral neuropathy Musculoskeletal system: purpura and petechiae edema dermatitis hyperkeratosis osteoporosis tetany Endocrine system: amenorrhea impotence infertility hyperparathyroidism Celiac sprue Small intestine idiosyncratic reaction to gliadin, a protein in the gluten of wheat, rye, and barley an antibody against the transglutaminase activated cytotoxic killer-T cells invade the epithelium Microscopy: villi disappear crypts deepen Whipple's disease Small intestine & systemic lipid pools in the mucosa Tropheryma whippelii (~actinomyces) bacilli-laden macrophages in: gut mucosa lymph nodes, joints, endocardium brain. IDIOPATHIC INFLAMMATORY BOWEL DISEASES Crohn’s Disease Idiopathic Western developed populations limited to the terminal ileum (terminal ileitis) segmental lesions with intervening unaffected (“skip”) areas (regional enteritis) any level of the alimentary tract with systemic manifestations Crohn’s disease: Morphology Early disease: focal mucosal ulcers Progressive disease: mucosal ulcers coalescelong, serpentine “linear ulcers” tend to be oriented along the axis of the bowel mucosa acquires a coarsely textured, “cobblestone” appearance narrow fissures penetrating deeply through the bowel wall perforation or localized abscesses Hallmark: sharp demarcation of diseased bowel segments from adjacent uninvolved bowel. Crohn’s disease: Morphology Serosa: granular and dull gray Mesentery: thickened, edematous, and sometimes fibrotic Intestinal wall: rubbery and thick (edema, inflammation, fibrosis, hypertrophy of the muscularis) Lumen: narrowed (x-ray film of small intestine shows “string sign” ) Segmental disease: sharp demarcation of diseased bowel segments from adjacent uninvolved bowel. Crohn’s disease: Morphology Microscopic Characteristics: Transmural involvement of the bowel by Fissuring and formation of fistulas Crypt destruction inflammatory process mucosal damage noncaseating granulomas(50%) lymphoid aggregates fibrosisstrictures progressive atrophy Paneth cell metaplasia Ulcerative colitis An ulceroinflammatory disease limited to the colon affecting only the mucosa and submucosa extends in a continuous fashion proximally from the rectum (in contrast to Crohn’s disease) granulomas are absent Systemic disorder (similar to Crohn’s disease) migratory polyarthritis, sacroiliitis, ankylosing spondylitis, uveitis, hepatic involvement (pericholangitis and primary sclerosing cholangitis), skin lesions. Involves the rectum and extends proximally in a retrograde fashion to involve the entire colon (“pancolitis”) in the more severe cases. It is a disease of continuity “skip” lesions such as occur in CD are not found In 10% of patients with severe pancolitis, the distal ileum may develop mild mucosal inflammation (“backwash ileitis”). The appendix may be involved with both CD and UC. The mucosa exhibits slight reddening granularity friability easy bleeding Fully developed severe, active inflammation: extensive and broadbased ulceration of the mucosa in the distal colon or throughout its length Isolated islands of regenerating mucosa bulge upward to create “pseudopolyps.” Often the undermined edges of adjacent ulcers interconnect to create tunnels covered by tenuous mucosal bridges. The ulcers are frequently aligned along the axis of the colon (as with CD) In contrast to Crohn’s disease: rarely do the linear serpentine ulcers mural thickening does not occur Progressive mucosal atrophy in chronic cases Microscopy: diffuse mononuclear inflammatory infiltrate in the lamina propria, admixed with neutrophils occasional eosinophils and mast cells. Diffuse mononuclear cell infitration Pseudopolyps (carpet-like mucosa) pseudopolyp ulcer Crypt abscess Crypt abscess Long-term complication of UC : cancer. Particular attention to: epithelial changes signifying dysplasia and the progression to frank carcinoma Underlying inflammatory disease may mask the symptoms and signs of carcinoma The risk of cancer is highest in patients with pancolitis of 10 or more years’ duration, in whom it exceeds by 20-fold to 30-fold that in a control population. Malabsorption Syndromes Celiac sprue Gluten (gladin) Whipple's disease Tropherhyma whipplii Small intestine villi disappear crypts deepen Small intestine bacilli-laden macrophages (lymph nodes, joints, endocardium and/or brain) Bacterial Overgrowth Syndrome Aerobic and anaerobic organisms Proximal small Disaccharidase deficiency Less intestinal lactase Small intestine Abetalipoproteinemia Inability to All enterocytes loaded with dietary fat Terminal ileum noncaseating granulomas Crohn’s Disease Ulcerative Colitis bowel immunedeficiencies synthesize Idiopathic luminal stasis, hypochlorhydria, osmotic diarrhea and ulcers with perforation Idiopathic Colon Severe active inflammation, ulcers & pseudopolyps Location Bowel Terminal ileum Colon Anal troubles Oral lesions Skip lesions Layers Ulcers Pseudopolyps Fibrosis Fistulas Granulomas Bleeding Carcinoma risk Crohn's disease Variable Small Favorite site Right more than left Common Maybe + All three Linear fissures +++ +++ + + Subtle + Ulcerative colitis Rectum and upwards Large "Backwash" Left more than right No; continuous Mucosa only Broad / irregular ++ Heavy-duty +++ Colonic Diverticulosis A diverticulum is a blind pouch leading off the alimentary tract, lined by mucosa that communicates with the lumen of the gut Acquired diverticula may occur in the esophagus, stomach, and duodenum; duodenal diverticula occur in more than 1% of adults Congenital diverticula (Meckel’s diverticulum) have all three layers of the bowel wall; all other diverticula are acquired and either lack or have an attenuated muscularis propria. Histology: a thin wall composed of a flattened or atrophic mucosa, compressed submucosa, attenuated or totally descending colon or absent muscularis entire colon, however, propria may be affected hypertrophy of the Pathogenesis circular layer of the (1) focal weakness in the muscularis propria in colonic wall the affected bowel (2) increased intraluminal segment is usually pressure. seen. Most colonic diverticula are small flask-like or spherical outpouchings, usually 0.5 to 1 cm in diameter and located in the sigmoid colon Complications Obstruction Perforation Marked fibrotic thickening due to the inflammation Narrowing (resembles colonic cancer) Diverticular infection pericolic abscesses sinus tracts pelvic or generalized peritonitis. Bowel Obstruction Mechanical obstruction Adhesions (post-op, Crohn's) Hernias Volvulus Intussusception Tumors Inflammatory strictures Obstructive material (gallstone, fecalith, foreign body) Congenital Atresia of the anus / imperforate anus Congenital atresia / strictures Meconium ileus (cystic fibrosis) Pseudo-obstruction Paralytic ileus Vascular bowel infarction Myopathies & neuropathies (Hirschsprung’s disease) Bowel Obstruction : Hernias A weakness or defect in the wall of the peritoneal cavity may permit protrusion of a pouch-like, serosa-lined sac of peritoneum, called a hernial sac. The usual sites: anteriorly at the inguinal and femoral canals, umbilicus, surgical scars. Intruders : small bowel loops, omentum, large bowel. Pathology: impair venous drainage of the trapped viscus stasis and edema compromise of arterial supply and venous drainage (strangulation) infarction of the trapped segment. Bowel Obstruction : Adhesions Peritonitis: surgical procedures, infection, endometriosis. As the peritonitis heals: adhesions (between bowel segments or the abdominal wall and operative site) fibrous bridges closed loops trapped intestine (internal herniation). The sequence of events following herniation: obstruction strangulation. Bowel Obstruction : Intussusception Intussusception occurs when one segment of the small intestine, constricted by a wave of peristalsis, suddenly becomes telescoped into the immediately distal segment of bowel. Once trapped, the invaginated segment is propelled by peristalsis farther into the distal segment, pulling its mesentery along behind it. Clinical: intraluminal mass or tumor as the point of traction. Complications: intestinal obstruction infarction. Bowel Obstruction : Volvulus Complete twisting of a loop of bowel about its mesenteric base of attachment produces intestinal obstruction and infarction. Sigmoid, cecum, small bowel (all or portions), stomach, transverse colon (rarely).