Williams, T., Worley, C., Canner, N., & Lawler, E. (2012). Sustained
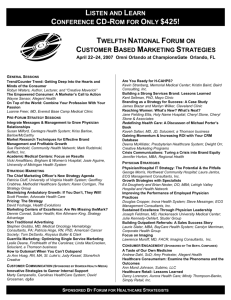
advertisement

CHAPTER 2 ORGANIZING FOR AGILE AND SUSTAINABLE HEALTHCARE: THE ALEGENT HEALTH CASE Christopher G. Worley, Ph.D. Senior Research Scientist Center for Effective Organizations Marshall School of Business University of Southern California Los Angeles, CA 90089 cworley@marshall.usc.edu 1-213-740-9814 Acknowledgements: Sincere thanks and appreciation are extended to the leadership at Alegent Health, and in particular to Kenneth Lawonn, senior vice president technology and strategy, for their support in writing this chapter. Appreciation is also given to my colleagues at the Center for Effective Organizations and the editors of this volume for their feedback and support. 1 ABSTRACT Purpose This chapter argues that the concept of agility is an effective robust framework for designing sustainable healthcare systems. Design/Methodology/Approach This case study of Alegent Health was based on seven years of data collection. It includes observations of meetings, large-group interventions, and other activities; site visits to different hospitals in the system to observe changes in practice; interviews with Alegent Health executives, primary care physicians, hospital presidents, specialist physicians and physician groups, and health systems staff and nurses; and a variety of archival data including meeting minutes, video tapes, conference proceedings, and website material. Findings The Alegent Health system has evolved over time according to the principles of agility. It built a series of new capabilities that contribute to improved clinical outcomes, sustained financial results, and more socially and ecologically responsible results. Designing healthcare systems based on agility is a more effective and sustainable approach than relying on legislative or other criteria. Originality/Value 2 The discussion of sustainability in healthcare has focused primarily on specific projects or how to respond to specific technological, regulatory, or clinical changes. Alegent Health’s experience provides important lessons, opportunities, and challenges that can help advance our understanding of effective healthcare and use organizational agility to create more sustainable healthcare systems. This chapter provides healthcare system administrators an alternative design option. Keywords: agility, sustainable healthcare, organization design Category: Research paper 3 INTRODUCTION The Affordable Care Act was an important milestone in U.S. healthcare reform, and its implications and implementation challenges occupy many of the column inches in newspapers, magazines, and journals. While almost everyone agrees healthcare is broken, this legislation and the public debate surrounding it reflects deep divisions over how the system should operate. Increasing costs, decreasing quality, restricted access, feelings of entitlement to care, the impending bankruptcy of the Medicare/Medicaid budget, and a variety of entrenched stakeholder positions contribute to a contentious national conversation. To date, much of the legislative debate has focused on healthcare financing (c.f., Meyer, 2011; Clark, Savitz, and Pingree, 2010). The perspective taken here is that such a focus, while urgent, often misses two important issues that, if not addressed, could negate or neutralize the benefits of reform and have broader long-term consequences. First, much of the focus of healthcare reform and affordable care has been on “accountable care organizations” (ACOs) (Meyer, 2011; Devers and Berenson, 2009). ACOs are the instrument through which Medicare reimbursement will occur and how providers are being encouraged to collaborate to achieve lower costs and higher quality. The focus has NOT been on how such organizations are to be designed and there is a dearth of research, case studies, and other efforts to describe the organization designs that will be necessary – even essential – to meeting the objectives of healthcare reform. Second, with the focus on the financial side of reform, environmental and social responsibility issues are receiving less attention. The healthcare industry, in the largest sense of the term, is responsible for an enormous amount of social and ecological consequences, both good and ill. An effective healthcare industry promises important improvements in the quality of 4 life; but an ineffective industry destroys lives, families, and communities and dumps or leaves excessive amounts of toxins in the environment. By not attending to the design of the organizations that will deliver care and their ability to support or generate positive social and ecological consequences, we will have missed an important opportunity to affect change. The purpose of this chapter is to describe how the design concepts of agility, adaptability, and sustainability can be used as appropriate “design criteria” (Mohrman and Cummings, 1989) for healthcare systems. Although designing for agility and sustainability are addressed within a U.S. hospital system, the importance of the issues extends well beyond those borders. Sustaining economic, clinical, social, and ecological outcomes requires the ability to adapt no matter what the regional, regulatory, or cultural context. Healthcare systems everywhere can benefit from the adaptation of agile principles. We use the Alegent Health case, an integrated delivery system (IDS) and provider-hospital-organization (PHO) in Omaha, Nebraska, to demonstrate how these principles might be implemented. Alegent Health’s experience provides important lessons, opportunities, and challenges that can help advance our understanding of effective healthcare and create more sustainable healthcare systems. HEALTHCARE REFORM, ORGANIZATION DESIGN, AND SUSTAINABILITY This section provides a brief review of the context of healthcare reform in the U.S. It then describes frameworks of organization design and their implications on agility, collaboration, integration, and sustainability. These elements and frameworks are used to inform our discussion of Alegent Health’s evolution. The Context of Healthcare Reform in the United States 5 The Patient Protection and Affordable Care Act (ACA) was passed by Congress in 2009 in response to alarming increases in healthcare costs, the lack of insurance coverage and access, and declining clinical care quality. It provided for the phased introduction of a comprehensive and mandated system of health insurance and the creation of accountable systems of care. A key feature of the ACA is the creation of “accountable care organizations” (ACOs). They are defined as “groups of doctors, hospitals, and other healthcare providers, who come together voluntarily to give coordinated high quality care to their Medicare patients” (CMS website, 2012). As defined, ACOs are very similar to physician-health organizations (PHOs), health-maintenance organizations (HMOs), and integrated delivery systems (IDSs), organization forms that emerged during Clinton-era healthcare reform efforts (Bader, 2009; American Hospital Association, 2010; Shortell and McCurdy, 2009; Gillies, Shortell, Anderson, Mitchell, and Morgan, 1993).1 1 In as much as ACOs closely resemble definitions of PHOs, IDSs, HMOs and other models, and while there has been a small amount of research on ACOs per se (Deloitte Healthcare Solutions, 2010; Meyer, 2011; Crosson, 2011; Higgins, Steward, Dawson, and Bocchino, 2011), we do have some understandings of the difficulties of creating effective care through collaboration. The evidence is largely in favor of these forms of organizations (Shortell and McCurdy, 2010). For example, the larger and more integrated the system, the more likely the system is to use standardized care management processes (e.g., Casalino, Gillies, Shortell, Schmittdiel, Bodenheimer, Robinson, Rundall, Oswald, Schauffler, and Wang, 2003; ), implement electronic medical records and more sophisticated IT systems (e.g., Blumenthal, 2009), possess effective quality programs (e.g., Mehrotra, Epstein, Rosenthal, 2006), lower costs (e.g., Medicare Payment Advisory Commission. 2007; Sterns, 2007), and improve clinical outcomes (e.g., Clark, Savitz, and Pingree, 2010). In addition, physicians were more likely to engage in cooperative clinical integration behaviors when their perception of the healthcare system’s image and reputation was high (Dukerich, Golden, and Shortell, 2002) or when the system had a strong patient-centered philosophy (Rittenhouse, Shortell, Gillies, Casalino, Robinson, McCurdy, and Siddique, 2010). Despite these results, healthcare systems struggle to change and tying reimbursements to performance may help. However, an analysis by Devers and Berenson (2009) suggest that ACOs are unlikely to be “game changers” because the organization challenges may be too large to produce short term results. “Even providers with the greater experience with the kinds of payment methods and programs discussed find that it takes time and capacity building in key areas, such as cultural change, managerial and physician leadership, teamwork, health information technology, and management process redesign and improvement” (Devers and Berenson, p. 9). 6 However, this most recent definition stands in contrast to earlier definitions. For example, a January, 2010 definition on the Center for Medicare and Medicaid Services website described ACOs as “an organization of healthcare providers that agrees to be accountable for the quality, cost, and overall care of Medicare beneficiaries who are enrolled in the traditional fee-for-service program who are assigned to it.” This latter definition was based on the original legislation. An ACO began – and I argue that this original definition continues to dominate much of the thinking about and description of ACOs – as a financial instrument. It was conceived of as reimbursement and delivery model to link payments to performance metrics, including cost and quality, for an assigned population of patients. More important than the substantive shift in definition is the likelihood that healthcare reform regulation and requirements in the U.S. will continue to shift. Healthcare providers, whether they are hospitals, physician groups, pharmaceuticals, health insurance companies, or other stakeholders, who look to regulations for operating and design criteria are likely to become frustrated. Healthcare policy, subject to the whims of politics and public opinion, is unlikely to be an effective guide to designing sustainable healthcare systems. It is one thing to set up an incentive system to get individuals, groups, and organizations to behave in certain ways, and it is quite another to design the processes, workflow, decision making, and coordination necessary to produce the behavior in an ongoing way. Organization Design for Agility, Collaboration, Integration, and Sustainability An organization’s design is the configuration of elements that foster (or hinder) the achievement of valued business, customer (patient), and employee outcomes (Nadler and Tushman, 1997; Lawrence and Lorsch, 1967; Galbraith, 1994). According to these perspectives, organization 7 design is more than just structure. It involves the conscious alignment of strategy, structure, systems, and human resource processes. Galbraith (1994) suggests that organization design begins with a clearly articulated strategy that specifies both the direction and goals of the organization but also the means to achieve those objectives. Then, specific features are designed to support the strategy and fit with each other. Among the features that have to be addressed are the work processes that create value for customers and other stakeholders; the core structural units and dynamic lateral structures and processes that focus attention and resources on effective work process execution; the management processes that establish strategies and align goals, define decision making processes and accountabilities, create communication channels, and support organization learning and change; and the reward systems and people processes that align individual and group inducements and contributions and describe the skills, knowledge and values of the workforce. Many of these organization design models have been adapted to specific applications, including high involvement (Lawler, 1986) and customer-centric organizations (Galbraith, 2005). More recently, these models have been used to support more flexible, adaptable, and agile organizations (Sull, 2008; Verlboda, 1998; Haeckel, 1999) and healthcare systems (Goldman and Graham, 1999). Lawler and Worley (2006, 2011) have modified and extended Galbraith’s model to support agility and sustainable effectiveness (Table 1). ---------------------------Table 1 about here ---------------------------- 8 Board Composition and Purpose Most for-profit boards in the United States and Europe are designed and staffed to serve one stakeholder group – investors or owners – and favors an economic performance focus in companies (Conger, 2009; Lorsch and MacIver, 1989). Boards of not-for-profit or nongovernmental organizations (NGOs) are not immune to this financial bias. A sustainable healthcare system design requires an independent chair and members who represent all of the organization’s most important stakeholders, including representatives of the community, medical profession, and the environment. Membership diversity enables a balanced focus on financial, clinical, social, and ecological outcomes. In support of that diverse focus, boards need to routinely receive financial, operational, and clinical information; employee engagement results; and community and environmental impact data to engage and drive more diversified and informed thinking about the organization’s impact on multiple stakeholders. Long and Short-term Strategy Agile and sustainable organizations must have clear, shared, and aligned long-term and shortterm strategies. A sustainably-oriented and change-friendly identity defines the organization’s long-term strategy (Mirvis, Googins, and Kinnicutt, 2010). It possesses an internal culture and set of values that support financial, clinical, social, and environmental behaviors, and it has a brand/image/reputation for pursuing and creating financial, clinical, social, and environmental outcomes. Identities in sustainable organization designs embrace these different types of value creation as a central part of who the organization is and what it stands for. Sustainability initiatives and CSR programs are not “in addition to,” but rather central to decisions that integrate and/or balance profits, social outcomes, and environmental impacts. This can only 9 happen when an organization has a clear identity that stresses all types of value. A specific example can help to show how these concepts are manifest in a healthcare organization. DaVita is a Fortune 500 kidney care services firm and their “we’re a ‘village’ first and a company second” identity reflects such an integrated view (Lawler and Worley, 2011). Internally, there is a clear and widely shared understanding that taking care of patients and each other—maintaining the village—will lead to revenue and profit. Externally, financial analysts know that the quarterly earnings call begins with a review of clinical outcomes first, financial results second. DaVita extends the village metaphor to its community relationships and the natural environment. There are a variety of internal employee support programs, a strong healthcare reform agenda, several external philanthropy efforts that focus on social accountability, and a clear understanding of its environmental responsibilities. DaVita managers and employees actively work to reduce or eliminate the toxic wastes from its dialysis treatment processes. To do otherwise would poison the village water well (figuratively) and fail to create the conditions for long-term survival. In addition, sustainable organization designs are able to leverage their identities by thinking in terms of a short term strategic intent that changes from time-to-time as the demands of the environment change (Worley, Cummings and Mobley, 2000). A strategic intent describes how the organization will achieve economic, clinical, social, and environmental objectives in the current period, and these intents can be described in terms of breadth (e.g., the range of clinical specialties the system pursues, its geographic reach, or patient populations served), aggressiveness (e.g., how hard the organization pursues its goals and strategies, including the investments it makes to achieve them), and differentiation (e.g., the bases on which the healthcare system competes against alternative choices). 10 Importantly, sustainable organizations may never be the best financial performers. An overly aggressive financial performance orientation can involve cost-cutting and other commitments that result in high, but short-term performance levels. This short-sighted focus on “today” prevents it from developing the adaptive capability needed to respond to tomorrow’s changes (Williams, Worley, Canner, and Lawler, 2012; Staw, 1976). Sustainable organizations have this capability, and they recognize that the cost is a lower return on immediate financial performance in exchange for more stable, long-term growth. Each of these elements, breadth, aggressiveness, and differentiation, can be changed relatively quickly to result in a different strategic intent. As a new intent emerges, each element has implications for organization design. For example, the broader the strategy, the more complex the organization must be to address different specialties, geographies, or patient populations. Changes in aggressiveness and differentiators imply shifts in resource commitments and management attention. Flexible Structure, Lateral Coordination, and Ambidextrous Work System Organization design research has highlighted the importance of alignment among design features in producing organization effectiveness (Cummings and Worley, 2009; Beer, 2009; Lawrence and Lorsch, 1967; Rumelt, 1974). To support agile and sustainable strategies, these designs must have flexible structures, effective lateral mechanisms, and ambidextrous work systems. Flexible structures have a “maximum surface area” that puts many organization members in contact with the environment. This often translates into relatively flat structures with an external focus. An external focus increases the structural flexibility by allowing members, first hand, to experience change in the environment and make meaningful inputs to strategy and 11 operations. The sustainability-oriented and change-friendly identity and performance management systems (described below) support this focus. In addition, as business, social, and other environments have become more turbulent and uncertain, the generally accepted “truth” that there is no perfect structural form has focused attention on the importance of intentionally designing and managing lateral coordination in organizations. When it comes to internal clinical integration, the following taxonomy of lateral coordinating mechanisms can be usefully applied (Galbraith, 1993) (Figure 1): ----------------------Figure 1 about here ----------------------The figure suggests that as an organization uses higher levels of integration, the potential for integration and coordination goes up, but so too do the direct costs of coordination. According to this taxonomy, most organizations require the bottom three forms of coordination. At the lowest level, organizations coordinate their activities, both vertically and horizontally, through plans, budgets, goals, and other traditional processes. Additional coordination can be achieved at a relatively small price by building informal mechanisms, such as creating opportunities for individuals in the organization to work with each other (co-location, job rotation) or through interdepartmental events, such as all-hands meetings or after-hours social gatherings. The third method of integration involves formalizing, enabling, and facilitating communication through electronic coordination. Internal networks, such an electronic medical record or IT-enabled social networks, allow people to communicate about any subject, anytime, 12 and any place. These basic, infrastructural elements of coordination provide organizations with the core routines necessary to integrate functions, clinical programs, and sites of service. Additional and higher levels of integration require the deliberate design of new structures. When the organization identifies the need to coordinate among two or more units, specific lateral integrating roles can be created. This might happen for example, when a hospital system appoints a case manager or patient advocate role to ensure that all parts of the system are working together to address an issue. Some issues are more complex than one person can handle and a high level of coordination can be achieved by creating overlay teams. These permanent or temporary teams are cross-functional or multi-stakeholder in composition. They can be organized to deliver services, such as a cardiology team that could include surgeons, clinical staff, radiology technicians, and home-health specialists, or created to support hospital governance in the form of councils, steering committees, and boards. These governance committees typically address issues that must be coordinated across the system. Physician councils, for example, can be created to establish standardized procedures for certain illnesses. Management positions (project managers) are added when an overlay team needs a formal, dedicated leadership role. The last two integrating mechanisms, matrix structure and line organization, represent decisions to change the core structure or surface area of the organization. If prior methods of lateral coordination (around a particular structural logic, such as function or product or geography) are insufficient, the organization can choose to deliberately coordinate two dimensions at the same time (matrix) or structurally separate a business, function, or service as its own unit. A hospital system that grows through acquisition may find that the outpatient clinics 13 in each acquired hospital are too disparate and uncoordinated resulting in uneven utilization. The parent organization could create an outpatient unit to coordinate scheduling. Ambidextrous work systems are also vital to support agility and sustainability. Agile healthcare systems must be able to perform its core work, such as the routine delivery of radiological services, reliably and in service of an existing strategic intent. This is the driver of current performance, including cost savings and clinical quality. But it must also support the creative work that generates new projects, defines new services, or finds better ways of operating. The principles surrounding innovative work design are different and underdeveloped. They are thought to include shared goals, multi-stakeholder teams, transparent information, temporary and iterative work cycles, and social networks (Lawler and Worley, 2011). For example, in addition to the critical work of dialysis, DaVita has an explicit and flexible process, a matrix of people and projects monitored by senior managers, to ensure the right budget, time, objectives, and decision authority are available to support the most important initiatives and projects. This allows the organization to gather and charter resources quickly, and when a project is over, make the resources available for other projects. This is the essence of an ambidextrous organization (Tushman and O’Reilly, 1996). Talent and Performance Management Sustainable organizations view talent and performance management differently than traditional organizations: They have more leaders and different kinds of leaders. Not more individuals in management jobs, but more leaders. Individuals throughout the organization must have the willingness and skills to take leadership roles when appropriate. 14 When moments arise where the right thing to do is uncertain or when something needs to be challenged, agile organizations need individuals to come forward and provide leadership. Leaders need to be effective in resolving issues, making tradeoffs, and getting the right things done to optimize a combination of economic, social, and environmental outcomes. This will only happen if the organization develops a leadership capacity that reflects an identity of shared responsibility, shared leadership, and sustainable effectiveness. It requires a culture that says leadership doesn’t rest with jobs and isn’t restricted to executives. Leadership must be something that anyone in an organization who has a sense of what is right, what a patient requires, or what is necessary to meet environmental and social demands is not only welcomed, but encouraged to exercise (Lawler & Worley, 2011). To support that shared leadership philosophy, sustainable organizations know about and develop the skills and competencies needed to support economic, social, and environmental outcomes. In addition to paying for those skills, reward systems recognize achievement of sustainable profit levels, corporate social responsibility targets, and lower carbon footprints. Ideally, it makes sense to stress group or team performance because of the interdependencies that exist in organizations committed to sustainable effectiveness. Change and Learning Capability Finally, organization designs that drive clinical, financial, and other outcomes must be able to change if they are to sustain those outcomes over time. This requires the flexible features described above plus the ability to change and learn. Since strategic intents can only generate an advantage over a relatively short period of time, organizations need the ability to shift from one intent to another (Fredberg, Norrgren, & Shani, 2011; Worley & Lawler, 2010). 15 Change and learning capabilities, like other capabilities, require a critical mass of knowledge and skill, an architecture to support behavior, and experience (Mohrman and Worley, 2009; Worley and Lawler, 2009; Worley, Feyerherm, and Knudsen, 2010). Many healthcare systems have plenty of knowledge in clinical areas or policy requirements, but are often weaker in their understanding of change and learning. Similarly, effective enterprise-wide change and learning capabilities require a shared language, framework, and tools that support coordination across organization boundaries. Finally, capabilities do not appear fully developed. The organization must practice change and learning to develop the social capital and experience necessary to become proficient at them. The guidelines and definitions provided by healthcare reform are insufficient to guide the design of effective healthcare systems. The principles of organization design based on agility and sustainability however, can help provide a robust set of criteria. Agile organizations can adapt to any change that comes along. Methods and Research Setting Alegent Health is a not-for-profit, faith-based healthcare system and the largest private employer in Nebraska. It was established in January, 1996 through a joint operating agreement between Catholic Health Initiatives and Immanuel Health Systems. Headquartered in Omaha with a service area extending to southwestern Iowa, Alegent Health in 2011 operated ten hospitals and more than 100 sites of service with over 1,200 physicians on its medical staff and approximately 9,000 employees. As with other hospital systems in the U.S. about 200 physicians are employed by the system and provide mostly primary care services. Its founding mission and vision 16 statement, crafted in 2004, relied on its faith-based heritage and challenged the organization to achieve a world-class standard. Alegent Health has engaged in a variety of strategy and organization change efforts since the appointment of a new CEO in 2004 and has made itself available to researchers to help evaluate the effectiveness of different interventions. As part of that evaluation process, USC’s Center for Effective Organization has partnered with Alegent Health to assess the development and impact of its innovation capability (Worley, Mohrman, and Nevitt, 2011), describe its quality program, monitoring its sustainability efforts, and the on-going adaptation of its sustainability and care coordination and integration programs. The data on which this case study is based includes observations of meetings, large-group interventions, and other activities; site visits to different hospitals in the system to observe changes in practice; interviews with Alegent Health executives, primary care physicians, hospital presidents, specialist physicians and physician groups, and health systems staff and nurses; and a variety of archival data including meeting minutes, video tapes, conference proceedings, and website material. Correlating organization changes with improved outcomes is always difficult in case research; it is doubly difficult in with regard to healthcare outcomes. There are very few generally accepted and objectives measures, the databases are still being developed, and they have not been in place long. However, the Alegent case makes several claims regarding improved outcomes and the best data available are presented. THE EVOLUTION OF ALEGENT HEALTH 17 Alegent Health, like other healthcare systems in the U.S., has been responding to and taking proactive actions to meet the challenges of its industry and local market. The organization has envisioned and implemented a series of strategic initiatives that have driven or affected clinical outcomes, financial performance, community health, and environmental impact. Alegent’s evolution can be described in four phases, including 1) The development of an innovation capability and the institutionalization of decision accelerators as a method of change, learning, and decision making 2) The adaptation and integration of the medical staff, quality programs, and IT infrastructure 3) The emergence of a sustainability strategy and the development and implementation of the systems of care concept 4) Current challenges and adaptations to the economic crisis and healthcare reform Building an Innovation Capability In 2004, Alegent Health’s board of directors appointed a new CEO and provided a clear mandate for leadership. The most pressing issue was the repair of the distressed relationships with its attending physicians. The prior administration had alienated its non-employed physician community, and a public “no confidence” vote was played out in the local media. The physicians were concerned with the way Alegent was organized and operated. A clearly centralized decision making style resulted in service line VPs – the leaders of the women's and children's, cardiovascular, orthopedics, oncology, neurosciences, and behavioral health services – driving strategy and operations. Hospital vice-president/COOs lacked operational control and physicians 18 were alarmed by the inability to get things done with quality and in a timely manner. Alegent’s reputation in the broader Omaha area suffered. One of the CEO’s initial tasks was the development of a vision and values statement for the system. Using an inclusive process, the organization pegged itself to an aggressive “world class” standard. The vision and values in 2005 read: Vision Achieve world-class leadership in compassionate, faith-based health services that measurably enriches the lives of families we serve through an exceptional commitment to quality. Values create caring and compassionate environments respect the dignity of every person care for the resources entrusted to us as responsible stewards collaborate with others to improve the health of our communities attend especially to the needs of those who are poor and disadvantaged act with integrity in all endeavors In support of the vision and values, Alegent reorganized into a matrix structure that gave the hospital vice-president/COOs more control over their facilities. The service line vice presidents were charged with setting strategy and working with the hospitals to execute it. This structure is shown in Figure 2. 19 ----------------------------Figure 2 About Here ---------------------------A key feature of the structure was the Chief Innovation Officer (CIO) position. The CIO was charged with invigorating the service lines and learning to collaborate with the hospital presidents to increase innovation, lower costs, and improve quality. Two organization consultants introduced the CIO to “decision accelerators” (DAs) through site visits to organizations with innovative reputations. A DA is a type of large-group intervention (Shmulyian, Bateman, Philpott, and Gulri, 2010). It brings multiple stakeholders together over multiple days to address an organizational issue, and uses divergent and convergent decision-making processes to arrive at innovative solutions. Small multi-stakeholder teams work on a specific task, such as creating a vision or strategy, which is then presented to the large group and discussed. That “product” is then iterated based on different perspectives (e.g., stakeholders) and inputs (e.g., business and market expectations). This divergent/convergent process of “rapid prototyping” is one feature that distinguishes the DA from other large-group interventions. The CIO organized six initial DAs in July and August of 2005, one for each of the service lines. Each DA was to generate an innovative vision, core strategies, and high-level implementation milestones for that service line in pursuit of world-class healthcare. The DAs were an important intervention in the Alegent organization. Not only did they produce novel strategies for the services lines and a means for coordinating with the hospitals, they directly addressed the physician community’s concern over operational involvement. Between 27% and 20 47% of the participants in a DA were physicians from the respective specialty (Worley, Mohrman, and Nevitt, 2011). What began as an intervention to involve physicians in clinical planning eventually became an important capability in the system. Soon after the initial six DAs took place, additional DAs were convened and by March, 2007, Alegent had conducted more than 100 DAs. In addition, a particular vocabulary diffused throughout the system. People began to talk about “pulling up chairs to have a cross-functional conversation,” they engaged in “rapid prototyping” of ideas, and they reached out to people in other groups to build “social capital.” All of these terms were introduced as part of DA events. Over time, the organization developed the skills and knowledge to design, facilitate, deliver, and follow up on decision accelerator conferences; created a physical structure, language and vocabulary, and strategy for creating innovation in the system; and built up a body of experience on how to make the DAs most effective. Internalizing many of the DA’s processes gave Alegent a flexible decision-making platform and innovation capability. An important outcome of the original six DAs was a board request for $315 million dollars to remodel the hospitals to support the world class service line objectives. What became known as “Generation Patient” was a broad and systemic upgrading of the Alegent facilities that began in 2005 and was to be completed by 2012. The Development of a Quality Process and Technical Infrastructure The original six DAs and the innovation capability they spawned involved community representatives, patients, regulators, physicians and physician groups, and healthcare executives in a wide variety of the most critical issues facing the system. Two of the most important 21 initiatives that came out of these conversations – quality and technology – would become important pillars of Alegent’s sustainable design. While both quality and the electronic enablement of care had been on-going programs within Alegent, the DAs helped re-focus and reshape their purposes and implementations. On the quality side, at about the same time as the initial DAs were being implemented, Alegent’s board was asking the CEO, “How are we holding Alegent accountable for the quality of care we provide?” (Maas, 2008). The question generated important discussions at the board level, initiated a strategic planning effort, and resulted in “The Quality Revolution” strategy. As part of the plan, the board renamed the Professional Affairs Committee – which had been responsible for quality but spent most of its time on credentialing – to the Patient Safety and Quality Committee. Internally, and partly as a result of his experiences in the original DAs, the chief medical officer kicked off a revitalized quality effort with a 2½-day quality DA. Aligned with the clinical service line visions, it developed a list of the market and other environmental trends in quality to create an internal quality strategy. Then, the DA helped to support physicians in building a process and framework they could own to drive evidence-based care across the hospital system. The CMO took the DA results and realigned the medical staffs at the hospitals. At the time, there was no organized way to bring the different medical staffs together. Utilizing a “mirror organization” concept, each hospital medical staff used the same structure – a quality council composed of the chief medical director, vice chief medical director, and other physicians. The leaders of the hospital quality councils sat on a governance body – the Physicians Leadership Council (PLC) which reported directly to the board as part of the Quality Revolution strategy. Part of that governance process was a routine for developing “evidence-based” care 22 protocols that established clinical best practices and encouraged physicians to follow them. A DA in late 2007 helped to bring many of the physicians into early discussions and development of the protocols thereby increasing their commitment to the processes. The physician-led process quickly developed condition-specific processes for 30 clinical areas, including pneumonia, heart failure, and acute stroke. In the process of developing these protocols, the physicians reviewed and retired 208 existing protocols including 49 separate cardiac and 65 obstetric protocols that were consolidated into seven and four evidence-based protocols, respectively. Figures 3 and 4 summarize Alegent’s progress in clinical quality and patient satisfaction. Figure 3 shows an increasing quality trend from 2003 to 2006 using a composite score of 20 different measures. In 2007 and 2009, the data is a redefined and more comprehensive set of quality measures that permits comparison across both regional healthcare systems and a set of “world class” competitors but also reflects an increasing trend. In June, 2008, Alegent was recognized by the national Network for Regional Healthcare Improvement (NRHI) as the number one healthcare organization in terms of clinical/quality outcomes and patient satisfaction. Finally, Figure 4 shows small declines in two measures from the HCAHPS survey. -------------------------------Figures 3 and 4 about here --------------------------------On the technology side, an Alegent-Siemens Medical Solutions alliance was formed in 2002 to develop and implement an IT system that integrated the patient medical record, physician offices, and hospital administration. Throughout Alegent Health’s hospitals and 23 clinics, Siemens was to provide all of the health system’s new equipment needs for diagnostics, patient monitoring, patient records, and healthcare information technology (IT) systems, and in addition would digitally integrate patient data, medical, and diagnostic information. Like the quality initiative, Alegent’s technology initiative got an important bump from the innovation process. An interesting outcome from the original strategy DAs was a clear statement of the clinical service lines’ IT needs. Alegent and, more importantly, the IT function had never had an integrated needs assessment to inform its planning. Most of the IT focus in healthcare was on clinical issues and Alegent, like a few others, was working on electronic medical records and the related infrastructure. But the DAs identified a new and emerging set of issues. What the community and the service lines wanted was Web-based assistance to help patients navigate through the system of physicians, offices, and appointments and an easy way to get information about healthcare. The organization had to become a much more knowledgefriendly system. Based on that input, an initial DA to map out an overall strategy was convened. After that, a second, “deep dive” DA began by presenting the strategy and then turning to a discussion of how to implement it. Partners and vendors, such as Siemens, applications specialists, IT experts, and clinical representatives developed a three- year plan to support the service lines, the quality revolution strategy, and the health system interface to the community. One of the best outcomes from this effort was the creation of the “MyCost” tool. Found on Alegent’s website and first made available in early 2007, MyCost allows patients to obtain an estimate of actual costs they will incur for a specific test or procedures, along with an estimate of out-of-pocket expenses given their insurer’s plan. 24 Between 2005 and 2008, Alegent Health and its Senior VP of strategy and technology were recognized for the programs implemented through the Siemens alliance and the DA strategies, including awards from Healthcare Informatics (HCI) Magazine, the Advanced Information Management Institute, Health Imaging & IT's Top 25 Connected Facilities, and the American Hospital Association's Most Wired (and Wireless) Hospitals & Health Networks. The IT function continues to be at the forefront of the industry with the construction of a LEEDcertified data center in 2011, the decision to move ahead with the implementation of the stateof-the-art EPIC system, and the development of business intelligence applications (Howell, 2011). The Emergence of a Sustainability Strategy As many of the projects emanating from the initial DAs, generation patient, and the quality and IT initiatives were being put in place, Alegent’s CEO was becoming concerned about issues related to ecological sustainability and wanted to see Alegent move in this direction. As a part of its 2007 strategic planning review, Alegent’s Board also worried about the ecological aspects of healthcare. In particular, two of their values – caring for resources as responsible stewards and collaborating with the community to improve health - influenced them to consider their ecological impact and how the delivery of care reflected these values. Benchmark research and a preliminary assessment of Alegent’s impact on the environment, led the CEO and the Chair of the Board’s planning committee to appoint a VP of Sustainability to develop and implement an integrated sustainability strategy. Based on his experience with the DAs in setting vision and strategy, guiding implementation, and driving consensus and buy in across a range of stakeholder interests, the VP 25 convened a sustainability DA. In collaboration with the Sustainability Leadership Institute, 63 people representing the healthcare system (executives, physicians, and operations), corporations (Baxter Healthcare, Portion Pac Chemical Corp), NGOs (Sustainability Leadership Institute, Omaha by Design), government (Omaha Chamber of Commerce), and academia (University of Nebraska, Omaha) met in February 2008. In support of a 20-year vision, the DA developed six “planks” of activity to address issues in the value chain (upstream and downstream), transportation, facilities, internal culture, and community/partnerships. In May, 2008, a second DA was conducted to put “meat on the bones, clarify action, and take it to the next level.” On the first day, key executives and operations leaders went through a “consistency check” to fill in some of the blanks in the action plan. On the second day, many of the same stakeholders who participated in the first DA returned to respond to the action plans and develop additional recommendations. In particular, the group recommended addressing the “low hanging fruit” as a way to build awareness and momentum for sustainability in the organization. This included recycling efforts, setting up systems for duplex printing, working with facilities to develop energy protocols, and so on. The group also suggested implementing more systemic programs and projects on a pilot basis. One of the hospital presidents volunteered and work began on that effort. Thanks to the DA and the organization’s innovation capability, Alegent was able to move to a fully vetted sustainability strategy and plan in five months. Dubbed “Eco-Alegent,” a 1, 3, and 5-year sustainability vision and planning milestones, a pilot program at one of the hospitals (another hospital that just couldn’t wait for the initial pilot results also joined in), and a variety of other projects were created. The “other” projects included a program to reduce “red bag waste,” manage water and power usage in all Alegent facilities, lease 50 Toyota Prius’s to support the 26 home health initiative, work with government transportation agencies to create bike and trail paths and alter bus routes for employees, and involve physicians and a major healthcare supplier to change packaging. Sustainable Healthcare Delivery - The Systems of Care Model In response to a variety of forces that were operating in the healthcare industry around 2008 and 2009, including scarcity of qualified human resources, increasing costs, decreasing reimbursements, and increasing demand for consumer value, Alegent began to think about how it might change the delivery of care. With the development of its innovation capability, Alegent had proactively responded to these forces by consolidating its complex cardiovascular surgeries to one location; integrating its laboratories, sleep centers, and food services; and reinventing the Alegent Health Clinic organization – a multi-specialty network of more than 200 medical providers offering primary and specialty care at over 50 locations. But Alegent management also believed a more comprehensive model was needed to organize and align the efforts of the multiple stakeholders involved. As depicted in Figure 5, Alegent characterized traditional healthcare delivery as one of “transactions of care.” Under this model, there was a clear “location focus” where patients were seen at different places and at times that were convenient for the healthcare provider. Information about the patient’s past health, treatments, or lab results was fragmented and resulted in duplicate tests, wasted time, and increased costs. Instead, Alegent started to think in terms of “systems of care.” This forward thinking model represented a healthcare business model that could deliver better outcomes by efficiently 27 coordinating patient information and patient needs, clinical decisions, and operations through owned, affiliated, and virtual sites of care. ---------------------Figure 5 about here -----------------------In a systems of care model, certain tertiary care specialties, like cardiovascular surgery, neurology, and high-risk pediatrics, might be focused in a single hospital to increase volume and optimize quality. Secondary specialties, such as cardiology, obstetrics, oncology, or orthopedic surgery, would be housed in a few sites but with access on demand virtually or via transfer across the system. Finally, a core set of hospital departments (e.g., emergency, radiology), services (e.g., general surgery), or facilities (e.g., inpatient beds, catering) would be available in every hospital. Such a system of care would excel at physician, clinical, and information integration. Value would be created by providing timely access to care, lowering costs, and demonstrating the ability to measure and deliver superior clinical outcomes, patient engagement, loyalty and financial stewardship - the very values that Alegent espoused. Alegent’s experience with innovation and change led them to specify the success factors necessary to lead and operate this model. They included: Leadership with both horizontal and vertical integration – triad leadership between nurses, administration, and physicians Cultural changes – different focus with new acceptable norms Access to information, at the right time, in the right way Seamless coordination and handoffs 28 Continuously engaged individuals providing and receiving services Expanded continuum with new / improved nodes / models of care Shared risk / aligned incentives Demonstrated meaningful outcomes that exceed expectations Global brand / identity Alegent Health began to implement some elements of the systems of care concept by reorganizing to emphasize the role of the Alegent Health Clinics organization, creating a shared leadership model where a hospital vice-president/COO and medical director team worked together to implement quality at the hospital on a day-to-day basis but to also coordinate care by establishing standards across the system for a particular service line. (See Figure 6 for a modified picture of this structure.) Alegent Health Clinic’s “patient-centered medical home” pilot project demonstrated how the systems of care concept could be implemented. The Patient-Centered Medical Home builds a partnership between patients and their primary care physicians - and when appropriate - the patient’s family. A care team, led by a primary care physician and featuring care coordinators, physician assistants, certified medical assistants, and other specialists as needed, represents the patient’s “home.” The care team provides patients with the individual care they need and coordinates treatments across the system. Initially, the clinic physicians identified three different disease processes - diabetes, hypertension and dyslipidemia – they believed could be managed proactively and lead to fewer hospitalizations and fewer medications. 29 Four primary care physicians and three physician assistants at a clinic use group visits to help those patients who have been diagnosed with one of these chronic illnesses. The physicianled clinic teams meet every morning to go over the day’s schedule. They look at preventive care opportunities, labs that need to be done, and any other services that will be needed during the visit. A group of 6-10 patients, dieticians, physical therapists, and pharmacists meet and share their lab and other results, such as weight, BMI and blood pressure. The visits include a regular medical office visit. The patients see that they are not alone in their disease process, get encouragement from the other patients, and support from their medical team. The pilot program showed improved care quality and the potential to lower healthcare costs by increasing access to more efficient, coordinated care. By avoiding unnecessary hospitalizations and emergency room visits, these early results can produce savings for patients. The National Committee for Quality Assurance (NCQA) granted Alegent Health Clinic’s medical home program the highest Level 3 recognition – after the Clinic scored 95.25 out of a possible 100 points. Current Challenges and Adaptations to Economic Crises and Healthcare Reform Both the Eco-Alegent initiative and the systems of care model were sidetracked to some extent by the economic recession of 2008-2010. When the cost of capital increased, when capital itself became unavailable, and when hospital utilization decreased, the health system faced some tough choices. Eventually, there was a round of layoffs, the non-employed physician community became upset, and CEO who had led the transformation and five other members of the executive team resigned. 30 For the sustainability program, the effort remains alive and well at the local level. Hospital, headquarters, and other support facilities have implemented “green teams” to identify and address local issues but there has been less progress on the broader planks of the strategy. For the systems of care, Alegent took a step back to think about rebuilding trust with the physicians. As conversations began, the focus was on managing chronic disease and what it meant to be clinically integrated. The systems of care model – developed collaboratively but implemented in a mostly top down fashion – had an implicit logic that suggested which tertiary care services would make good candidates for centralization. Rather than prescribing how to implement the changes, the system is trying to work more collaboratively with the medical staff to become more integrated and less fragmented. The DA process continues to serve and support the health system in this regard. A recent DA focused on developing a care coordination capability. About 70 people, representing physician specialists, primary care physicians, nurses, and other stakeholders explored the pockets of care coordination that were already happening internally, like the patient-centered medical home project above, as well as some external examples. These were used to build design criteria and a care coordination capability vision. Based on those criteria and vision, the capability was decomposed into a number of “functionalities” or core, repeatable processes with a team formed around each one. For example, one team was formed around creating a “seamless patient experience” to look at how handoffs occur among and between the primary care, home, and hospital environments. Each team was tasked with coming back to the large group with metrics and critical success factors for each functionality after 30 days. In the next meeting, the team explored where 31 processes experience problems, breakdowns, or bottlenecks and then reconfigured the teams to look at those issues. Similarly, the organization continues to evolve its structure to support an integrated model. A modified version of the Alegent Health leadership structure is shown in Figure 7 to reflect the organization’s current operations and show how its integrated delivery model is reflected in the shared leadership of hospitals and service lines. The hospital COOs and Campus Chief Quality Officers (CCQO) share in the operation of a respective hospital and service line, although Alegent has recently clarified those roles. The physician leader is primarily focused on quality and patient safety at a facility. In Figure 6, those roles have been differentiated to visualize the cross-facility and cross-business unit coordination that takes place in support of clinical and operational integration. ------------------------------Figure 6 about here ------------------------------- As shown, Alegent uses the following lateral mechanisms to coordinate care: • The healthcare system’s Senior VP/COO, the Senior VP/CQO, the VP/Chief Nursing Officer, the Hospital COOs, and CCQOs are the team ultimately accountable for the coordination of care. The team sets operational policy, makes resource allocation/tradeoff decisions regarding care delivery within health system (i.e., resolves any conflicts and sets priorities among and between the “hospital” team and the different “service line” teams). 32 • The “hospital” team is composed of the hospital COOs and the CCQOs. It shares clinical, facility, and administration best practices, including how to drive behavior and culture change in the facility and the adoption of environmental practices from the “green teams.” It interfaces with the “service line teams” to understand each hospital’s role in that specialty and ensure that the facility is ready to deliver. It also interfaces with Alegent Health Clinic to ensure seamless relationships (e.g., handoffs, privacy, transportation, communication, etc.) between the clinics, the community, and the hospitals. • The “service line” teams are chaired by the respective hospital COO and made up of physicians and clinical staff from other hospitals. The CCQO may work on the service line team if it represents his or her particular medical specialty. The service line teams are charged with the where, when, how, and why of care within that service line. For example, the team determines evidence based care pathways, how they will interact with primary care physicians, and where the service is best delivered (hospital, home, clinic, office). This includes working with the Alegent Health Clinic to ensure seamless relationships (e.g., handoffs, privacy, transportation, communication, etc.) between the clinics, the community, and the hospitals. The team is also responsible for monitoring physician behavior and coaching them toward quality. Finally, the service line team must also coordinate with the IT organization to maintain databases and connectivity, coordinate with other service lines/specialties, set standards of care, and monitor quality measures (and interfaces with health system quality office). 33 Over the past seven years, Alegent Health has demonstrated the ability to change and redesign itself along multiple dimensions. In implementing change, it has improved quality, leveraged technology, supported its community, and addressed its environmental footprint. Alegent’s journey has occurred at a time when the healthcare environment – in all its aspects – has been shifting and changing. Its change, learning, and innovation capability – as manifest in the DA – has been the foundation that enabled it to continuously reconfigure and introduce new approaches to achieve more sustainable functioning. DISCUSSION An agile healthcare system is a combination of flexible organization features – structures, care delivery processes, leadership, and decision-making systems – and the ability to change the configuration of those features over and over again. Alegent Health’s evolution, seen in the context of a volatile healthcare environment and sustainability, is an important demonstration of what is possible. This section distills and draws out two key learnings: (1) agility is built by addressing all of the parts and (2) agility is a journey that can be pursued sequentially. Alegent’s claim to agility is supported by a wide variety of design features and organization changes. Table 2 reproduces the agility design features and summarizes Alegent’s history, capabilities, and accomplishments with respect to those features, ----------------------Table 2 about here 34 ------------------------ The board supported sustainable effectiveness. It was board level decisions that ushered in a new CEO, visioning process, and innovation effort; kicked off the Quality Revolution strategy; initiated the sustainability strategy; and supported the system of care process. Alegent’s long-term identity supported its short-term strategic intents. Alegent Health’s identity is rooted in an image and corporate values that have not changed much over time. In addition to its faith-based mission, its values consistently focus on patients, the community, and quality, and its value of stewardship has been broadly interpreted to imply that the organization should work toward sustainable outcomes. Although its reputation has varied a little - its relationship with non-employed physicians has been up and down over the years – Alegent continues to be proactive in working with the community (e.g., it offers the DA facility to host community events and discussions, sponsors local events, and supports volunteer efforts) and continues to solicit feedback from the community about its operations. It has projected and lived up to a consistent image. In addition, each of Alegent’s initiatives or intents responded to pressures in the environment and built a more agile and sustainable healthcare system. The sequence involved (1) becoming more innovative and world class, (2) driving quality and technical excellence, (3) engaging with sustainability, and (4) building an integrated system of care. Each intent was consistent with Alegent’s overall identity. Alegent’s design features – structure, coordination, and work system – support continuous re-alignment. Alegent’s two reorganizations – first to a matrix and then to a 35 strong functional organization with lateral teams – increased the surface area of the organization. The matrix structure increased the hospital vice-president/COOs’ exposure to their environments, including more control over operations, quality, and physician relations. Similarly, the structure supporting the systems of care elevated and exposed the clinics to broader strategic issues, and gave the hospital and physician managers more exposure to clinical and administrative issues across the system. Alegent has leveraged a variety of lateral routines. Its long-term relationships with Siemens resulted in state-of-the-art electronic coordination systems. The matrix structure legitimized service line/hospital integration and coordination, quality councils and a physician leadership council supported the quality revolution strategy, and governance groups help to coordinate care, service line teams, and hospital teams in the latest structure. The DA must be recognized for its role in this regard. It represents a very flexible method for coordinating work, decisions, strategy, and action. It represents a deep capability for pulling together multiple stakeholders, both internal and external, to explore a variety of issues. In addition, the processes surrounding the DA, including identifying critical issues to address, designing and delivering the DA event, and following through on decisions made, has become an effective and integrated adjunct to traditional healthcare system work. While the hospitals perform the day-to-day services that must meet reliability and quality standards, the broader DA capability provides a flexible method for exploring, designing, and implementing innovations. The uneven implementation of the system of care concept can be interpreted as further support for the importance of the DA capability. Part of the physicians’ resistance 36 was a perception that it was being driven outside the DA process. The concept was developed collaboratively, but implementation was more top-down. That Alegent has reengaged the physicians using the DA to address clinical integration may be an acknowledgement of its acceptance as a way of doing business within the system, and the dangers of straying from a participative model of decision making. A shared leadership philosophy is manifest in the structure. By having administrative (hospital COOs) and clinical (physicians) positions responsible for both operations and clinical integration, they have designed in a model where the difficult tensions of administration and clinical issues can be seen and managed collaboratively. However, there is little evidence of performance management changes and that represents a potential area for Alegent to explore in building out its agile capabilities. The DA has become a powerful change and learning mechanism. The centerpiece of the Alegent case is clearly the decision accelerator – a robust routine for change, learning, and innovation. As a decision making, innovation generation, and strategy tool, it has served the organization in a variety of capacities. But as a core component of a broader and more fundamental change and learning capability, the DA has served as a vehicle supporting Alegent’s agility. The ability of the DA process to drive change and learning derives, first, from its ability to formalize the most important but informal aspects of relationships among stakeholders. This is often referred to as “social capital.” A physician requests and is granted privileges at a hospital, and those privileges are detailed in a contract. But on a day-to-day basis, the physician has to interact with a number of ever-changing people occupying nursing, administration, billing, radiology, pharmacy services and other roles 37 in the system. These people and relationships are not specified in contracts or formal policy and procedure documents. That coordination does not “just happen.” The DA builds this “social capital” by creating relationships among people. Sustainability, whether it is in service of clinical, social, or ecological outcomes, is supported by the clarification and enrichment of these relationships and interactions. If everyone associated with patient care agrees that decreasing toxic waste is important but everyone assumes someone else will worry about it, it doesn’t happen. The DA process is a powerful way to support this learning. The DA was also a powerful change and learning mechanism in this case because it represented an important, robust, and central design intervention. Why did the Quality Revolution get implemented so quickly and so well? Certainly, the board’s support had something to do with it, but what would have happened if Alegent Health had implemented the DA and innovation capability process at a later point in time? It is, of course, a speculative question, but an important one. If the DA had not been the first intervention, the way change unfolded at Alegent would have been very different. The quality initiative, electronic medical record implementation, and service line changes probably would have been handled in more traditional ways. The DA was powerful because it enabled the effectiveness of every change that came after it. Most of the issues addressed by the DA/innovation capability – quality, clinical strategies, and cost reduction – are part of any hospital’s operations. But they got addressed in Alegent quickly and comprehensively by all of the stakeholders. Building a change and learning capability first not only jump-started the transformation at Alegent, it provided an important accelerator for change. 38 The above point highlights a second learning from the Alegent Health case. The development of an agile capability is a journey, one that is never finished. An organization that has survived over a relatively long period of time has to possess some level of agility, but it can always become more agile. Part of Alegent’s success is explained by the way they went about changing. Although they changed a great many features, they did not try to change everything all at once. They faced each challenge and opportunity as a way to build on prior successes. That does not mean there was not a lot of change going on, only that the changes were linked together. The amount of change facing healthcare organizations is tremendous, and systems can become overwhelmed with too much change all at once. It may be convenient (and accurate) to describe Alegent’s changes as sequential, but in all cases the changes overlapped. For example, the DA and innovation capabilities continue to develop to this day even though they may have been the “first” changes. Similarly, installing a uniform quality approach across a system that was used to considerable autonomy prior to the CEO change, and then attempting to optimize the care delivery system is not only a large change but a complex and continuing one. Administrators must balance the speed of change with the recognition that each change can make a unique contribution to sustainable effectiveness. Avoiding the perception that “everything is changing all at once” can be mitigated by ensuring that each change builds on another and setting the expectation that change will never be over. The comments about the DA’s power as a change and learning mechanism and it being the “first” intervention raises an interesting suggestion for future research. It would worth exploring the role of “initial initiatives.” Can successful large-scale change or the development of an agile capability in healthcare or other industries be influenced by that choice of “what gets 39 implemented first?” The Alegent case suggests that good candidates for an initial initiative are not related to specific functional targets (e.g., quality, ERP implementation) but to processes, routines, and capabilities that can integrate and accelerate organization change and learning. CONCLUSION Healthcare reform is only one aspect of a turbulent and uncertain environment facing hospital systems in the U.S.. It is an environment that is unlikely to become anywhere near stable for a long time, if ever. Interpreting the political processes intended to “bend the cost curve” for the best way to organize is an important element of environmental scanning, but is also probably futile. Other countries or regulatory frameworks are likely to be facing their own version of disruption and change. A better approach is to design a healthcare system that is able to change strategies, reconfigure its structures and work processes, and conceive of and implement innovation on a routine basis. Whatever changes come, an agile healthcare system can adapt to them. The Alegent case supports the conclusion that sustainable healthcare systems must be agile. In fact, it would be hard to conceive of a sustainable system that wasn’t agile. Alegent Health, armed with the robust DA routine, is in a great position to identify, innovate, and implement change as required by an uncertain and complex environment. Such a capability will support their pursuit of accountable care and drive clinical, financial, community, and ecological improvements. Building an organization around the characteristics of agility has prepared Alegent for healthcare reform and any number of other challenges it will face. Their successes and challenges can serve as a model for other healthcare systems. 40 REFERENCES American Health Association. (2010). AHA white paper on clinical integration. Retrieved on February 5, 2012 from http://www.aha.org/content/00-10/070417clinicalintegration.pdf. Bader, J. (2009). Clinically integrated physician-hospital organizations. Great Boards, 9(4), 112. Beer, M. (2009). High commitment high performance: How to build a resilient organization for sustained advantage. San Francisco: Jossey-Bass. Beer, M., Fredberg, T., & Foote, N. (2011). Higher ambition: How great leaders create economic and social value. Cambridge, MA: Harvard Business Review Press. Blumenthal, D. (2009). Stimulating the adoption of health information technology. New England Journal of Medicine 360(15), 1477-1479. Bodenheimer, T., Wang, M., Rundall, T., Shortell, S., Gillies, R., Oswald, N., Casalino, L., & Robinson, J. (2004). What are the facilitators and barriers in physician organizations' use of care management processes?” Joint Commission Journal on Quality and Patient Safety, 30(9), 505-514. Casalino, L., Gillies, R., Shortell, S., Schmittdiel, J., Bodenheimer, T., Robinson, J., Rundall, T., Oswald, N., Schauffler, H., & Wang, M. (2008). External incentives, information technology and organized processes to improve health care quality for patients with chronic diseases. Journal of the American Medical Association, 289(4), 434-441. Center for Medicare and Medicaid Services (CMS). (2011). Retrieved February 6, 2012 from https://www.cms.gov/ACO/. 41 Clark, D., Savitz, L. & Pingree, S. (2010). Cost cutting in health systems without compromising quality care. Frontiers of Health Service Management, 27(2),19-30. Conger, J. (Ed.). (2009). Boardroom realities: Building leaders across your board. (San Francisco: Jossey-Bass. Cummings, T., & Worley, C. (2009). Organization development and change (9th ed.). Mason, OH: Southwestern College Publishing. Deloitte Center for Health Solutions. (2010). Accountable care organizations: A new model for sustainable innovation. Retrieved February 6, 2012 from http://www.deloitte.com/assets/DcomUnitedStates/Local%20Assets/Documents/US_CHS_AccountableCareOrganizations_070 610.pdf Devers, K., & Berenson, R. (2009). Can accountable care organizations improve the value of health care by solving the cost and quality quandaries? Urban Institute. Retrieved January 15, 2012 from http://www.urban.org/publications/411979.html Dukerich, J., Golden, B., & Shortell, S. (2002). Beauty is in the eye of the beholder: The impact of organizational identification, identity, and image on the cooperative behaviors of physicians. Administrative Science Quarterly 47, 507-533. Fredberg, T., Norrgren, F., & Shani, A. (2011). Developing and sustaining change capability via learning mechanisms: A longitudinal perspective on transformation. In: W. Pasmore, A. Shani, & R. Woodman (Eds.), Research in organizational change and development (Vol. 19, pp. 117-161). Howard House, UK: Emerald Publishing. Galbraith, J. R. (1993). Competing with flexible lateral organizations (2nd ed.). Reading, MA: Addison-Wesley. 42 Galbraith, J. R. (1994). Designing organizations: An executive briefing on strategy, structure and process. San Francisco: Jossey-Bass. Galbraith, J. R. (2005). Designing the customer-centric organization. San Francisco: JosseyBass. Gillies, R., Shortell, S., Anderson, D. Mitchell, J., & Morgan, K. (1993). Conceptualizing and measuring integration: Finding from the Health Systems Integration Study. Hospital and Health Services Administration, 38(4), 467-489. Goldman, S., & Graham, C. (Eds.). (1999). Agility in health care: Strategies for mastering turbulent markets. San Francisco: Jossey-Bass. Haeckel, S. (1999). Adaptive enterprise: Creating and leading sense-and-respond organizations. Boston: Harvard Business School Press. Hanna, D. (1988). Designing organizations for high performance. Reading, MA: AddisonWesley. Hoffman, A. J. (2010). Climate change as a cultural and behavioral issue: Addressing barriers and implementing solutions. Organizational Dynamics, 39(4), 295-305. Howell, W. (2011). Business intelligence: Key to hospital’s sustained success. Retrieved January 24, 2012 from http://www.porterresearch.com/Resource_Center/Blog_News/Industry_News/2011/Augu st/Business_Intelligencex_Key_to_a_Hospitalxs_Continued_Success.html Lawler, E.E. (1986). High-involvement management. San Francisco: Jossey-Bass. Lawler, E.E., & Worley, C. (2006). Built to change. San Francisco: Jossey-Bass. Lawler, E.E., & Worley, C. (2011). Management reset: Organizing for sustainable effectiveness. San Francisco: Jossey-Bass. 43 Lawrence, P., & Lorsch, J. (1967). Organization and environment. Cambridge, MA: Harvard Business School Press. Lorsch, J., & MacIver, E. (1989). Pawns or potentates: The reality of America’s corporate boards. Boston: Harvard Business School Press. Maas, D. (2008, May). Assuming quality leadership. Trustee, 17-20. Medicare Payment Advisory Commission. (2007). Assessing alternatives to the sustainable growth rate system. Retrieved February 8, 2012 from http://www.medpac.gov/documents/Mar07_SGR_mandated_report.pdf Mehrotra, A., Epstein, A., & Rosenthal, M. (2006). Do integrated medical groups provide higher quality medical care than IPAs. Annals of Internal Medicine, 145(11), 826-833. Meyer, H. (2011). Accountable care organization prototypes: Winners and losers? Health Affairs, 30(7), 1227-1231. Miles, R., Snow, C., Fjeldstad, O., Miles, G., & Lettl, C. (2010). Designing organizations to meet 21st-century opportunities and challenges. Organizational Dynamics, 39(2), 93-103. Mirvis, P. H., & Googins, B. (2006). Stages of corporate citizenship: A developmental framework. California Management Review, 48, 2, 104-126. Mirvis, P. H, Googins, B., & Kinnicutt, S. (2010). Vision, mission, values: Guideposts to sustainability. Organizational Dynamics, 39(4), 316-324. Mohrman, S. A. & Worley, C. G. (2009). Dealing with rough times: A capabilities development approach to surviving and thriving. Human Resource Management, 48(3): 433-445. Mohrman, S. A., & Cummings, T. G. (1989). Self-designing organizations: Learning how to create high performance. Reading: Addison-Wesley. Nadler, D., & Tushman, M. (1997). Competing by design. New York: Oxford University Press. 44 Rittenhouse, D., Shortell, S., Gillies, R., Casalino, L., Robinson, J. McCurdy, R., & Siddique, J.. (2010). Improving chronic illness care: Findings from a national study of care management processes in large physician practices. Medical Care Research and Review, 67(3), 301-320. Rumelt, R. (1974). Strategy, structure, and economic performance. Cambridge, MA: Harvard Business School Press. Shortell, S., & McCurdy, R. (2010). Integrated health systems. Studies in Health Technology and Informatics, 153, 369-382. Shmulyian, S., Bateman, B., Philpott, R., & Gulri, N. (2010). Art or artist? An analysis of eight large-group methods for driving large-scale change. In: W. Pasmore, A. Shani, & R. Woodman (Eds.), Research in organizational change and development (Vol. 18, pp. 183232). Staw, B. (1976). Knee-deep in the big muddy: A study of escalating commitment to a chosen course of action. Organizational Behavior and Human Performance, 16, 27-44. Sterns, J. (2007). Quality, efficiency, and organizational structure. Journal of Health Care Finance, 37(1), 100-107. Sull, D. (2008). The upside of turbulence. New York: HarperBusiness. Tushman, M., & O’Reilly, C. (1996) Ambidextrous organizations: Managing evolutionary and revolutionary change, California Management Review, 38, 8-30. Volberda, H. (1998). Building the flexible firm: How to remain competitive. New York: Oxford University Press. Williams, T., Worley, C., Canner, N., & Lawler, E. (2012). Sustained high performance and the role of agility. White Paper, Center for Effective Organizations, Los Angeles, CA. 45 Worley, C. (2010). On the road to corporate responsibility: The institutionalization of sustainability at Gap, Inc. In: S. Mohrman, A. Shani, & P. Docherty, Organizing for sustainable effectiveness (Vol. 1, pp. 73-97). Worley, C., Cummings, T., & Mobley, F. (2000). The dynamics of strategic change in hospitals: Managed care strategies, organization design, and performance. Public Administration and Management: An Interactive Journal 5. Retrieved from http://www.pamij.com Worley, C., Feyerherm, A., & Knudsen, D. (2010). Building a collaboration capability for sustainability: How Gap Inc. is creating and leveraging a strategic asset. Organizational Dynamics. 39(4), 325-334. Worley, C., & Lawler, E. (2009). Building a change capability at Capital One Financial. Organizational Dynamics, 38(4), 245-251. Worley, C., Mohrman, S. A., & Nevitt, J. (2011). Large group interventions: An empirical field study of their composition, process, and outcomes. Journal of Applied Behavioral Science, 47(4), 404-431. 46 Table 1 Design Features of an Agile, Sustainable Organization Design Feature Board Composition and Purpose Clear Long-term and Short-term Strategies Flexible Structure, Lateral Coordination, and Ambidextrous Work System Talent and Performance Management Change and Learning Capabilities Description Supporting Sustainability Board members that represent an organization’s multiple stakeholders and the information required to balance outcomes across those stakeholder demands A sustainability-oriented and change-friendly identity consisting of internal values and an external brand/image/reputation that explains long term success and a triple bottom line objective Short-term strategic intents that describe how the organization will win – across financial, social, and environmental outcomes - in the current environment A structural form that places organization members in contact with the environment and results in a strong external focus A flexible, lateral decision making, operating, and resource allocation process The ability to support both traditional and innovative work designs A philosophy and practice of shared leadership reinforced by performance management systems that measure and reward sustainable activities The ability to implement organization change, especially the transition from one strategic intent to another, and the ability to apply past learnings to current operations. 47 Table 2 Alegent Health and Sustainable, Accountable Design Criteria Agility Feature Board composition and purpose Clear long-term and short-term strategy Flexible structure, lateral coordination, and ambidextrous work systems Talent and performance management Change and learning capability Description, Activity, and Outcome Heavy board involvement in innovation (Board involvement in DA and commitment to Generation Patient), quality (Quality Revolution) and sustainability (Board initiation) Alegent’s identity reflects a strong change-friendly but a stronger sustainability-oriented orientation. Corporate values have changed very little over time, staying true to faith-based mission, stewardship (which has been interpreted to support environmental outcomes) Reputation/Brand – quality awards, recognition, community involvement A series of strategic intents : Innovation – Quality – Sustainability – Systems of Care Two reorganizations – first to a matrix and then to a shared leadership/strong functional organization with heavy use of lateral teams The DA represents a robust organization feature that supports work ambidexterity, flexible decision-making, and resourceallocation process Internal and external collaborations can be carried out through the DA and innovation capability to work on specific issues Shared leadership – physician/manager team Little evidence of performance management innovation The DA serves an important role in generating and managing change 48 Figure 1 A Taxonomy of Lateral Coordinating Mechanisms 49 Figure 3 Alegent Health’s Composite Quality Scores* between 2003 and 2009 100% Composite Score 90% 80% Alegent Regional 70% World Class 60% 50% 2003 2004 2005 2006 2007 2009 * Between 2003 and 2006, the composite quality score consists of a weighted average of 20 measures. For 2007 and 2009, the composite quality score is a weighted average of the acute myocardial infarction (AMI) score, the heart failure (HF) score, pneumonia (PN) composite score, and the surgical care improvement project (SCIP) composite score. The world class average includes: Johns Hopkins, Rochester Methodist (Mayo Clinic), St. Mary’s (Mayo Clinic), Mass General, UCLA Med Center, Barnes Jewish Hospital, New York Presbyterian, Duke University, and Cleveland Clinic. 50 Figure 4 Comparative Patient Satisfaction Scores for Alegent Health between 2007 and 2009 Percentage of Patients Giving Hospital a 9 or 10 Rating, 100% 90% 80% 2007 70% 2009 60% 50% Alegent Health System Regional Competitor Average World Class Average Percentage of Patients Willing to Recommend Hospital 100% 90% 80% 2007 2009 70% 60% Alegent Health System Regional Competitor Average World Class Average The data are from the Hospital Consumer Assessment of Healthcare Providers and Systems (HCAHPS) measures: http://www.hcahpsonline.org/home.aspx 51 Figure 5 Systems of Care Model 52 Figure 2. Alegent Structure ~2007 CEO CMO Technology Chief Innovation Officer Right Track HR CFO Chief Operations Officer Mercy Cardiology Oncology Orthopedics Women & Children Behavioral Health 53 Midland Bergen Lakeside Immanuel CEO Figure 6. Alegent Health Structure ~2011 Strategy & Technology Chief Financial Officer COO Chief Quality Officer General Counsel Alegent Health Clinic Chief Nursing Officer Hospital COO Campus CQO Hospital COO Campus CQO Hospital COO Campus CQO Hospital COO Oncology (Led by Service Line MD) Cardiology (Led by Specialist MD) Other Service Lines (Led by Appropriate MD) 54 Campus CQO Hospital COO Campus CQO 55